Sandbox:FB
Overview
Eosinophilic gastroenteritis (EG) is a rare disorder characterized by localized patchy or diffuse eosinophilic infiltration of the gastrointestinal (GI) tissue. The presentation may vary depending on the location, depth and extent of bowel wall involvement. It usually runs a chronic relapsing course.[1][2][3]
Historical Perspective
The first description of eosinophilic gastroenteritis was by Kaijser et al. in 1937, and it was described as an allergic disease of the gut.[4][5] Klein et al. subsequently classified it into three types (predominant mucosal, muscular, and subserosal layer disease) based on the depth of eosinophilic infiltration.[6]
Classification
Eosinophilic gastroenteritis can be subdivided into three groups according to the Klein classification:[7][8][9]
- Mucosal eosinophilic gastroenteritis
- Most common subtype of eosinophilic gastroenteritis.
- Mucosal infiltration by eosinophils, and/or presence of mucosal edema on barium studies.
- Absent histological evidence of muscle infiltration.
- No evidence of gastrointestinal obstruction or eosinophilic ascites.
- Muscular eosinophilic gastroenteritis
- Documentation of complete/incomplete bowel obstruction, and/or infiltration of the tunica muscularis by eosinophils.
- No evidence of eosinophilic ascites.
- Subserosal eosinophilic gastroenteritis
- Eosinophilic infiltration of the gut
- Eosinophilic ascites is present
Risk Factors
- Allergy: A study conducted in 40 patients with eosinophilic gastroenteritis demonstrated a history of allergy in half of the patients.[7] Food intolerance or allergy is more commonly seen in mucosal eosinophilic gastroenteritis, affecting over 50% of patients with mucosal disease according to a study.[7]
Pathophysiology
Pathogenesis
- Eosinophilic gastroenteritis is a rare disease with poorly understood pathophysiology.
- Eosinophils are normally seen in the entire GIT (except in the esophagus) of healthy individuals.[3]
- In patients with eosinophilic gastroenteritis, there is varying degrees of increased eosinophilic infiltration of the GIT (in the absence of other known causes of tissue eosinophilia).[5][3]
- Any part of the GIT from the esophagus to the colon can be affected. Occasionally, eosinophilic gastroenteritis affects the entire gastrointestinal tract.[7] The stomach and proximal small intestine are most commonly affected, while the colon is usually the least affected part of the GIT.[5][7][3]
- The etiology of the excessive eosinophilic infiltration of the GIT is not clear. Destruction of the GIT epithelium caused by the release of eosinophilic basic protein and activated degranulating eosinophils has been proposed.[7][10]
- Inflammatory mediators such as Th-2 cytokines (IL-3, IL-5 and IL-13), eosinophils, and eosinophilic mediators such as eotaxin have been strongly implicated.[5][3][8]
- The inflammatory mediators associated with the pathogenesis of eosinophilic gastroenteritis have well established roles in the pathogenesis of allergy and asthma. A significant number of patients with eosinophilic gastroenteritis have also been documented to have allergies/allergy-related disorders, suggesting a hypersensitivity reaction is involved in the pathogenesis of eosinophilic gastroenteritis.[5][8]
Causes
The cause of eosinophilic gastroenteritis is unknown.[8]
Differentiating Sandbox:FB from Other Diseases
Diseases with peripheral eosinophilia and gastrointestinal symptoms should be differentiated from eosinophilic gastroenteritis. It is also important to consider eosinophilic gastroenteritis in the differential diagnosis of unexplained gastrointestinal symptoms (even when peripheral eosinophilia is not present). Most diseases that can manifest with gastrointestinal symptoms and peripheral eosinophilia are easily differentiated from eosinophilic gastroenteritis via detailed history taking, laboratory investigations, and histologic examination of endoscopic biopsies.[8][3] Some of these diseases include:[8][3]
- Intestinal parasitic infections: Stool examination for ova and parasites can be utilized for diagnosis.
- Inflammatory bowel disease (IBD): Biopsy can easily ddistinguish IBD from eosinophilic gastroenteritis.
- Hypereosinophilic syndrome: It usually presents with markedly elevated peripheral eosinophilia (>1500 cells/μL) for more than six consecutive months. The organs that are commonly affected in hypereosinophilic syndrome are the lungs, skin, GIT, kidneys, heart and brain.
- Helicobacter pylori infecton: This is not a common cause of tissue eosinophilia. Histology of gastric biopsies using silver staining can rule out Helicobacter pylori infection.
- Vasculitic disorders such as churg-Strauss syndrome and polyarteritis nodosa: Eosinophilic infiltration of small blood vessels in the GIT is seen. Autoantibodies are present and markers of inflammation are elevated.
- Connective tissue disorders such as scleroderma and dermatomyositis
- Celiac disease
- Drugs: Some medications have been documented to cause eosinophilic infiltration of the GIT. Examples of such medications include gold compounds, rifampicin, clofazimine, gemfibrozil, azathioprine, enalapril, naproxen and other NSAIDS, interferon, tacrolimus, etc.[11][12][13][14][15][16][17][18][19]
Epidemiology and Demographics
Incidence
The estimated incidence of eosinophilic gastroenteritis is approximately 1-20 per 100,000 patients.[5][3] It is a rare disease with approximately 300 reported cases in published literature.[8]
Age
EG can present at any age.[8] However, a higher incidence has been observed in the third to fifth decade of life.[3][1] In pediatric patients with eosinophilic gastroenteritis, the esophagus is usually the involved organ (eosinophilic esophagitis).[5] The youngest documented pediatric case of eosinophilic gastroenteritis occurred in a full-term 10month old infant.[5]
Sex
There is a higher incidence in adult males.[20][5]
Race
Eosinophilic gastroenteritis has been documented in all races.[21] However, most of the cases reported occurred in Caucasians.[8]
Screening
There is no screening guideline for eosinophilic gastroenteritis.
Natural History, Complications, and Prognosis
Natural History
Eosinophilic gastroenteritis is an idiopathic disease. A history of allergy/allergy-related disorders have been documented in a significant number of patients with the disease.
Complications
Complications of eosinophilic gastroenteritis can include the following:[7][4][22][9][3][23]
- Gastric outlet obstruction: Pyloric outlet obstruction has been documented in patients with muscular eosinophilic gastroenteritis, and surgical intervention is often required in severe cases.
- Esophageal narrowing/strictures: Seen when there is esophageal involvement.
- Biliary tract disease such as biliary tract fibrosis and obstruction.
- Intestinal perforation
- Intussusception
- Acute pancreatitis
Prognosis
The prognosis is good with treatment but relapses are common, which may necessitate chronic low dose steroid therapy for maintenance of remission.[3][9]
Diagnosis
History and Symptoms
History
It is important to obtain the following history from the patient:[7]
- Presenting symptoms
- Duration of symptoms
- History of allergy: A history of food allergy/intolerance, drug allergy, allergy-related conditions such as seasonal allergies, atopy, asthma, and nasal polyps should be obtained.
Symptoms
Eosinophilic gastroenteritis can present with several nonspecific gastrointestinal symptoms. The manifestations often depend on the site affected in the GIT, and the involved layer of the gastrointestinal wall.[3][8][24] The following are the gastrointestinal symptoms seen in eosinophilic gastroenteritis:[7][10][5][8][9][25][4]
Common symptoms
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Poor appetite
- Weight loss
- Steatorrhea
- Frank or occult hematochezia
- Abdominal bloating: More often seen in patients with subserosal disease.
- Ascites: Seen more often in patients with subserosal disease.
Uncommon symptoms
- Dysphagia: This has been documented in patients with esophageal involvement.
- Hematemesis
- Jaundice
- Other documented features are Cholangitis, pancreatitis,[26] eosinophilic splenitis, acute appendicitis and giant refractory duodenal ulcer.
Physical Examination
The physical examination findings in eosinophilic gastroenteritis are non-specific, and are mostly dependent on the site and depth of bowel involvement. The following are the common findings that may be present:[3]22036223
HEENT
- Anemia
Gastrointestinal system
- Abdominal tenderness
- Ascites
- Hematochezia on rectal exam
Skin
Eczema may be seen in patients with atopy.
Laboratory Findings
The following laboratory findings can be seen:[7][3]
- CBC: Peripheral blood eosinophilia is often seen, but it may be absent in >20% of affected patients. Patients with subserosal disease often have a higher eosinophil count. Anemia can also be present.
- Elevated serum IgE is a common finding.
- Elevated ESR: This can be moderately elevated in 25% of patients with eosinophilic gastroenteritis.
- Hypoalbuminuria: This can occur as a result of severe malabsorption and protein losing enteropathy.
- Fecal fat test: Mild-moderate steatorrhea is sometimes seen.
- Stool α-1 antitrypsin clearance: For assessment of fecal protein loss.
- Allergy testing: Tests such as skin-prick and RAST testing may be done when specific food and environmental allergies are strongly suspected as triggers for the disease.
Microscopic Findings
Eosinophilic gastroenteritis is a diagnosis of exclusion. There are no well standardized pathologic criteria for making a diagnosis of eosinophilic gastroenteritis. Talley et al. proposed three diagnostic criteria:[3][7]
- Presence of gastrointestinal symptoms
- Biopsy demonstrating eosinophilic infiltration of one or more areas of the GIT (from the esophagus to colon)
- Exclusion of other causes of tissue eosinophilia.
Biopsy
- Biopsy is widely used for making a diagnosis. In the absence of other causes of tissue eosinophilia, eosinophilic infiltration of the GIT on biopsy and/or the presence of eosinophilic ascitic fluid in a patient with gastrointestinal symptoms is diagnostic for eosinophilic gastroenteritis.[5]
- Eosinophilic infiltration of the gastrointestinal tract is seen on histology following endoscopic/surgical biopsies. Abnormal eosinophilic infiltration of the GIT can be defined as the presence of diffuse or multifocal eosinophils ≥20 per high power field.[7][3]
- The diagnosis can occasionally be missed, especially in patients with the localized patchy infiltration. Multiple biopsy samples throughout the GIT (including visually normal areas) should be taken.[3]
Paracentesis
- In cases of suspected eosinophilic ascites, it is important to perform a diagnostic paracentesis.[3]
Hypereosinophilia, the hallmark of allergic response, may be absent in up to 20% of patients, but hypoalbuminaemia and other abnormalities suggestive of malabsorption may be present.
When eosinophilic gastroenteritis is observed in association with eosinophilic infiltration of other organ systems, the diagnosis of idiopathic hypereosinophilic syndrome should be considered.[27]
Imaging Findings
There are no guidelines for the diagnosis of eosinophilic gastroenteritis.
Endoscopy
There are no specific endoscopic findings for eosinophilic gastroenteritis. Gross findings such as gastric pseudopolyps are commonly seen. Other non-specific findings seen in the GIT include erythema, erosions, and lymphonodular hyperplasia occurring in the gastric antrum, fundus, and pyloric regions of the stomach.[5]
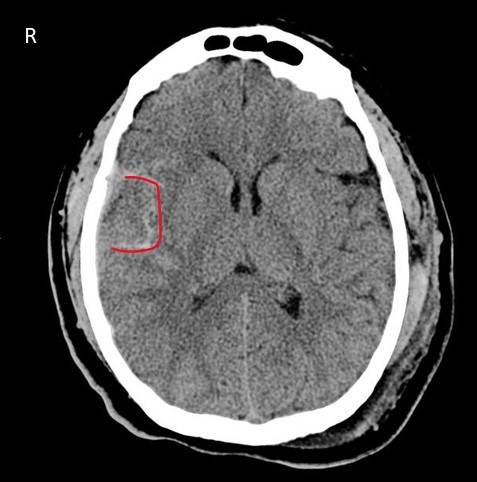
CT scan
Imaging studies such as a CT scan is essential, especially when biopsy studies are not diagnostic.[7] Radiological changes seen in the gastrointestinal tract are non-specific findings such as very prominent bowel folds,
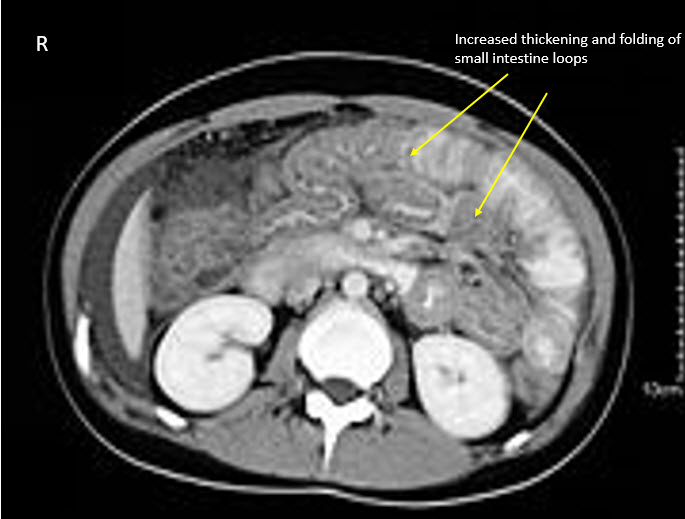
CT scan may show nodular and irregular thickening of the folds in the distal stomach and proximal small bowel, but these findings can also be present in other conditions like Crohn's disease and lymphoma.
The endoscopic appearance in eosinophilic gastroenteritis is nonspecific; it includes erythematous, friable, nodular, and occasional ulcerative changes.[28] Sometimes diffuse inflammation results in complete loss of villi, involvement of multiple layers, submucosal oedema and fibrosis.[29][30]
Radio isotope scan using Tc-99m HMPAO-labeled leukocyte SPECT may be useful in assessing the extent of disease and response to treatment but has little value in diagnosis, as the scan does not help differentiating EG from other causes of inflammation.[31][32]
Treatment
There are no guidelines/definitive consensus for the management of eosinophilic gastroenteritis, and the treatment is usually based on the severity of the disease. Steroids are widely recognized as the mainstay of treatment for eosinophilic gastroenteritis.
Medical Therapy
The medical management of eosinophilic gastroenteritis entails the following:[7][33]:[3][33][34][28][5]28279648
Preferred therapy
- Corticosteroids: This is the mainstay of therapy for eosinophilic gastroenteritis. A dramatic response to corticosteroid therapy is commonly seen in patients with subserosal disease. A 90% response rate to corticosteroid therapy has been documented in some studies.
- Dietary modification
- Elimination of identified food allergies from the diet.
- Introduction of elemental diets.
Alternate therapy
- Montelukast: It can be used alone for the treatment of eosinophilic gastroenteritis or as maintenance therapy. Some patients treated with montelukast alone did not have a relapse.22036223 Montelukast is sometimes used in combination with steroids as a steroid-sparing agent.
- Ketotifen
- Cromolyn sodium
- Suplatast
- Biologic medications such as omalizumab, reslizumab and mepolizumab.
Surgery
Prevention
References
- ↑ 1.0 1.1 Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH (1970). "Eosinophilic gastroenteritis". Medicine (Baltimore). 49 (4): 299–319. PMID 5426746.
- ↑ Treiber GG, Weidner S (2007). "Eosinophilic gastroenteritis". Clin Gastroenterol Hepatol. 5 (5): e16. doi:10.1016/j.cgh.2007.01.011. PMID 17428742.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 Uppal V, Kreiger P, Kutsch E (2016). "Eosinophilic Gastroenteritis and Colitis: a Comprehensive Review". Clin Rev Allergy Immunol. 50 (2): 175–88. doi:10.1007/s12016-015-8489-4. PMID 26054822.
- ↑ 4.0 4.1 4.2 Whitaker IS, Gulati A, McDaid JO, Bugajska-Carr U, Arends MJ (2004). "Eosinophilic gastroenteritis presenting as obstructive jaundice". Eur J Gastroenterol Hepatol. 16 (4): 407–9. PMID 15028974.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Shetty V, Daniel KE, Kesavan A (2017). "Hematemesis as Initial Presentation in a 10-Week-Old Infant with Eosinophilic Gastroenteritis". Case Rep Pediatr. 2017: 2391417. doi:10.1155/2017/2391417. PMC 5337357. PMID 28299223.
- ↑ Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH (1970). "Eosinophilic gastroenteritis". Medicine (Baltimore). 49 (4): 299–319. PMID 5426746.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR (1990). "Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues". Gut. 31 (1): 54–8. PMC 1378340. PMID 2318432 2318432 Check
|pmid=value (help). - ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Baig MA, Qadir A, Rasheed J (2006). "A review of eosinophilic gastroenteritis". J Natl Med Assoc. 98 (10): 1616–9. PMC 2569760. PMID 17052051.
- ↑ 9.0 9.1 9.2 9.3 Lee CM, Changchien CS, Chen PC, Lin DY, Sheen IS, Wang CS; et al. (1993). "Eosinophilic gastroenteritis: 10 years experience". Am J Gastroenterol. 88 (1): 70–4. PMID 8420276.
- ↑ 10.0 10.1 Tan AC, Kruimel JW, Naber TH (2001). "Eosinophilic gastroenteritis treated with non-enteric-coated budesonide tablets". Eur J Gastroenterol Hepatol. 13 (4): 425–7. PMID 11338074 11338074 Check
|pmid=value (help). - ↑ Shakeer VK, Devi SR, Chettupuzha AP, Mustafa CP, Sandesh K, Kumar SK; et al. (2002). "Carbamazepine-induced eosinophilic enteritis". Indian J Gastroenterol. 21 (3): 114–5. PMID 12118924.
- ↑ Lange P, Oun H, Fuller S, Turney JH (1994). "Eosinophilic colitis due to rifampicin". Lancet. 344 (8932): 1296–7. PMID 7968003.
- ↑ Jiménez-Sáenz M, González-Cámpora R, Linares-Santiago E, Herrerías-Gutiérrez JM (2006). "Bleeding colonic ulcer and eosinophilic colitis: a rare complication of nonsteroidal anti-inflammatory drugs". J Clin Gastroenterol. 40 (1): 84–5. PMID 16340639.
- ↑ Bridges AJ, Marshall JB, Diaz-Arias AA (1990). "Acute eosinophilic colitis and hypersensitivity reaction associated with naproxen therapy". Am J Med. 89 (4): 526–7. PMID 2220886.
- ↑ Kakumitsu S, Shijo H, Akiyoshi N, Seo M, Okada M (2000). "Eosinophilic enteritis observed during alpha-interferon therapy for chronic hepatitis C." J Gastroenterol. 35 (7): 548–51. PMID 10905364.
- ↑ Lee JY, Medellin MV, Tumpkin C (2000). "Allergic reaction to gemfibrozil manifesting as eosinophilic gastroenteritis". South Med J. 93 (8): 807–8. PMID 10963515.
- ↑ Ravi S, Holubka J, Veneri R, Youn K, Khatib R (1993). "Clofazimine-induced eosinophilic gastroenteritis in AIDS". Am J Gastroenterol. 88 (4): 612–3. PMID 8470652.
- ↑ Barak N, Hart J, Sitrin MD (2001). "Enalapril-induced eosinophilic gastroenteritis". J Clin Gastroenterol. 33 (2): 157–8. PMID 11468446.
- ↑ Saeed SA, Integlia MJ, Pleskow RG, Calenda KA, Rohrer RJ, Dayal Y; et al. (2006). "Tacrolimus-associated eosinophilic gastroenterocolitis in pediatric liver transplant recipients: role of potential food allergies in pathogenesis". Pediatr Transplant. 10 (6): 730–5. doi:10.1111/j.1399-3046.2006.00538.x. PMID 16911498.
- ↑ Guandalini, Stefano (2004). Essential Pediatric Gastroenterology and Nutrition. City: McGraw-Hill Professional. ISBN 0071416307. Page 210.
- ↑ Guandalini, Stefano (2004). Essential Pediatric Gastroenterology and Nutrition. City: McGraw-Hill Professional. ISBN 0071416307. Page 210.
- ↑ Jimenez-Saenz M, Villar-Rodriguez JL, Torres Y, Carmona I, Salas-Herrero E, Gonzalez-Vilches J; et al. (2003). "Biliary tract disease: a rare manifestation of eosinophilic gastroenteritis". Dig Dis Sci. 48 (3): 624–7. PMID 12757181 12757181 Check
|pmid=value (help). - ↑ Lyngbaek S, Adamsen S, Aru A, Bergenfeldt M (2006). "Recurrent acute pancreatitis due to eosinophilic gastroenteritis. Case report and literature review". JOP. 7 (2): 211–7. PMID 16525206.
- ↑ Lee C, Changchien C, Chen P, Lin D, Sheen I, Wang C, Tai D, Sheen-Chen S, Chen W, Wu C (1993). "Eosinophilic gastroenteritis: 10 years experience". Am. J. Gastroenterol. 88 (1): 70–4. PMID 8420276.
- ↑ Tien FM, Wu JF, Jeng YM, Hsu HY, Ni YH, Chang MH; et al. (2011). "Clinical features and treatment responses of children with eosinophilic gastroenteritis". Pediatr Neonatol. 52 (5): 272–8. doi:10.1016/j.pedneo.2011.06.006. PMID 22036223.
- ↑ Lyngbaek S, Adamsen S, Aru A, Bergenfeldt M (2006). "Recurrent acute pancreatitis due to eosinophilic gastroenteritis. Case report and literature review". JOP. 7 (2): 211–7. PMID 16525206.
- ↑ Matsushita M, Hajiro K, Morita Y, Takakuwa H, Suzaki T (1995). "Eosinophilic gastroenteritis involving the entire digestive tract". Am. J. Gastroenterol. 90 (10): 1868–70. PMID 7572911.
- ↑ 28.0 28.1 Chen MJ, Chu CH, Lin SC, Shih SC, Wang TE (2003). "Eosinophilic gastroenteritis: clinical experience with 15 patients". World J Gastroenterol. 9 (12): 2813–6. PMC 4612059. PMID 14669340.
- ↑ Johnstone J, Morson B (1978). "Eosinophilic gastroenteritis". Histopathology. 2 (5): 335–48. PMID 363591.
- ↑ Katz A, Goldman H, Grand R (1977). "Gastric mucosal biopsy in eosinophilic (allergic) gastroenteritis". Gastroenterology. 73 (4 Pt 1): 705–9. PMID 892374.
- ↑ Lee K, Hahm K, Kim Y, Kim J, Cho S, Jie H, Park C, Yim H (1997). "The usefulness of Tc-99m HMPAO labeled WBC SPECT in eosinophilic gastroenteritis". Clinical nuclear medicine. 22 (8): 536–41. PMID 9262899.
- ↑ Imai E, Kaminaga T, Kawasugi K, Yokokawa T, Furui S (2003). "The usefulness of 99mTc-hexamethylpropyleneamineoxime white blood cell scintigraphy in a patient with eosinophilic gastroenteritis". Annals of nuclear medicine. 17 (7): 601–3. PMID 14651361.
- ↑ 33.0 33.1 Barbie DA, Mangi AA, Lauwers GY (2004). "Eosinophilic gastroenteritis associated with systemic lupus erythematosus". J Clin Gastroenterol. 38 (10): 883–6. PMID 15492606.
- ↑ Katz AJ, Twarog FJ, Zeiger RS, Falchuk ZM (1984). "Milk-sensitive and eosinophilic gastroenteropathy: similar clinical features with contrasting mechanisms and clinical course". J Allergy Clin Immunol. 74 (1): 72–8. PMID 6547462.