Single photon emission computed tomography
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
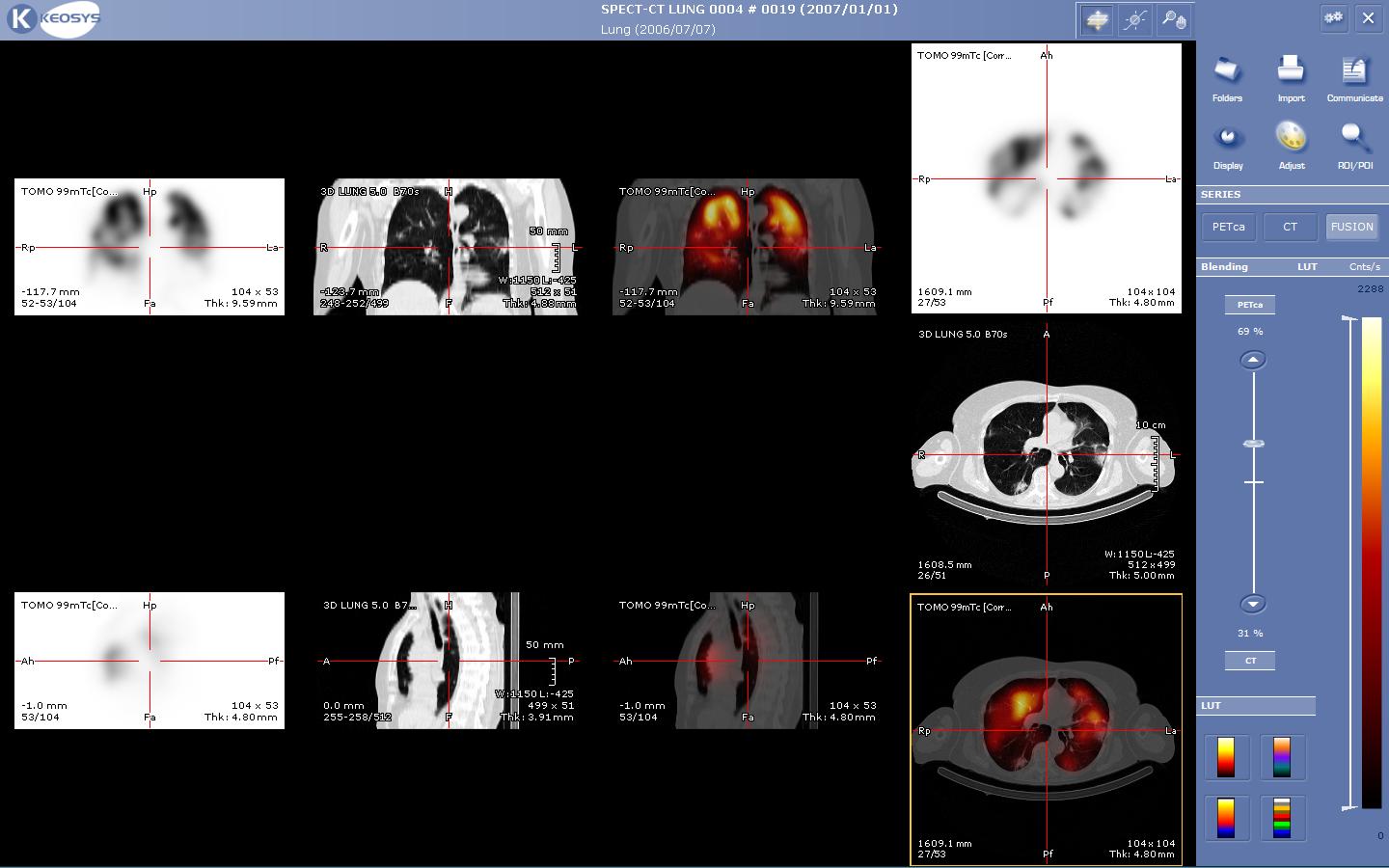
Single photon emission computed tomography (SPECT) is a nuclear medicine tomographic imaging technique using gamma rays. It is very similar to conventional nuclear medicine planar imaging using a gamma camera. However, it is able to provide true 3D information. This information is typically presented as cross-sectional slices through the patient, but can be freely reformatted or manipulated as required.
Principles
In the same way that a plain X-ray is a 2-dimensional (2-D) view of a 3-dimensional structure, the image obtained by a gamma camera image is a 2-D view of 3-D distribution of a radionuclide. SPECT imaging is performed by using a gamma camera to acquire multiple 2-D images (also called projections), from multiple angles. A computer is then used to apply a tomographic reconstruction algorithm to the multiple projections, yielding a 3-D dataset. This dataset may then be manipulated to show thin slices along any chosen axis of the body, similar to those obtained from other tomographic techniques, such as MRI, CT, and PET.
Because SPECT acquisition is very similar to planar gamma camera imaging, the same radiopharmaceuticals may be used. If a patient is examined in another type of nuclear medicine scan but the images are non-diagnostic, it may be possible to proceed straight to SPECT by moving the patient to a SPECT instrument, or even by simply reconfiguring the camera for SPECT image acquisition while the patient remains on the table.
To acquire SPECT images, the gamma camera is rotated around the patient. Projections are acquired at defined points during the rotation, typically every 3-6 degrees. In most cases, a full 360 degree rotation is used to obtain an optimal reconstruction. The time taken to obtain each projection is also variable, but 15 – 20 seconds is typical. This gives a total scan time of 15-20 minutes.
Multi-headed gamma cameras can provide accelerated acquisition. For example, a dual headed camera can be used with heads spaced 180 degrees apart, allowing 2 projections to be acquired simultaneously, with each head requiring 180 degrees of rotation. Triple-head cameras with 120 degree spacing are also used.
Cardiac gated acquisition (Medical imaging)|gated acquisitions are possible with SPECT, just as with planar imaging techniques such as MUGA. Triggered by EKG to obtain differential information about the heart in various parts of its cycle, gated myocardial SPECT can be used to obtain quantitative information about myocardial perfusion, thickness, and contractility of the myocardium during various parts of the cardiac cycle; and also to allow calculation of left ventricular ejection fraction, stroke volume, and cardiac output.
Application
SPECT can be used to complement any gamma imaging study, where a true 3D representation can be helpful. E.g. tumor imaging, infection (leukocyte) imaging, thyroid imaging or bone imaging.
Because SPECT permits accurate localisation in 3D space, it can be used to provide information about localised function in internal organs. E.g. functional cardiac or brain imaging.
Myocardial perfusion imaging
Myocardial perfusion imaging (MPI) is a form of functional cardiac imaging, used for the diagnosis of ischemic heart disease. The underlying principle is that under conditions of stress, diseased myocardium receives less blood flow than normal myocardium. MPI is one of several types of cardiac stress test.
A cardiac specific radiopharmaceutical is administered. E.g. 99mTc-tetrofosmin (Myoview™, GE healthcare), 99mTc-sestamibi (Cardiolite®, Bristol-Myers Squibb). Following this, the heart rate is raised to induce myocardial stress, either by exercise or pharmacologically with adenosine, dobutamine or dipyridamole (aminophylline can be used to reverse the effects of dipyridamole).
SPECT imaging performed after stress reveals the distribution of the radiopharmaceutical, and therefore the relative blood flow to the different regions of the myocardium. Diagnosis is made by comparing stress images to a further set of images obtained at rest. As the radionuclide redistributes slowly, it is not usually possible to perform both sets of images on the same day, hence a second attendance is required 1-7 days later (although, with a Tl-201 myocardial perfusion study with dipyridamole, rest images can be acquired as little as two-hours post stress). However, if stress imaging is normal, it is unnecessary to perform rest imaging, as it too will be normal – thus stress imaging is normally performed first.
MPI has been demonstrated to have an overall accuracy of about 83% (sensitivity: 85%; specificity: 72%) [2], and is comparable (or better) than other non-invasive tests for ischemic heart disease, including stress echocardiography. The gold-standard test, however, remains invasive cardiac catheterization.
Functional brain imaging
Usually the gamma-emitting tracer used in functional brain imaging is 99mTc-HMPAO (hexamethylpropylene amine oxime). 99mTc is a metastable nuclear isomer which emits gamma rays which can be detected by a gamma camera. When it is attached to HMPAO, this allows 99mTc to be taken up by brain tissue in a manner proportial to brain blood flow, in turn allowing brain blood flow to be assessed with the nuclear gamma camera.
Because blood flow in the brain is tightly coupled to local brain metabolism and energy use, the 99mTc-HMPAO tracer (as well as the similar 99mTc-EC tracer) is used to assess brain metabolism regionally, in an attempt to diagnose and differentiate the different causal pathologies of dementia. Meta analysis of many reported studies suggests that SPECT with this tracer is about 74% sensitive at diagnosing Alzheimer's disease, vs. 81% sensitivity for clinical exam (mental testing, etc.). More recent studies have show accuracy of SPECT in Alzheimer diagnosis as high as 88% PMID 16785801. In meta analysis, SPECT was superior to clinical exam and clinical criteria (91% vs. 70%) in being able to differentiate Alzheimer's disease from vascular dementias. PMID 15545324 This latter ability relates to SPECT's imaging of local metabolism of the brain, in which the patchy loss of cortical metabolism seen in multiple strokes differs clearly from the more even or "smooth" loss of non-occipital cortical brain function typical of Alzheimer's disease.
99mTc-HMPAO SPECT scanning competes with FDG PET scanning of the brain, which works to assess regional brain glucose metabolism, to provide very similar information about local brain damage from many processes. SPECT is more widely available, however, for the basic reason that the radioisotope generation technology is longer-lasting and far less expensive in SPECT, and the gamma scanning equipment is less expensive as well. The reason for this is that 99mTc (technetium-99m) is extracted from relatively simple technetium-99m generators which are delivered to hospitals and scanning centers weekly, to supply fresh radioisotope, whereas FDG PET relies on FDG which must be made in an expensive medical cyclotron and "hot-lab" (automated chemistry lab for radiopharmaceutical manufacture), then must be delivered directly to scanning sites, with delivery-fraction for each trip handicapped by its natural short 110 minute half-life.
Reconstruction
Reconstructed images typically have resolutions of 64x64 or 128x128 pixels, with the pixel sizes ranging from 3-6 mm. The number of projections acquired is chosen to be approximately equal to the width of the resulting images. In general, the resulting reconstructed images will be of lower resolution, have increased noise than planar images, and be susceptible to artifacts.
Scanning is time consuming, and it is essential that there is no patient movement during the scan time. Movement can cause significant degradation of the reconstructed images, although movement compensation reconstruction techniques can help with this. A highly uneven distribution of radiopharmaceutical also has the potential to cause artifacts. A very intense area of activity (e.g. the bladder) can cause extensive streaking of the images and obscure neighboring areas of activity. (This is a limitation of the filtered back projection reconstruction algorithm. Iterative reconstruction is an alternative algorithm which is growing in importance, as it is less sensitive to artifacts and can also correct for attenuation).
Attenuation of the gamma rays within the patient can lead to significant underestimation of activity in deep tissues, compared to superficial tissues. Approximate correction is possible, based on relative position of the activity. However, optimal correction is obtained with measured attenuation values. Modern SPECT equipment is available with an integrated x-ray CT scanner. As X-ray CT images are an attenuation map of the tissues, this data can be incorporated into the SPECT reconstruction to correct for attenuation. It also provides a precisely registered CT image which can provide additional anatomical information.
Further reading
- For anyone interested in the brain-imaging applications of SPECT then this is a great review, although the full-text article is not available online without a subscription to the journal. The following link provides a link to the abstract only, and you might be able to access the full article through a membership with a medical library. W. Gordon Frankle, Mark Slifstein, Peter S. Talbot, and Marc Laruelle (2005). "Neuroreceptor Imaging in Psychiatry: Theory and Applications". International Review of Neurobiology, 67: 385-440.
Typical SPECT acquisition protocols
| Study | Radioisotope | Emission energy (keV) | Half-life | Radiopharmaceutical | Activity (MBq) | Rotation (degrees) | Projections | Image resolution | Time per projection (s) |
|---|---|---|---|---|---|---|---|---|---|
| Bone scan | Technetium-99m | 140 | 6 hours | Phosphonates / Bisphosphonates | 800 | 360 | 120 | 128 x 128 | - |
| Myocardial perfusion scan | Technetium-99m | 140 | 6 hours | tetrofosmin; Sestamibi | 700 | 180 | 60 | 128 x 128 | 30 |
| Brain scan | Technetium-99m | 140 | 6 hours | HMPAO; ECD | 555-1110 | 360 | 64 | 128 x 128 | 30 |
| Tumor scan | Indium-111 | 159 | 13 hours | MIBG | 400 | 360 | 60 | 64 x 64 | 30 |
| White cell scan | Indium-111 & Technetium-99m | 171 & 245 | 67 hours | in vitro labelled leucocytes | 18 | 360 | 60 | 64 x 64 | 30 |
Related chapters
- Gamma camera
- Neuroimaging
- Functional neuroimaging
- Magnetic resonance imaging
- Positron emission tomography
- ISAS (Ictal-Interictal SPECT Analysis by SPM)
Resources
- Nuclear Medicine Information
- GE HealthCare, Philips, Siemens - Major manufacturers of SPECT scanners
- ISAS (Ictal-Interictal SPECT Analysis by SPM) - Yale University
de:Single Photon Emission Computed Tomography fa:مقطعنگاری رایانهای تک فوتونی it:Tomografia ad emissione di fotone singolo nl:SPECT-scan no:SPECT