Metoprolol tartrate (tablet): Difference between revisions
No edit summary |
No edit summary |
||
| Line 175: | Line 175: | ||
In general, administration of a [[beta-blocker]] should be withheld before [[dipyridamole]] testing, with careful monitoring of heart rate following the [[dipyridamole]] injection. | In general, administration of a [[beta-blocker]] should be withheld before [[dipyridamole]] testing, with careful monitoring of heart rate following the [[dipyridamole]] injection. | ||
|useInGeri=* The geriatric population may show slightly higher plasma concentrations of metoprolol as a combined result of a decreased metabolism of the drug in elderly population and a decreased hepatic blood flow. However, this increase is not clinically significant or therapeutically relevant. | |||
|useInRenalImpair=The systemic availability and half-life of metoprolol in patients with renal failure do not differ to a clinically significant degree from those in normal subjects. | |||
|useInHepaticImpair=Since the drug is primarily eliminated by hepatic metabolism, hepatic impairment may impact the pharmacokinetics of metoprolol. The elimination half-life of metoprolol is considerably prolonged, depending on severity (up to 7.2 h). | |||
|useInGeri= | |||
|useInRenalImpair= | |||
|useInHepaticImpair=( | |||
|administration=(Oral/Intravenous/etc) | |administration=(Oral/Intravenous/etc) | ||
|monitoring======Condition 1===== | |monitoring======Condition 1===== | ||
Revision as of 14:28, 7 July 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Metoprolol tartrate (tablet) is a anti-anginal, antiarrhythmic, beta-adrenergic blocker that is FDA approved for the {{{indicationType}}} of acute myocardial infarction (AMI). Common adverse reactions include bradyarrhythmia, constipation, depression, diarrhea, dizziness, dyspnea, fatigue, headache, heart block, heart failure, hypotension, indigestion, nausea, pruritus, rash, and wheezing.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Hypertension
- Dosing Information
- Individualize the dosage of Lopressor tablets. Lopressor tablets should be taken with or immediately following meals.
- The usual initial dosage of Lopressor tablets is 100 mg daily in single or divided doses, whether used alone or added to a diuretic. Increase the dosage at weekly (or longer) intervals until optimum blood pressure reduction is achieved. In general, the maximum effect of any given dosage level will be apparent after 1 week of therapy. The effective dosage range of Lopressor tablets is 100-450 mg per day. Dosages above 450 mg per day have not been studied. While once-daily dosing is effective and can maintain a reduction in blood pressure throughout the day, lower doses (especially 100 mg) may not maintain a full effect at the end of the 24-hour period, and larger or more frequent daily doses may be required. This can be evaluated by measuring blood pressure near the end of the dosing interval to determine whether satisfactory control is being maintained throughout the day. Beta1 selectivity diminishes as the dose of Lopressor is increased.
Angina Pectoris
- Dosing Information
- The dosage of Lopressor tablets should be individualized. Lopressor tablets should be taken with or immediately following meals.
- The usual initial dosage of Lopressor tablets is 100 mg daily, given in two divided doses. gradually increase the dosage at weekly intervals until optimum clinical response has been obtained or there is pronounced slowing of the heart rate. The effective dosage range of Lopressor tablets is 100-400 mg per day. Dosages above 400 mg per day have not been studied. If treatment is to be discontinued, gradually decrease the dosage over a period of 1-2 weeks
Myocardial Infarction
- Dosing information
- Early treatment:
- During the early phase of definite or suspected acute myocardial infarction, initiate treatment with Lopressor as soon as possible after the patient's arrival in the hospital. Such treatment should be initiated in a coronary care or similar unit immediately after the patient's hemodynamic condition has stabilized.
- Begin treatment in this early phase with the intravenous administration of three bolus injections of 5 mg of Lopressor each; give the injections at approximately 2-minute intervals. During the intravenous administration of Lopressor, monitor blood pressure, heart rate, and electrocardiogram.
- In patients who tolerate the full intravenous dose (15 mg), initiate Lopressor tablets, 50 mg every 6 hours, 15 minutes after the last intravenous dose and continue for 48 hours. Thereafter, the maintenance dosage is 100 mg twice daily.
- Start patients who appear not to tolerate the full intravenous dose on Lopressor tablets either 25 mg or 50 mg every 6 hours (depending on the degree of intolerance) 15 minutes after the last intravenous dose or as soon as their clinical condition allows. In patients with severe intolerance, discontinue Lopressor.
- Late treatment: Start patients with contraindications to treatment during the early phase of suspected or definite myocardial infarction, patients who appear not to tolerate the full early treatment, and patients in whom the physician wishes to delay therapy for any other reason on Lopressor tablets, 100 mg twice daily, as soon as their clinical condition allows. Continue therapy for at least 3 months. Although the efficacy of Lopressor beyond 3 months has not been conclusively established, data from studies with other beta blockers suggest that treatment should be continued for 1-3 years.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Atrial Fibrillation, Rate Control
- Developed by: American College of Cardiology (ACC) and American Heart Association (AHA)
- Class of Recommendation: Class I
- Level of Evidence: Level B
- Dosing Information
- Acute Setting: Lopressor injection 2.5—5 mg IV bolus over 2 min; up to 3 doses[1]
In the absence of preexcitation, intravenous administration of beta blockers (esmolol, metoprolol, or propranolol) or nondihydropyridine calcium channel antagonists (verapamil, diltiazem) is recommended to slow the ventricular response to atrial fibrillation in the acute setting, exercising caution in patients with hypotension or heart failure.[2]
Non–Guideline-Supported Use
Atrial flutter
- Dosing Information
- Lopressor injection dose range: 2—15 mg[3]
Multifocal atrial tachycardia
- Dosing Information
- Lopressor injection dose range: 2—15 mg[3]
Supraventricular Tachycardia
- Dosing Information
- Lopressor injection dose range: 2—15 mg[3]
Aggressive Behavior
Injection Site Pain Associated with Propofol Use
- Dosing Information
- Pretreatment with Lopressor injection 2 mg.[4]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Metoprolol tartrate (tablet) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Metoprolol tartrate in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Metoprolol tartrate in pediatric patients.
Contraindications
- Hypertension and Angina: Lopressor is contraindicated in sinus bradycardia, heart block greater than first degree, cardiogenic shock, and overt cardiac failure.
- Hypersensitivity to Lopressor and related derivatives, or to any of the excipients; hypersensitivity to other beta blockers (cross sensitivity between beta blockers can occur).
- Sick-sinus syndrome.
- Severe peripheral arterial circulatory disorders.
- Myocardial Infarction: Lopressor is contraindicated in patients with a heart rate <45 beats/min; second-degree heart block and third-degree heart block; significant first-degree heart block (P-R interval ≥0.24 sec); systolic blood pressure <100 mmHg; or moderate-to-severe cardiac failure.
Warnings
Heart Failure
Beta blockers, like Lopressor, can cause depression of myocardial contractility and may precipitate heart failure and cardiogenic shock. If signs or symptoms of heart failure develop, treat the patient according to recommended guidelines. It may be necessary to lower the dose of Lopressor or to discontinue it.
Ischemic Heart Disease
Do not abruptly discontinue Lopressor therapy in patients with coronary artery disease. Severe exacerbation of angina, myocardial infarction and ventricular arrhythmias have been reported in patients with coronary artery disease following the abrupt discontinuation of therapy with beta-blockers. When discontinuing chronically administered Lopressor, particularly in patients with coronary artery disease, the dosage should be gradually reduced over a period of 1-2 weeks and the patient should be carefully monitored. If angina markedly worsens or acute coronary insufficiency develops, Lopressor administration should be reinstated promptly, at least temporarily, and other measures appropriate for the management of unstable angina should be taken. Patients should be warned against interruption or discontinuation of therapy without the physician's advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue Lopressor therapy abruptly even in patients treated only for hypertension.
Use During Major Surgery
Chronically administered beta-blocking therapy should not be routinely withdrawn prior to major surgery; however, the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Bradycardia
Bradycardia, including sinus pause, heart block, and cardiac arrest have occurred with the use of Lopressor. Patients with first-degree atrioventricular block, sinus node dysfunction, or conduction disorders may be at increased risk. Monitor heart rate and heart rhythm in patients receiving Lopressor. If severe bradycardia develops, reduce or stop Lopressor.
Exacerbation of Bronchospastic Disease
Patients with bronchospastic disease,should, in general, not receive beta blockers, including Lopressor. Because of its relative beta1 selectivity, however, Lopressor may be used in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Because beta1 selectivity is not absolute use the lowest possible dose of Lopressor and consider administering Lopressor in smaller doses three times daily, instead of larger doses two times daily, to avoid the higher plasma levels associated with the longer dosing interval. Bronchodilators, including beta2 agonists, should be readily available or administered concomitantly.
Diabetes and Hypoglycemia
Beta blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected.
Pheochromocytoma
If Lopressor is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
Thyrotoxicosis
Lopressor may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Avoid abrupt withdrawal of beta blockade, which might precipitate a thyroid storm.
Adverse Reactions
Clinical Trials Experience
Hypertension and Angina
- Most adverse effects have been mild and transient.
- Central Nervous System: Tiredness and dizziness have occurred in about 10 of 100 patients. Depression has been reported in about 5 of 100 patients. Mental confusion and short-term memory loss have been reported. Headache, nightmares, and insomnia have also been reported.
- Cardiovascular: Shortness of breath and bradycardia have occurred in approximately 3 of 100 patients. Cold extremities; arterial insufficiency, usually of the Raynaud type; palpitations; congestive heart failure; peripheral edema; and hypotension have been reported in about 1 of 100 patients. Gangrene in patients with pre-existing severe peripheral circulatory disorders has also been reported very rarely.
- Respiratory: Wheezing (bronchospasm) and dyspnea have been reported in about 1 of 100 patients. Rhinitis has also been reported.
- Gastrointestinal: Diarrhea has occurred in about 5 of 100 patients. Nausea, dry mouth, gastric pain, constipation, flatulence, and heartburn have been reported in about 1 of 100 patients. Vomiting was a common occurrence.
- Hypersensitive Reactions: Pruritus or rash have occurred in about 5 of 100 patients. Very rarely, photosensitivity and worsening of psoriasis has been reported.
- Miscellaneous: Peyronie's disease has been reported in fewer than 1 of 100,000 patients. Musculoskeletal pain, blurred vision, and tinnitus have also been reported. There have been rare reports of reversible alopecia, agranulocytosis, and dry eyes. Discontinuation of the drug should be considered if any such reaction is not otherwise explicable. There have been very rare reports of weight gain, arthritis, and retroperitoneal fibrosis (relationship to Lopressor has not been definitely established). The oculomucocutaneous syndrome associated with the beta blocker practolol has not been reported with Lopressor.
Myocardial Infarction
- Central Nervous System: Tiredness has been reported in about 1 of 100 patients. Vertigo, sleep disturbances, hallucinations, headache, dizziness, visual disturbances, confusion, and reduced libido have also been reported, but a drug relationship is not clear.
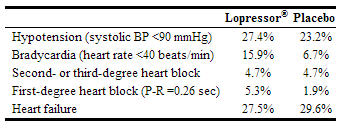
- Cardiovascular: In the randomized comparison of Lopressor and placebo, the following adverse reactions were reported:
- Respiratory: Dyspnea of pulmonary origin has been reported in fewer than 1 of 100 patients.
- Gastrointestinal: Nausea and abdominal pain have been reported in fewer than 1 of 100 patients.
- Dermatologic: Rash and worsened psoriasis have been reported, but a drug relationship is not clear.
- Miscellaneous: Unstable diabetes and claudication have been reported, but a drug relationship is not clear.
Potential Adverse Reactions
- A variety of adverse reactions not listed above have been reported with other beta blockers and should be considered potential adverse reactions to Lopressor.
- Central Nervous System: Reversible mental depression progressing to catatonia; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics.
- Cardiovascular: Intensification of AV block.
- Hematologic: Agranulocytosis, nonthrombocytopenic purpura and thrombocytopenic purpura.
- Hypersensitive Reactions: Fever combined with aching and sore throat, laryngospasm and respiratory distress.
Postmarketing Experience
The following adverse reactions have been reported during postapproval use of Lopressor:
- Confusional state.
- An increase in blood triglycerides and a decrease in High Density Lipoprotein (HDL).
- Hepatitis, jaundice and non-specific hepatic dysfunction.
- Isolated cases of transaminase, alkaline phosphatase, and lactic dehydrogenase elevations have also been reported.
- Because these reports are from a population of uncertain size and are subject to confounding factors, it is not possible to reliably estimate their frequency
Drug Interactions
Catecholamine-depleting Drugs
Catecholamine-depleting drugs (e.g., reserpine) may have an additive effect when given with beta blockers or monoamine oxidase (MAO) inhibitors. Observe patients treated with metoprolol plus a catecholamine depletor for evidence of hypotension or marked bradycardia, which may produce vertigo, syncope, or postural hypotension. In addition, possibly significant hypertension may theoretically occur up to 14 days following discontinuation of the concomitant administration with an irreversible MAO inhibitor.
Digitalis Glycosides and Beta Blockers
Both digitalis glycosides and beta blockers slow atrioventricular conduction and decrease heart rate. Concomitant use can increase the risk of bradycardia. Monitor heart rate and PR interval.
Calcium channel blockers
Concomitant administration of a beta blockers with a calcium channel blocker may produce an additive reduction in myocardial contractility because of negative chronotropic and inotropic effects.
CYP2D6 Inhibitors
Potent inhibitors of the CYP2D6 enzyme may increase the plasma concentration of metoprolol which would mimic the pharmacokinetics of CYP2D6 poor metabolizer. Increase in plasma concentrations of metoprolol would decrease the cardioselectivity of metoprolol. Known clinically significant potent inhibitors of CYP2D6 are antidepressants such as fluvoxamine, fluoxetine, paroxetine, sertraline, bupropion, clomipramine, and desipramine; antipsychotics such as chlorpromazine, fluphenazine, haloperidol, and thioridazine; antiarrhythmics such as quinidine or propafenone; antiretrovirals such as ritonavir; antihistamines such as diphenhydramine; antimalarials such as hydroxychloroquine or quinidine; antifungals such as terbinafine.
Hydralazine
Concomitant administration of hydralazine may inhibit presystemic metabolism of metoprolol leading to increased concentrations of metoprolol.
Alpha-adrenergic agents
Antihypertensive effect of alpha blocker such as guanethidine, betanidine, reserpine, alpha-methyldopa or clonidine may be potentiated by beta-blockers including metoprolol. Beta blockers may also potentiate the postural hypotensive effect of the first dose of prazosin, probably by preventing reflex tachycardia. On the contrary, beta blockers may also potentiate the hypertensive response to withdrawal of clonidine in patients receiving concomitant clonidine and beta blocker. If a patient is treated with clonidine and metoprolol concurrently, and clonidine treatment is to be discontinued, stop metoprolol several days before clonidine is withdrawn. Rebound hypertension that can follow withdrawal of clonidine may be increased in patients receiving concurrent beta-blocker treatment.
Ergot Alkaloid
Concomitant administration with beta-blockers may enhance the vasoconstrictive action of ergot alkaloids.
Dipyridamole
In general, administration of a beta-blocker should be withheld before dipyridamole testing, with careful monitoring of heart rate following the dipyridamole injection.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA):
There is no FDA guidance on usage of Metoprolol tartrate (tablet) in women who are pregnant.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Metoprolol tartrate (tablet) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Metoprolol tartrate (tablet) during labor and delivery.
Nursing Mothers
There is no FDA guidance on the use of Metoprolol tartrate (tablet) in women who are nursing.
Pediatric Use
There is no FDA guidance on the use of Metoprolol tartrate (tablet) in pediatric settings.
Geriatic Use
- The geriatric population may show slightly higher plasma concentrations of metoprolol as a combined result of a decreased metabolism of the drug in elderly population and a decreased hepatic blood flow. However, this increase is not clinically significant or therapeutically relevant.
Gender
There is no FDA guidance on the use of Metoprolol tartrate (tablet) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Metoprolol tartrate (tablet) with respect to specific racial populations.
Renal Impairment
The systemic availability and half-life of metoprolol in patients with renal failure do not differ to a clinically significant degree from those in normal subjects.
Hepatic Impairment
Since the drug is primarily eliminated by hepatic metabolism, hepatic impairment may impact the pharmacokinetics of metoprolol. The elimination half-life of metoprolol is considerably prolonged, depending on severity (up to 7.2 h).
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Metoprolol tartrate (tablet) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Metoprolol tartrate (tablet) in patients who are immunocompromised.
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
Solution
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Y-Site
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Admixture
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Syringe
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
TPN/TNA
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
Metoprolol tartrate (tablet)
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | ? |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
(Description)
Structure
(Description with picture)
Pharmacodynamics
(Description)
Pharmacokinetics
(Description)
Nonclinical Toxicology
(Description)
Clinical Studies
Condition 1
(Description)
Condition 2
(Description)
Condition 3
(Description)
How Supplied
(Description)
Storage
There is limited information regarding Metoprolol tartrate (tablet) Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Metoprolol tartrate (tablet) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Metoprolol tartrate (tablet) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
(Patient Counseling Information)
Precautions with Alcohol
Alcohol-SandboxAlonso interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Metoprolol tartrate (tablet) Brand Names in the drug label.
Look-Alike Drug Names
- (Paired Confused Name 1a) — (Paired Confused Name 1b)
- (Paired Confused Name 2a) — (Paired Confused Name 2b)
- (Paired Confused Name 3a) — (Paired Confused Name 3b)
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Fuster, V.; Rydén, LE.; Cannom, DS.; Crijns, HJ.; Curtis, AB.; Ellenbogen, KA.; Halperin, JL.; Le Heuzey, JY.; Kay, GN. (2006). "ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients with Atrial Fibrillation)". Eur Heart J. 27 (16): 1979–2030. doi:10.1093/eurheartj/ehl176. PMID 16885201. Unknown parameter
|month=ignored (help) - ↑ Wann, LS.; Curtis, AB.; Ellenbogen, KA.; Estes, NA.; Ezekowitz, MD.; Jackman, WM.; January, CT.; Lowe, JE.; Page, RL. (2013). "Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines". Circulation. 127 (18): 1916–26. doi:10.1161/CIR.0b013e318290826d. PMID 23545139. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 3.2 Amsterdam, EA.; Kulcyski, J.; Ridgeway, MG. (1991). "Efficacy of cardioselective beta-adrenergic blockade with intravenously administered metoprolol in the treatment of supraventricular tachyarrhythmias". J Clin Pharmacol. 31 (8): 714–8. PMID 1880230. Unknown parameter
|month=ignored (help) - ↑ Aşik, I.; Yörükoğlu, D.; Gülay, I.; Tulunay, M. (2003). "Pain on injection of propofol: comparison of metoprolol with lidocaine". Eur J Anaesthesiol. 20 (6): 487–9. PMID 12803269. Unknown parameter
|month=ignored (help)