Gonorrhea physical examination: Difference between revisions
No edit summary |
|||
| Line 53: | Line 53: | ||
**Periorbital edema | **Periorbital edema | ||
**Corneal involvement | **Corneal involvement | ||
*Neonatal Conjunctivitis | *[[Neonatal Conjunctivitis]] | ||
**[[Chemosis]] | **[[Chemosis]] | ||
**Severe lid edema | **Severe lid edema | ||
Revision as of 20:06, 4 October 2016
|
Gonorrhea Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gonorrhea physical examination On the Web |
|
American Roentgen Ray Society Images of Gonorrhea physical examination |
|
Risk calculators and risk factors for Gonorrhea physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2]
Overview
Women with gonococcal infection usually appear to be well until complications such as PID develop. Physical examination of women with gonococcal infection is usually remarkable for mucopurulent urethral, cervical or vaginal discharge, friable appearance of the cervix, and cervical motion tenderness. Common physical examination finding of gonococcal infection among men includes mucopurulent urethral discharge. Less commonly penile edema, and epididymal tenderness and edema (epididymitis) may also be seen as a part of complicated gonococcal infection.[1][2][3]
Physical examination of patients with pharyngeal gonococcal infection is usually remarkable for mild pharyngeal exudates and rectal gonococcal infection is usually remarkable for mucopurulent anal discharge. Physical examination of patients with disseminated gonococcal infection (DGI) is usually remarkable for fever, pustular or vesicular rash, and musculoskeletal findings.[1][4]
Physical examination
Common urogenital and extragenital Infection
The most common site of gonococcal infection is the urethra, endocervix, rectum, and pharynx. Physical examination of patients with gonococcal infection is usually remarkable for:
| Type of Gonococcal Infection | Physical Examination |
|---|---|
| Urogenital infection in men[2] |
|
| Urogenital infection in women:[1][3][5][6][7][8] |
|
| Proctitis[9] |
|
| Pharyngitis[10][11] |
|
| Conjunctivitis |
|
Disseminated Gonococcal Infection
Dissemination gonococcal infection usually can result two clinical syndromes:[4][12][13]
- Septic arthritis (purulent arthritis)
- Arthritis-dermatitis syndromes (with a triad of tenosynovitis, dermatitis, and polyarthralgias)
Other less common manifestations of disseminated gonococcal infection include:
Physical examination of patients with disseminated gonococcal infection is usually remarkable for:[1][4]
| Disseminated Gonococcal Infection | Organ systems |
|---|---|
| General Appearance |
Note: Occurs in the acute phase of infection |
| Skin |
|
| Eye |
|
| Musculoskeletal |
Note: purulent arthritis may be abrupt onset of monoarthritis or oligoarthritis without skin lesions and fever
Note: most commonly occurs in hands and less commonly lower extremities
|
| Central Nervous System |
|
| Cardiac |
|
Images
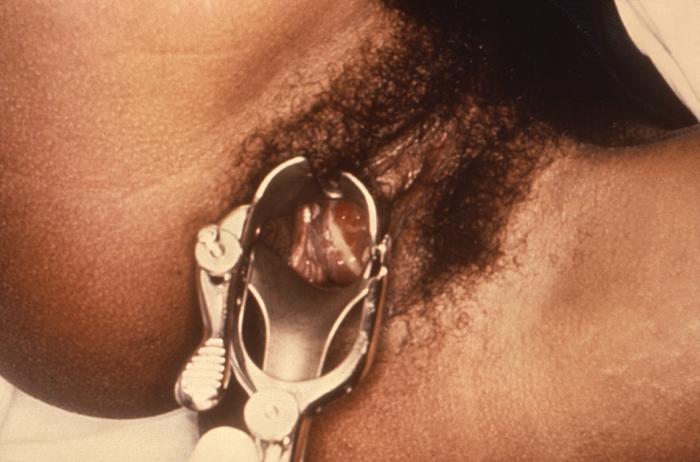
The following are images associated with gonorrhea physical examination.[14][15]
-
Gonococcal ophthalmia is due the pathogenic bacteria Neisseria gonorrhea
-
Gonococcal urethritis, which result in DGI and lead to gonococcal conjunctivitis
-
Purulent discharge emanating from the cervical os, and pooling in the vagina
-
Penile discharge in a patient with gonorrhea
-
Gonococcal pharyngitis
-
Swollen testes consistent with epididymitis in a patient with gonorrhea
-
Gonococcal infection of the conjunctiva in a neonate
-
Cutaneous gonococcal lesion due to a disseminated Neisseria gonorrhea
-
The lesion on the left hand due to the systemic dissemination of the Neisseria gonorrhea.
-
Gonococcal arthritis, inflammation of the skin due to a disseminated gonococcal infection
-
Close-up of a gonococcal lesion on the skin of a patient’s arm
-
Lesions of skin and arthritic knee joints due to Neisseria gonorrhea
-
Gonococcal arthritis of the hand
References
- ↑ 1.0 1.1 1.2 1.3 Workowski KA, Bolan GA, Centers for Disease Control and Prevention (2015). "Sexually transmitted diseases treatment guidelines, 2015". MMWR Recomm Rep. 64 (RR-03): 1–137. PMID 26042815.
- ↑ 2.0 2.1 Sherrard J, Barlow D (1996). "Gonorrhoea in men: clinical and diagnostic aspects". Genitourin Med. 72 (6): 422–6. PMC 1195730. PMID 9038638.
- ↑ 3.0 3.1 Barlow D, Phillips I (1978). "Gonorrhoea in women. Diagnostic, clinical, and laboratory aspects". Lancet. 1 (8067): 761–4. PMID 76760.
- ↑ 4.0 4.1 4.2 Rice PA (2005). "Gonococcal arthritis (disseminated gonococcal infection)". Infect Dis Clin North Am. 19 (4): 853–61. doi:10.1016/j.idc.2005.07.003. PMID 16297736.
- ↑ Huppert JS, Biro F, Lan D, Mortensen JE, Reed J, Slap GB (2007). "Urinary symptoms in adolescent females: STI or UTI?". J Adolesc Health. 40 (5): 418–24. doi:10.1016/j.jadohealth.2006.12.010. PMC 1976261. PMID 17448399.
- ↑ Eschenbach DA, Buchanan TM, Pollock HM, Forsyth PS, Alexander ER, Lin JS; et al. (1975). "Polymicrobial etiology of acute pelvic inflammatory disease". N Engl J Med. 293 (4): 166–71. doi:10.1056/NEJM197507242930403. PMID 806017.
- ↑ Risser WL, Risser JM, Benjamins LJ, Feldmann JM (2007). "Incidence of Fitz-Hugh-Curtis syndrome in adolescents who have pelvic inflammatory disease". J Pediatr Adolesc Gynecol. 20 (3): 179–80. doi:10.1016/j.jpag.2006.08.004. PMID 17561186.
- ↑ Rees E (1967). "Gonococcal bartholinitis". Br J Vener Dis. 43 (3): 150–6. PMC 1047872. PMID 4963696.
- ↑ Stansfield VA (1980). "Diagnosis and management of anorectal gonorrhoea in women". Br J Vener Dis. 56 (5): 319–21. PMC 1045815. PMID 7427703.
- ↑ Kraus SJ (1Link title979). "Incidence and therapy of gonococcal pharyngitis". Sex Transm Dis. 6 (2 Suppl): 143–7. PMID 386537. Check date values in:
|year=(help) - ↑ Osborne NG, Grubin L (1979). "Colonization of the pharynx with Neisseria gonorrhoeae: experience in a clinic for sexually transmitted diseases". Sex Transm Dis. 6 (4): 253–6. PMID 119330.
- ↑ Bleich AT, Sheffield JS, Wendel GD, Sigman A, Cunningham FG (2012). "Disseminated gonococcal infection in women". Obstet Gynecol. 119 (3): 597–602. doi:10.1097/AOG.0b013e318244eda9. PMID 22353959.
- ↑ O'Brien JP, Goldenberg DL, Rice PA (1983). "Disseminated gonococcal infection: a prospective analysis of 49 patients and a review of pathophysiology and immune mechanisms". Medicine (Baltimore). 62 (6): 395–406. PMID 6415361.
- ↑ STD Gonorrhea Infection Gallery http://www.std-gov.org/std_picture/gonorrhea_w.htm Accessed on September 22, 2016
- ↑ Centers for Disease Control and Prevention. Public Health Image Library (PHIL) http://phil.cdc.gov/phil/home.asp Accessed on September 22, 2016