Gonorrhea physical examination: Difference between revisions
m (Bot: Removing from Primary care) |
|||
| (46 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Women with gonococcal infection usually appear to be well until complications such as [[Pelvic inflammatory disease|PID]] develop. Physical examination of women with gonococcal infection is usually remarkable for [[mucopurulent discharge|mucopurulent]] [[urethral]], [[cervical]], or [[vaginal]] discharge; friable appearance of the [[cervix]]; and cervical motion tenderness. One common physical examination finding of gonococcal infection in men is [[Mucopurulent discharge|mucopurulent]] urethral discharge. Less commonly, penile edema and epididymal tenderness and edema ([[epididymitis]]) may also be observed as part of complicated gonococcal infection.<ref name="pmid26042815">{{cite journal| author=Workowski KA, Bolan GA, Centers for Disease Control and Prevention| title=Sexually transmitted diseases treatment guidelines, 2015. | journal=MMWR Recomm Rep | year= 2015 | volume= 64 | issue= RR-03 | pages= 1-137 | pmid=26042815 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26042815 }} </ref><ref name="pmid9038638">{{cite journal| author=Sherrard J, Barlow D| title=Gonorrhoea in men: clinical and diagnostic aspects. | journal=Genitourin Med | year= 1996 | volume= 72 | issue= 6 | pages= 422-6 | pmid=9038638 | doi= | pmc=1195730 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9038638 }} </ref><ref name="pmid76760">{{cite journal| author=Barlow D, Phillips I| title=Gonorrhoea in women. Diagnostic, clinical, and laboratory aspects. | journal=Lancet | year= 1978 | volume= 1 | issue= 8067 | pages= 761-4 | pmid=76760 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=76760 }} </ref> | |||
Physical examination of patients with pharyngeal gonococcal infection is usually remarkable for mild pharyngeal exudates and rectal gonococcal infection is usually remarkable for [[Mucopurulent discharge|mucopurulent]] anal discharge. | |||
Physical examination of patients with disseminated gonococcal infection (DGI) is usually remarkable for [[fever]], pustular or vesicular rash, and musculoskeletal findings.<ref name="pmid26042815">{{cite journal| author=Workowski KA, Bolan GA, Centers for Disease Control and Prevention| title=Sexually transmitted diseases treatment guidelines, 2015. | journal=MMWR Recomm Rep | year= 2015 | volume= 64 | issue= RR-03 | pages= 1-137 | pmid=26042815 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26042815 }} </ref><ref name="pmid16297736">{{cite journal| author=Rice PA| title=Gonococcal arthritis (disseminated gonococcal infection). | journal=Infect Dis Clin North Am | year= 2005 | volume= 19 | issue= 4 | pages= 853-61 | pmid=16297736 | doi=10.1016/j.idc.2005.07.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16297736 }} </ref> | |||
==Physical examination== | ==Physical examination== | ||
| Line 20: | Line 24: | ||
* Bull-headed clap (penile edema) | * Bull-headed clap (penile edema) | ||
* Unilateral epididymal tenderness and edema ([[epididymitis]]) | * Unilateral epididymal tenderness and edema ([[epididymitis]]) | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" | '''Urogenital infection in women''':<ref name="pmid26042815">{{cite journal| author=Workowski KA, Bolan GA, Centers for Disease Control and Prevention| title=Sexually transmitted diseases treatment guidelines, 2015. | journal=MMWR Recomm Rep | year= 2015 | volume= 64 | issue= RR-03 | pages= 1-137 | pmid=26042815 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26042815 }} </ref><ref name="pmid76760">{{cite journal| author=Barlow D, Phillips I| title=Gonorrhoea in women. Diagnostic, clinical, and laboratory aspects. | journal=Lancet | year= 1978 | volume= 1 | issue= 8067 | pages= 761-4 | pmid=76760 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=76760 }} </ref><ref name="pmid17448399">{{cite journal| author=Huppert JS, Biro F, Lan D, Mortensen JE, Reed J, Slap GB| title=Urinary symptoms in adolescent females: STI or UTI? | journal=J Adolesc Health | year= 2007 | volume= 40 | issue= 5 | pages= 418-24 | pmid=17448399 | doi=10.1016/j.jadohealth.2006.12.010 | pmc=1976261 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17448399 }} </ref><ref name="pmid806017">{{cite journal| author=Eschenbach DA, Buchanan TM, Pollock HM, Forsyth PS, Alexander ER, Lin JS et al.| title=Polymicrobial etiology of acute pelvic inflammatory disease. | journal=N Engl J Med | year= 1975 | volume= 293 | issue= 4 | pages= 166-71 | pmid=806017 | doi=10.1056/NEJM197507242930403 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=806017 }} </ref><ref name="pmid17561186">{{cite journal| author=Risser WL, Risser JM, Benjamins LJ, Feldmann JM| title=Incidence of Fitz-Hugh-Curtis syndrome in adolescents who have pelvic inflammatory disease. | journal=J Pediatr Adolesc Gynecol | year= 2007 | volume= 20 | issue= 3 | pages= 179-80 | pmid=17561186 | doi=10.1016/j.jpag.2006.08.004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17561186 }} </ref><ref name="pmid4963696">{{cite journal| author=Rees E| title=Gonococcal bartholinitis. | journal=Br J Vener Dis | year= 1967 | volume= 43 | issue= 3 | pages= 150-6 | pmid=4963696 | doi= | pmc=1047872 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4963696 }} </ref> | | style="padding: 5px 5px; background: #DCDCDC;" | '''Urogenital infection in women''':<ref name="pmid26042815">{{cite journal| author=Workowski KA, Bolan GA, Centers for Disease Control and Prevention| title=Sexually transmitted diseases treatment guidelines, 2015. | journal=MMWR Recomm Rep | year= 2015 | volume= 64 | issue= RR-03 | pages= 1-137 | pmid=26042815 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26042815 }} </ref><ref name="pmid76760">{{cite journal| author=Barlow D, Phillips I| title=Gonorrhoea in women. Diagnostic, clinical, and laboratory aspects. | journal=Lancet | year= 1978 | volume= 1 | issue= 8067 | pages= 761-4 | pmid=76760 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=76760 }} </ref><ref name="pmid17448399">{{cite journal| author=Huppert JS, Biro F, Lan D, Mortensen JE, Reed J, Slap GB| title=Urinary symptoms in adolescent females: STI or UTI? | journal=J Adolesc Health | year= 2007 | volume= 40 | issue= 5 | pages= 418-24 | pmid=17448399 | doi=10.1016/j.jadohealth.2006.12.010 | pmc=1976261 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17448399 }} </ref><ref name="pmid806017">{{cite journal| author=Eschenbach DA, Buchanan TM, Pollock HM, Forsyth PS, Alexander ER, Lin JS et al.| title=Polymicrobial etiology of acute pelvic inflammatory disease. | journal=N Engl J Med | year= 1975 | volume= 293 | issue= 4 | pages= 166-71 | pmid=806017 | doi=10.1056/NEJM197507242930403 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=806017 }} </ref><ref name="pmid17561186">{{cite journal| author=Risser WL, Risser JM, Benjamins LJ, Feldmann JM| title=Incidence of Fitz-Hugh-Curtis syndrome in adolescents who have pelvic inflammatory disease. | journal=J Pediatr Adolesc Gynecol | year= 2007 | volume= 20 | issue= 3 | pages= 179-80 | pmid=17561186 | doi=10.1016/j.jpag.2006.08.004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17561186 }} </ref><ref name="pmid4963696">{{cite journal| author=Rees E| title=Gonococcal bartholinitis. | journal=Br J Vener Dis | year= 1967 | volume= 43 | issue= 3 | pages= 150-6 | pmid=4963696 | doi= | pmc=1047872 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=4963696 }} </ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* [[Mucopurulent discharge|Mucopurulent]] | * [[Mucopurulent discharge|Mucopurulent]] [[urethral]], [[cervical]] or [[vaginal]] discharge | ||
* Positive cervical motion tenderness | * Positive cervical motion tenderness | ||
* Friable cervical mucosa | * Friable cervical mucosa | ||
| Line 41: | Line 43: | ||
| style="padding: 5px 5px; background: #DCDCDC;" | '''Pharyngitis'''<ref name="pmid386537">{{cite journal| author=Kraus SJ| title=Incidence and therapy of gonococcal pharyngitis. | journal=Sex Transm Dis | year= 1[[Link title]]979 | volume= 6 | issue= 2 Suppl | pages= 143-7 | pmid=386537 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=386537 }} </ref><ref name="pmid119330">{{cite journal| author=Osborne NG, Grubin L| title=Colonization of the pharynx with Neisseria gonorrhoeae: experience in a clinic for sexually transmitted diseases. | journal=Sex Transm Dis | year= 1979 | volume= 6 | issue= 4 | pages= 253-6 | pmid=119330 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=119330 }} </ref> | | style="padding: 5px 5px; background: #DCDCDC;" | '''Pharyngitis'''<ref name="pmid386537">{{cite journal| author=Kraus SJ| title=Incidence and therapy of gonococcal pharyngitis. | journal=Sex Transm Dis | year= 1[[Link title]]979 | volume= 6 | issue= 2 Suppl | pages= 143-7 | pmid=386537 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=386537 }} </ref><ref name="pmid119330">{{cite journal| author=Osborne NG, Grubin L| title=Colonization of the pharynx with Neisseria gonorrhoeae: experience in a clinic for sexually transmitted diseases. | journal=Sex Transm Dis | year= 1979 | volume= 6 | issue= 4 | pages= 253-6 | pmid=119330 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=119330 }} </ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | * Pharyngeal exudates | ||
* [[lymphadenitis|Cervical lymphadenitis]] | * [[lymphadenitis|Cervical lymphadenitis]] | ||
|- | |- | ||
| Line 51: | Line 53: | ||
**Periorbital edema | **Periorbital edema | ||
**Corneal involvement | **Corneal involvement | ||
*Neonatal | *[[Neonatal conjunctivitis]] | ||
**[[Chemosis]] | **[[Chemosis]] | ||
**Severe lid edema | **Severe lid edema | ||
| Line 59: | Line 61: | ||
===Disseminated Gonococcal Infection=== | ===Disseminated Gonococcal Infection=== | ||
Dissemination gonococcal infection can result two clinical syndromes: | Dissemination gonococcal infection usually can result in two clinical syndromes:<ref name="pmid16297736">{{cite journal| author=Rice PA| title=Gonococcal arthritis (disseminated gonococcal infection). | journal=Infect Dis Clin North Am | year= 2005 | volume= 19 | issue= 4 | pages= 853-61 | pmid=16297736 | doi=10.1016/j.idc.2005.07.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16297736 }} </ref><ref name="pmid22353959">{{cite journal| author=Bleich AT, Sheffield JS, Wendel GD, Sigman A, Cunningham FG| title=Disseminated gonococcal infection in women. | journal=Obstet Gynecol | year= 2012 | volume= 119 | issue= 3 | pages= 597-602 | pmid=22353959 | doi=10.1097/AOG.0b013e318244eda9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22353959 }} </ref><ref name="pmid6415361">{{cite journal| author=O'Brien JP, Goldenberg DL, Rice PA| title=Disseminated gonococcal infection: a prospective analysis of 49 patients and a review of pathophysiology and immune mechanisms. | journal=Medicine (Baltimore) | year= 1983 | volume= 62 | issue= 6 | pages= 395-406 | pmid=6415361 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6415361 }} </ref> | ||
*Septic arthritis (purulent arthritis) | *[[Septic arthritis]] (purulent arthritis) | ||
*Arthritis-dermatitis syndromes (with a triad of [[tenosynovitis]], [[dermatitis]], and [[polyarthralgias]]) | *Arthritis-dermatitis syndromes (with a triad of [[tenosynovitis]], [[dermatitis]], and [[polyarthralgias]]) | ||
Other less common manifestations of disseminated gonococcal infection include: | Other, less common manifestations of disseminated gonococcal infection include: | ||
*Endocarditis | *[[Endocarditis]] | ||
*Meningitis | *[[Meningitis]] | ||
Physical examination of patients with disseminated gonococcal infection is usually remarkable for:<ref name="pmid26042815">{{cite journal| author=Workowski KA, Bolan GA, Centers for Disease Control and Prevention| title=Sexually transmitted diseases treatment guidelines, 2015. | journal=MMWR Recomm Rep | year= 2015 | volume= 64 | issue= RR-03 | pages= 1-137 | pmid=26042815 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26042815 }} </ref><ref name="pmid16297736">{{cite journal| author=Rice PA| title=Gonococcal arthritis (disseminated gonococcal infection). | journal=Infect Dis Clin North Am | year= 2005 | volume= 19 | issue= 4 | pages= 853-61 | pmid=16297736 | doi=10.1016/j.idc.2005.07.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16297736 }} </ref> | |||
Physical examination of patients with disseminated gonococcal infection is usually remarkable for: | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px;" align=center | ||
| Line 122: | Line 123: | ||
*'''[[Endocarditis]]''' | *'''[[Endocarditis]]''' | ||
**New murmur | **New murmur | ||
**Tachycardia | **[[Tachycardia]] | ||
|} | |} | ||
==Images== | |||
The following are images associated with gonorrhea physical examination.<ref>STD Gonorrhea Infection Gallery http://www.std-gov.org/std_picture/gonorrhea_w.htm Accessed on September 22, 2016</ref><ref name=CDCGonorrheapic>Centers for Disease Control and Prevention. Public Health Image Library (PHIL) http://phil.cdc.gov/phil/home.asp Accessed on September 22, 2016</ref> | |||
<div align="center"> | |||
<gallery heights="175" widths="175"> | |||
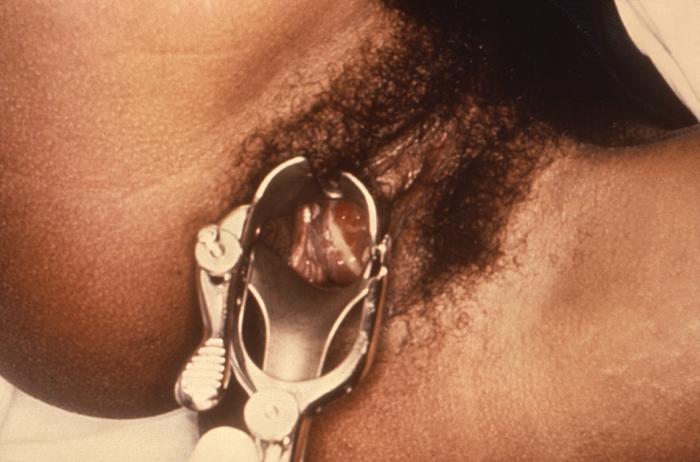
Image: Gonorrhea07.jpeg|Purulent discharge emanating from the cervical os, and pooling in the vagina - Source: https://www.cdc.gov/ | |||
Image:Gonorrhea penile discharge.jpg|Penile discharge in a patient with gonorrhea - Source: https://www.std.gov/ | |||
Image:Gonorrhea20.jpg|Gonococcal pharyngitis - Source: https://www.cdc.gov/ | |||
Image:220px-Gonococcal_ophthalmia_neonatorum.jpg|[[Ophthalmia neonatorum]] - Source: https://www.cdc.gov/ | |||
Image:Gonorrhea36.jpg|Close-up of a gonococcal lesion on the skin of a patient’s arm - Source: https://www.cdc.gov/ | |||
Image:Gonorrhea35.jpg|Lesions of skin and arthritic knee joints due to Neisseria gonorrhea - Source: https://www.cdc.gov/ | |||
Image:Gonorrhea3.jpg|Gonococcal arthritis of the hand - Source: https://www.cdc.gov/ | |||
</gallery> | </gallery> | ||
</div> | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Gynecology]] | |||
[[Category:FinalQCRequired]] | |||
[[Category:Emergency mdicine]] | |||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | |||
[[Category:Rheumatology]] | |||
[[Category:Dermatology]] | |||
[[Category:Neurology]] | |||
[[Category:Cardiology]] | |||
[[Category:Urology]] | |||
[[Category:Gastroenterology]] | |||
Latest revision as of 21:55, 29 July 2020
|
Gonorrhea Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gonorrhea physical examination On the Web |
|
American Roentgen Ray Society Images of Gonorrhea physical examination |
|
Risk calculators and risk factors for Gonorrhea physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Mehrsefat, M.D. [2]
Overview
Women with gonococcal infection usually appear to be well until complications such as PID develop. Physical examination of women with gonococcal infection is usually remarkable for mucopurulent urethral, cervical, or vaginal discharge; friable appearance of the cervix; and cervical motion tenderness. One common physical examination finding of gonococcal infection in men is mucopurulent urethral discharge. Less commonly, penile edema and epididymal tenderness and edema (epididymitis) may also be observed as part of complicated gonococcal infection.[1][2][3]
Physical examination of patients with pharyngeal gonococcal infection is usually remarkable for mild pharyngeal exudates and rectal gonococcal infection is usually remarkable for mucopurulent anal discharge. Physical examination of patients with disseminated gonococcal infection (DGI) is usually remarkable for fever, pustular or vesicular rash, and musculoskeletal findings.[1][4]
Physical examination
Common urogenital and extragenital Infection
The most common site of gonococcal infection is the urethra, endocervix, rectum, and pharynx. Physical examination of patients with gonococcal infection is usually remarkable for:
| Type of Gonococcal Infection | Physical Examination |
|---|---|
| Urogenital infection in men[2] |
|
| Urogenital infection in women:[1][3][5][6][7][8] |
|
| Proctitis[9] |
|
| Pharyngitis[10][11] |
|
| Conjunctivitis |
|
Disseminated Gonococcal Infection
Dissemination gonococcal infection usually can result in two clinical syndromes:[4][12][13]
- Septic arthritis (purulent arthritis)
- Arthritis-dermatitis syndromes (with a triad of tenosynovitis, dermatitis, and polyarthralgias)
Other, less common manifestations of disseminated gonococcal infection include:
Physical examination of patients with disseminated gonococcal infection is usually remarkable for:[1][4]
| Disseminated Gonococcal Infection | Organ systems |
|---|---|
| General Appearance |
Note: Occurs in the acute phase of infection |
| Skin |
|
| Eye |
|
| Musculoskeletal |
Note: purulent arthritis may be abrupt onset of monoarthritis or oligoarthritis without skin lesions and fever
Note: most commonly occurs in hands and less commonly lower extremities
|
| Central Nervous System |
|
| Cardiac |
|
Images
The following are images associated with gonorrhea physical examination.[14][15]
-
Purulent discharge emanating from the cervical os, and pooling in the vagina - Source: https://www.cdc.gov/
-
Penile discharge in a patient with gonorrhea - Source: https://www.std.gov/
-
Gonococcal pharyngitis - Source: https://www.cdc.gov/
-
Ophthalmia neonatorum - Source: https://www.cdc.gov/
-
Close-up of a gonococcal lesion on the skin of a patient’s arm - Source: https://www.cdc.gov/
-
Lesions of skin and arthritic knee joints due to Neisseria gonorrhea - Source: https://www.cdc.gov/
-
Gonococcal arthritis of the hand - Source: https://www.cdc.gov/
References
- ↑ 1.0 1.1 1.2 1.3 Workowski KA, Bolan GA, Centers for Disease Control and Prevention (2015). "Sexually transmitted diseases treatment guidelines, 2015". MMWR Recomm Rep. 64 (RR-03): 1–137. PMID 26042815.
- ↑ 2.0 2.1 Sherrard J, Barlow D (1996). "Gonorrhoea in men: clinical and diagnostic aspects". Genitourin Med. 72 (6): 422–6. PMC 1195730. PMID 9038638.
- ↑ 3.0 3.1 Barlow D, Phillips I (1978). "Gonorrhoea in women. Diagnostic, clinical, and laboratory aspects". Lancet. 1 (8067): 761–4. PMID 76760.
- ↑ 4.0 4.1 4.2 Rice PA (2005). "Gonococcal arthritis (disseminated gonococcal infection)". Infect Dis Clin North Am. 19 (4): 853–61. doi:10.1016/j.idc.2005.07.003. PMID 16297736.
- ↑ Huppert JS, Biro F, Lan D, Mortensen JE, Reed J, Slap GB (2007). "Urinary symptoms in adolescent females: STI or UTI?". J Adolesc Health. 40 (5): 418–24. doi:10.1016/j.jadohealth.2006.12.010. PMC 1976261. PMID 17448399.
- ↑ Eschenbach DA, Buchanan TM, Pollock HM, Forsyth PS, Alexander ER, Lin JS; et al. (1975). "Polymicrobial etiology of acute pelvic inflammatory disease". N Engl J Med. 293 (4): 166–71. doi:10.1056/NEJM197507242930403. PMID 806017.
- ↑ Risser WL, Risser JM, Benjamins LJ, Feldmann JM (2007). "Incidence of Fitz-Hugh-Curtis syndrome in adolescents who have pelvic inflammatory disease". J Pediatr Adolesc Gynecol. 20 (3): 179–80. doi:10.1016/j.jpag.2006.08.004. PMID 17561186.
- ↑ Rees E (1967). "Gonococcal bartholinitis". Br J Vener Dis. 43 (3): 150–6. PMC 1047872. PMID 4963696.
- ↑ Stansfield VA (1980). "Diagnosis and management of anorectal gonorrhoea in women". Br J Vener Dis. 56 (5): 319–21. PMC 1045815. PMID 7427703.
- ↑ Kraus SJ (1Link title979). "Incidence and therapy of gonococcal pharyngitis". Sex Transm Dis. 6 (2 Suppl): 143–7. PMID 386537. Check date values in:
|year=(help) - ↑ Osborne NG, Grubin L (1979). "Colonization of the pharynx with Neisseria gonorrhoeae: experience in a clinic for sexually transmitted diseases". Sex Transm Dis. 6 (4): 253–6. PMID 119330.
- ↑ Bleich AT, Sheffield JS, Wendel GD, Sigman A, Cunningham FG (2012). "Disseminated gonococcal infection in women". Obstet Gynecol. 119 (3): 597–602. doi:10.1097/AOG.0b013e318244eda9. PMID 22353959.
- ↑ O'Brien JP, Goldenberg DL, Rice PA (1983). "Disseminated gonococcal infection: a prospective analysis of 49 patients and a review of pathophysiology and immune mechanisms". Medicine (Baltimore). 62 (6): 395–406. PMID 6415361.
- ↑ STD Gonorrhea Infection Gallery http://www.std-gov.org/std_picture/gonorrhea_w.htm Accessed on September 22, 2016
- ↑ Centers for Disease Control and Prevention. Public Health Image Library (PHIL) http://phil.cdc.gov/phil/home.asp Accessed on September 22, 2016