Clostridium difficile infection
| Clostridium difficile | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
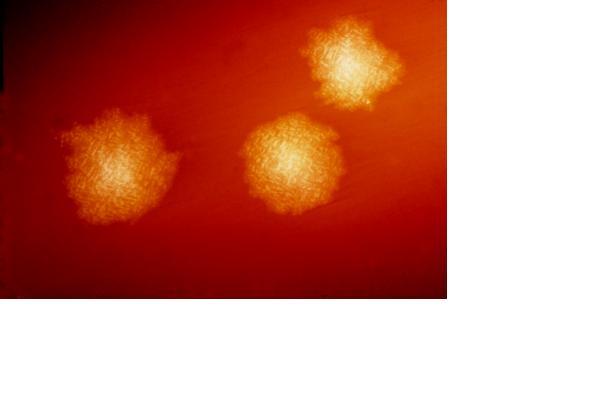 C. difficile colonies on a blood agar plate.
| ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Clostridium difficile Hall & O'Toole, 1935 |
|
Clostridium difficile Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Clostridium difficile infection On the Web |
|
American Roentgen Ray Society Images of Clostridium difficile infection |
|
Risk calculators and risk factors for Clostridium difficile infection |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor(s)-in-Chief: Abhishek Deshpande, M.D., PhD
Synonyms and keywords: C. Diff
Overview
Clostridium difficile or CDF/cdf' is a species of bacteria of the genus Clostridium which are Gram-positive, anaerobic, spore-forming rods (bacillus).[1] Clostridium difficile (C. diff) is one of the most common hospital-acquired infections, particularly in elderly hospitalized patients, and also one of the most common complications of antibiotics in hospitalized patients. Patients are rarely infected unless the normal flora of the intestinal tract has been altered by antibiotics. Up to 10% of patients hospitalized >2 days are affected.Of note, most antibiotic-associated diarrhea is not due to C. diff, but is due to an osmotic type diarrhea. The antibiotics wipe out the gastrointestinal (GI) tract’s normal flora, which usually break down unabsorbed carbohydrates. These unabsorbed carbohydrates remain in the lumen and carry with them water, resulting in diarrhea.C. difficile is the most significant cause of pseudomembranous colitis,[2] a severe infection of the colon, often after normal gut flora is eradicated by the use of antibiotics. Treatment is by stopping any antibiotics and commencing specific anticlostridial antibiotics, e.g. metronidazole.
Pathophysiology & Etiology
Bacteriology
Clostridia are motile bacteria that are ubiquitous in nature and are especially prevalent in soil. Under the microscope after Gram staining, they appear as long drumsticks with a bulge located at their terminal ends. Clostridium difficile cells are Gram positive. Clostridium shows optimum growth when plated on blood agar at human body temperatures. When the environment becomes stressed, however, the bacteria produce spores that tolerate the extreme conditions that the active bacteria cannot. First described by Hall and O'Toole in 1935, "the difficult clostridium" was resistant to early attempts at isolation and grew very slowly in culture.[3] C. difficile is a commensal bacterium of the human intestine in a minority of the population. . In small numbers it does not result in disease of any significance. Antibiotics, especially those with a broad spectrum of activity, cause disruption of normal intestinal flora, leading to an overgrowth of C. difficile. This leads to pseudomembranous colitis.
C. difficile is resistant to most antibiotics. It flourishes under these conditions. It is transmitted from person to person by the fecal-oral route. Because the organism forms heat-resistant spores, it can remain in the hospital or nursing home environment for long periods of time. It can be cultured from almost any surface in the hospital. Once spores are ingested, they pass through the stomach unscathed because of their acid-resistance. They change to their active form in the colon and multiply. It has been observed that several disinfectants commonly used in hospitals may fail to kill the bacteria, and may actually promote spore formation. However, disinfectants containing bleach are effective in killing the organisms[4].
Patients are rarely infected unless the normal flora of the intestinal tract has been altered by antibiotics. Following colonization C. diff releases two cytotoxins, A and B:
- The cytotoxins bind to receptors on intestinal epithelial cells.
- The cytotoxins usually result in acute inflammatory infiltrate, leading to cell necrosis and shedding.
- A shallow ulcer results, from which serum proteins, mucus, and inflammatory cells emanate, leading to the appearance of a pseudomembrane.
- Some strains do not produce toxin.
Toxins
Pathogenic C. difficile strains produce various toxins. The most well-characterized are enterotoxin (toxin A) and cytotoxin (toxin B).[1] These two toxins are both responsible for the diarrhea and inflammation seen in infected patients, although their relative contributions have been debated by researchers. Another toxin, binary toxin, has also been described, but its role in disease is not yet fully understood.[5]
Role in disease
With the introduction of broad-spectrum antibiotics in the latter half of the twentieth century, antibiotic-associated diarrhea became more common. Pseudomembranous colitis was first described as a complication of C. difficile infection in 1978,[6] when a toxin was isolated from patients suffering from pseudomembranous colitis and Koch's postulates were met.
Clostridium Difficile Infection (CDI), can range in severity from asymptomatic to severe and life threatening, and many deaths have been reported, especially amongst the aged. People are most often infected in hospitals, nursing homes, or institutions, although C. difficile infection in the community, outpatient setting is increasing. Clostridium difficile associated diarrhea (aka CDAD) has been linked to use of broad-spectrum antibiotics such as cephalosporins and clindamycin, though the use of quinolones is now probably the most likely culprit, which are frequently used in hospital settings. Frequency and severity of C. difficile colitis remains high and seems to be associated with increased death rates. Immunocompromised status and delayed diagnosis appear to result in elevated risk of death. Early intervention and aggressive management are key factors to recovery.
The rate of Clostridium difficile acquisition is estimated to be 13 percent in patients with hospital stays of up to two weeks and 50 percent in those with hospital stays longer than four weeks.
Increasing rates of community-acquired Clostridium difficile-associated infection/disease (CDAD) has also been linked to the use of medication to suppress gastric acid production: H2-receptor antagonists increased the risk twofold, and proton pump inhibitors threefold, mainly in the elderly. It is presumed that increased gastric pH, (alkalinity), leads to decreased destruction of spores.[7]
Genetics
On December 14, 2005, researchers at McGill University in Montreal, Quebec, led by Dr. Ken Dewar and Dr. Andre Dascal and in collaboration with province-organized NPO Genome Quebec's research facility, announced they had cracked the genetic code of the highly virulent Quebec strain of C. difficile. This was accomplished by using ultra high-throughput sequencing technology. The tests involved doing 400,000 DNA parallel sequencing reactions which took the bacterium's genome apart and reassembled it so it could be studied.[8][9]
It is expected this will allow quicker detection of the disease and better treatment.
Risk Factors
- Most antibiotics, including metronidazole, can be associated with C. diff infection, though the most commonly implicated are ampicillin, clindamycin, and the cephalosporins. Antibiotics only rarely associated with infection include parenteral antibiotics, tetracyclines, chloramphenicol, metronidazole and vancomycin. Onset is usually during or shortly after a course of antibiotics.
- Patients who have been staying long-term in a hospital or a nursing home have a higher likelihood of being colonized by this bacterium. Hospitalized patients are more likely to infected if their roommates are infected. C. diff can be cultured from many surfaces in the hospital room, and spores have been identified everywhere, including toilets, floors, mops, scales, furniture, etc. Health care workers commonly carry the organism on their hands, clothing and stethoscopes, though they are not usually fecal carriers.
- Hospital outbreaks are common.
- Newborns are often infected, but are asymptomatic. By 24 months of age, over half of toddlers have immunoglobulins to toxins A and B.
Diagnosis
Often clinicians begin treatment before results have come back based on clinical presentation to prevent complications. Knowledge of the local epidemiology of intestinal flora of a particular institution can guide therapy.
In adults, a clinical prediction rule found the best signs are[10] :
- significant diarrhea ("new onset of > 3 partially formed or watery stools per 24 hour period")
- exposure of antibiotics
- abdominal pain
- foul stool odor
The presence of any one of these findings has a sensitivity of 86% and a specificity of 45%.[10] In this study of hospitalized patients with a prevalence of positive cytotoxin assays of 14%, the positive predictive value was 20% and the negative predictive value was 95%.
History and Symptoms
Clinical manifestations can be quite variable. Some patients are asymptomatic, and others can present critically ill with toxic megacolon.
- Up to 2/3 of infected hospitalized patients are asymptomatic, but shed organisms and contaminate their environment. These patients are called C. Diff fecal excretors. These patients can be treated with vancomycin or metronidazole, but the bug is often not eradicated in these patients.
- The reason for the variability is not clear and is not accounted for by strain differences. Host factors are probably important, such as the presence of antitoxin antibodies and colonic toxin receptors.
- Risk factors for severe colitis include malignancy, Chronic Obstructive Pulmonary Disease (COPD), immunosuppression, renal failure, exposure to anti-peristaltic meds and clindamycin.
- Onset is usually during or shortly after a course of antibiotics. Cases rarely occur even a month after a course of antibiotics. Rarely patients have no recent history of antibiotics.
Antibiotic-associated diarrhea with C. diff infection, but without colitis
- Acute, foul-smelling watery diarrhea, with a mean of 3-4 stools a day.
- Lower abdominal pain, sometimes crampy
- Low-grade fever
Antibiotic-associated diarrhea with C. diff infection with colitis, but without pseudomembrane development In addition to profuse, watery diarrhea of 5-15 bowel movements daily, the patients suffer from:
- Fever
- Malaise
- Anorexia
- Lower quadrant abdominal pain and cramps, relieved by the passage of diarrhea.
- Nausea
- Dehydration
- Leucocytosis
- Fecal leucocytes present in >50%. Occult bleeding not uncommon.
- Sigmoidoscopy shows a nonspecific diffuse or patchy erthrematous colitis without pseudomembranes.
Antibiotic-associated diarrhea with C. diff infection with colitis and pseudomembrane development Patients tend to have the prominent signs as symptoms described above.
- Rarely patients will develop indolent, subacute pseudomembranous colitis with a protein-losing state due to the diffuse pancolitis. Patients may have severe hypoalbuminemia, ascites, peripheral edema, and their only signs/symptoms may be low-grade fever, anorexia and abdominal discomfort.
- Sigmoidoscopy shows pseudomembranes; raised yellow or off-white plaques ranging up to 1 cm in diameter scattered over the colorectal mucosa.
- Occasionally pseudomembranes will be located in the proximal colon.
Fulminant colitis
Fulminant colitis is an uncommon complication that occurs in 2-3% of patients with C. Diff, and can results in perforation, prolonged ileus, megacolon, and death.
Patients may present with:
- Severe abdominal pain and distension
- Severe diarrhea; diarrhea may be absent in patients with ileus
- Fever, chills
- Lethargy
- Tachycardia
- Leucocytosis, up to 40,000 mm3
- Metabolic acidosis
Toxic megcolon is an enlarged, dilated colon >7cm associated severe systemic toxicity.
- Small intestinal dilation may also occur
- Air-fluid levels may be present
- Submucosal edema may result in thumb-printing
Laboratory Findings
Cytotoxicity assay
C. difficile toxin detection as cytopathic effect in cell culture, and neutralized with specific anti-sera is the practical gold standard for studies investigating new CDAD diagnostic techniques. Toxigenic culture, in which organisms are cultured on selective medium and tested for toxin production remains the gold standard and is the most sensitive and specific test, although it is slow and labour-intensive.[11]
Enzyme-linked immunoabsorbant assay (ELISA) for toxin
Assessment of the A and B toxins by enzyme-linked immunoabsorbant assay (ELISA) for toxin A or B (or both) has:
- sensitivity 63-99%
- specificity 93-100%
At a prevalence of 15%, this leads to:
Experts recommend sending as many as three samples to rule-out disease if initial tests are negative. C. difficile toxin should clear from the stool of previously infected patients if treatment is effective.
Unfortunately, many hospitals only test for the prevalent toxin A. Strains that express only the B toxin are now present in many hospitals and ordering both toxins should occur. Not testing for both may contribute to a delay in obtaining laboratory results, which is often the cause of prolonged illness and poor outcomes.
Other stool tests
Stool leukocyte measurements and stool lactoferrin levels have also been proposed as diagnostic tests, but may have limited diagnostic accuracy.[12]
Computed tomography
In a recent study, a patient who received a diagnosis of CDC on the basis of computed tomography (CT scan) had an 88% probability of testing positive on stool assay.[13] Wall thickening is the key CT finding in this disease. Once colon wall thickening is identified as being >4 mm, the best ancillary findings were:
- pericolonic stranding
- ascites
- colon wall nodularity
The presence of wall thickness plus any one of these ancillary findings yields:
- sensitivity of 70%
- specificity of 93%
Using criteria of >=10 mm or a wall thickness of >4 mm and any of the more-specific findings does not add significantly to the diagnosis but gives equally satisfactory results. In this study with a prevalence of positive C. difficile toxin of 54%, the positive predictive value was 88%. Patients who have antibiotic-associated diarrhea who have CT findings diagnostic of CDC merit consideration for treatment on that basis. A weakness of this study was not using a gold standard cytotoxicity assay.
Endoscopy
Endoscopy may be indicated for quick diagnosis of pseudomembranous colitis or in atypical cases.
Treatment
Many persons will also be asymptomatic and colonized with Clostridium difficile. Treatment in asymptomatic patients is controversial, also leading into the debate of clinical surveillance and how it intersects with public health policy.
It is possible that mild cases do not need treatment.[14]
Patients should be treated as soon as possible when the diagnosis of Clostridium difficile colitis (CDC) is made to avoid frank sepsis or bowel perforation.
Pharmacotherapy
Three antibiotics are effective against C. difficile.
- Metronidazole 500mg orally three times daily is the drug of choice, because of superior tolerability, lower price and comparable efficacy[15]. Metronidazole is taken up by the GI tract, unlike vancomycin. Some therefore recommend prescriptions of severe cases with vancomycin, to insure adequate levels. IV metronidazole 500 mg TID is also effective.
- Oral vancomycin 125 mg four times daily is second-line therapy, but is avoided due to theoretical concerns of converting intestinal flora into vancomycin resistant organisms. However, it is used in the following cases: severe C. difficile diarrhea[16] (the duration of diarrhea is reduced to 3 versus 4.6 days with metronidazole; no response to oral metronidazole; the organism is resistant to metronidazole; the patient is allergic to metronidazole; the patient is either pregnant or younger than 10 years of age. Vancomycin must be administered orally because IV administration does not achieve gut lumen minimum therapeutic concentration.
- The use of linezolid may be considered too.
It has been known that drugs traditionally used to stop diarrhea worsen the course of C. difficile-related pseudomembranous colitis. Loperamide, diphenoxylate and bismuth compounds are indeed contraindicated, because slowing of fecal transit time is thought to result in extended toxin-associated damage. Cholestyramine, a powder drink occasionally used to lower cholesterol, is effective in binding both Toxin A and B, and slows bowel motility and helps prevent dehydration.[17] The dosage can be 4 grams daily, to up to four doses a day: caution should be exercised to prevent constipation, or drug interactions, most notably the binding of drugs by cholestyramine, preventing their absorption. A last-resort treatment in immunosuppressed patients is intravenous immunoglobulin (IVIG).[17]
Pseudomembranous colitis caused by C. difficile is treated with antibiotics, for example, vancomycin, metronidazole, bacitracin or fusidic acid.
Patients should be treated for 10-14 days, unless the inciting antibiotics can’t be discontinued, in which case metronidazole or vancomycin should be continued for a week or so after discontinuation of the inciting antibiotics. Failure to initially respond is typically not due to resistance, but may be due to misdiagnosis, noncompliance or other GI disease.
Up to 15-20% of patients will relapse after treatment, not typically due to resistant organisms. The exact mechanism has not been clarified; these patients often do not develop as prominent an antibody response, so immune mediated defects may be contributory. Relapse usually is within a few days of discontinued prescription, though may be as long as 30 days afterward. For relapse, patients should receive a second course of metronidazole for 14 days. For a second relapse, a C. diff titer should be checked to confirm the diagnosis, and then a third course of antibiotics should be with vancomycin. For patients with multiple relapses, some recommend a schedule of tapering vancomycin, from full dose down to 125 mg q3 days over the course of 6 weeks. Other potential prescriptions that are not commonly used include prescriptions with cholestyramine, which binds the toxin (but will also bind vancomycin), and attempts to repopulate the gut with organisms.
Fecal bacteriotherapy
Fecal bacteriotherapy, a procedure related to probiotic research, has been suggested as a potential cure for the disease. It involves infusion of bacterial flora acquired from the feces of a healthy donor in an attempt to reverse bacterial imbalance responsible for the recurring nature of the infection. It has a success rate of nearly 95% according to some sources.[18][19][20]
Surgery and Device Based Therapy
Patients with signs/symptoms of fulminant colitits should be evaluated by surgery for possible urgent surgery for bowel perforation, impending perforation, severe ileus with megacolon, or refractory septicemia.
Indications for Surgery
Indications for surgery include:
- Peritoneal signs
- Persistent bacteremia
- Progressive disease
- CT showing pericolonic inflammation with increasing bowel wall edema.
Colectomy
In those patients that develop systemic symptoms of CDC, colectomy may improve the outcome if performed before the need for vasopressors. The usual intervention is a subtotal colectomy with ileostomy.
Recurrence
The evolution of protocols for patients with recurrent C. difficile diarrhea also present a challenge: there is no known proper length of time or universally accepted alternative drugs with which one should be treated. However, re-treatment with metronidazole or vancomycin at the previous dose for 10 to 14 days is generally successful. The addition of rifampin to vancomycin also has been effective. Prophylaxis with competing, nonpathogenic organisms such as Lactobacillus spp. or Saccharomyces boulardii has been found to be helpful in preventing relapse in small numbers of patients (see, for example, Florastor, or Lactinex). It is thought that these organisms, also known as probiotics, help to restore the natural flora in the gut and make patients more resistant to colonization by C. difficile.
Prevention
The most effective method for preventing Clostridium difficile associated diarrhea (CDAD) is proper antimicrobial prescribing. In the hospital setting, where CDAD is most common, nearly all patients who develop CDAD are exposed to antimicrobials. Although this sounds easy to do, approximately 50% of antimicrobial use is considered inappropriate. This is consistent whether in the hospital, clinic, community, or academic setting. Several studies have demonstrated a decrease in CDAD by limiting antibitoics most strongly associated with CDAD or by limiting unnecessary antimicrobial prescribing in general, both in outbreak and non-outbreak settings.
Infection control measures, such as wearing gloves when caring for patients with CDAD, have been proven to be effective at preventing CDAD. This works by limiting the spread of C. difficile in the hospital setting.
Treatment with various oral supplements containing live bacteria has been studied in efforts to prevent Clostridium difficile-associated infection/disease. A randomized controlled trial using a probiotic drink containing Lactobacillus casei, L bulgaricus, and Streptococcus thermophilus was reported to have some efficacy. This study was sponsored by the company that produces the drink studied [21]. Although intriguing, several other studies have been unable to demonstrate any benefit of oral supplements of similar bacteria at preventing CDAD. Of note, patients on the antibiotics most strongly associated with CDAD were excluded from this study.
Notable outbreaks
On June 4, 2004, two outbreaks of a highly virulent strain of this bacterium were reported in Montreal, Quebec and Calgary, Alberta, in Canada. Sources put the death count as low as 36 and as high as 89, with approximately 1,400 cases in 2003 and within the first few months of 2004. C. difficile infections continued to be a problem in the Quebec health care system in late 2004. As of March 2005, it had spread into the Toronto, Ontario area, hospitalizing 10 people. One died while the others were being discharged.
A similar outbreak took place at Stoke Mandeville Hospital in the United Kingdom between 2003 and 2005. The local epidemiology of C. difficile may offer clues on how its spread may relate to the amount of time a patient spends in hospital and/or a rehabilitation center. It also samples institutions' ability to detect increased rates, and their capacity to respond with more aggressive hand washing campaigns, quarantine methods, and availability of yoghurt to patients at risk for infection.
It has been suggested that both the Canadian and English outbreaks were related to the seemingly more virulent 027 strain of bacterium. This strain has also been implicated in an epidemic at two Dutch hospitals (Harderwijk and Amersfoort, both 2005). A theory for explaining the increased virulence of 027 is that it is a hyperproducer of both toxin A and B, and that certain antibiotics may actually stimulate the bacteria to hyperproduce.
On December 2, 2005, The New England Journal of Medicine, in an article spearheaded by Drs. Vivian Loo, Louise Poirier, and Mark Miller, reported the emergence of a new, highly toxic strain of C. difficile, resistant to fluoroquinolone antibiotics, such as Cipro (ciprofloxacin) and Levaquin (levofloxacin), said to be causing geographically dispersed outbreaks in North America.[8] The Centers for Disease Control in Atlanta has also warned of the emergence of an epidemic strain with increased virulence, antibiotic resistance, or both.[22]
As one analyzes the pool of patients with the spores, many who are asymptomatic will pass the organism to individuals who are immunocompromised and hence, susceptible to increasing rates of diarrhea and poor outcome. It seems notable that the clusters described above represent a challenge to epidemiologists trying to understand how the illness spreads via the convergence of information technology with clinical surveillance.
On October 1, 2006, the bacteria was said to have killed at least 49 people at hospitals in Leicester, England over eight months, according to a National Health Service investigation. Another 29 similar cases were investigated by coroners.[23] A UK Department of Health memo leaked shortly afterwards revealed significant concern in government about the bacterium, described as being "endemic throughout the health service"[24]
On October 27, 2006, the bacteria was attributed to 9 deaths in Quebec, Canada.[25]
On November 18th, 2006, the bacteria was reported to have been responsible for 12 deaths in Quebec, Canada. This 12th reported death was only two days after the St. Hyacinthe's Honoré Mercier announced that the outbreak was under control. 31 patients were diagnosed with Clostridium difficile and four (as of Sat. Nov 18th) were still under observation. Cleaning crews took measures in an attempt to clear the outbreak.[26]
On February 27, 2007, a new outbreak was identified at Trillium Health Centre in Mississauga Ontario, where 14 people were diagnosed with the bacteria. The bacteria was the same strain as the one in Quebec. Officials have not been able to determine if C. difficile was responsible for deaths of four patients over the prior two months.[27]
In October 2007, Maidstone and Tunbridge Wells NHS Trust was heavily criticized by the Healthcare Commission regarding its handling of a major outbreak of C. difficile in its hospitals in Kent from April 2004 to September 2006. In its report, the Commission estimated that about 90 patients "definitely or probably" died as a result of the infection. [28][29]
References
- ↑ 1.0 1.1 Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. pp. pp. 322-4. ISBN 0-8385-8529-9.
- ↑ "Pseudomembranous Colitis". eMedicine. WebMD. 1 July 2005. Retrieved 2007-01-11.
- ↑ Hall I, O'Toole E (1935). "Intestinal flora in newborn infants with a description of a new pathogenic anaerobe, Bacillus difficilis". Am J Dis Child. 49: 390.
- ↑ "Cleaning agents 'make bug strong'". BBC News Online. 3 April 2006. Retrieved 2007-01-11.
- ↑ Barth H, Aktories K, Popoff M, Stiles B (2004). "Binary bacterial toxins: biochemistry, biology, and applications of common Clostridium and Bacillus proteins". Microbiol Mol Biol Rev. 68 (3): 373–402, table of contents. PMID 15353562.
- ↑ Larson H, Price A, Honour P, Borriello S (1978). "Clostridium difficile and the aetiology of pseudomembranous colitis". Lancet. 1 (8073): 1063–6. PMID 77366.
- ↑ Dial S, Delaney J, Barkun A, Suissa S (2005). "Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease". JAMA. 294 (23): 2989–95. PMID 16414946.
- ↑ 8.0 8.1 Loo V, Poirier L, Miller M, Oughton M, Libman M, Michaud S, Bourgault A, Nguyen T, Frenette C, Kelly M, Vibien A, Brassard P, Fenn S, Dewar K, Hudson T, Horn R, René P, Monczak Y, Dascal A (2005). "A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality". N Engl J Med. 353 (23): 2442–9. PMID 16322602.
- ↑ Scientists map C. difficile strain - Institute of Public Affairs, Montreal
- ↑ 10.0 10.1 Katz DA, Lynch ME, Littenberg B (1996). "Clinical prediction rules to optimize cytotoxin testing for Clostridium difficile in hospitalized patients with diarrhea". Am. J. Med. 100 (5): 487–95. doi:10.1016/S0002-9343(95)00016-X. PMID 8644759.
- ↑ Murray PR, Baron EJ, Pfaller EA, Tenover F, Yolken RH (editors) (2003). Manual of Clinical Microbiology (8th ed ed.). Washington DC: ASM Press. ISBN 1-55581-255-3 Check
|isbn=value: checksum (help). - ↑ Kirkpatrick ID, Greenberg HM (2001). "Evaluating the CT diagnosis of Clostridium difficile colitis: should CT guide therapy?". AJR. American journal of roentgenology. 176 (3): 635–9. PMID 11222194.
- ↑ Nelson R. Antibiotic treatment for Clostridium difficile-associated diarrhea in adults. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD004610. PMID 17636768
- ↑ Teasley DG, Gerding DN, Olson MM, Peterson LR, Gebhard RL, Schwartz MJ, Lee JT Jr. Prospective randomised trial of metronidazole versus vancomycin for Clostridium-difficile-associated diarrhoea and colitis. Lancet. 1983 Nov 5;2(8358):1043-6. PMID 6138597
- ↑ Zar FA, Bakkanagari SR, Moorthi KM, Davis MB (2007). "A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity". Clin. Infect. Dis. 45 (3): 302–7. doi:10.1086/519265. PMID 17599306.
- ↑ 17.0 17.1 Stroehlein J (2004). "Treatment of Clostridium difficile Infection". Curr Treat Options Gastroenterol. 7 (3): 235–239. PMID 15149585.
- ↑ Schwan A, Sjölin S, Trottestam U, Aronsson B (1983). "Relapsing clostridium difficile enterocolitis cured by rectal infusion of homologous faeces". Lancet. 2 (8354): 845. PMID 6137662.
- ↑ Paterson D, Iredell J, Whitby M (1994). "Putting back the bugs: bacterial treatment relieves chronic diarrhoea". Med J Aust. 160 (4): 232–3. PMID 8309401.
- ↑ Borody T (2000). ""Flora Power"-- fecal bacteria cure chronic C. difficile diarrhea" (PDF). Am J Gastroenterol. 95 (11): 3028–9. PMID 11095314.
- ↑ Hickson M, D'Souza AL, Muthu N; et al. (2007). "Use of probiotic Lactobacillus preparation to prevent diarrhoea associated with antibiotics: randomised double blind placebo controlled trial". BMJ. 335 (7610): 80. doi:10.1136/bmj.39231.599815.55. PMID 17604300.
- ↑ McDonald L (2005). "Clostridium difficile: responding to a new threat from an old enemy" (PDF). Infect Control Hosp Epidemiol. 26 (8): 672–5. PMID 16156321.
- ↑ Trust confirms 49 superbug deaths - BBC News
- ↑ Nigel Hawkes (11th January 2007). "Leaked memo reveals that targets to beat MRSA will not be met". The Times. Retrieved 2007-01-11. Check date values in:
|date=(help) - ↑ "C. difficile blamed for 9 death in hospital near Montreal". cNews. 11th January 200. Retrieved 2007-01-11. Check date values in:
|date=(help) - ↑ 12th person dies of C. difficile at Quebec hospital - CBC News
- ↑ [1]
- ↑ Healthcare Commission press release: Healthcare watchdog finds significant failings in infection control at Maidstone and Tunbridge Wells NHS Trust, 11 October 2007
- ↑ Daily Telegraph, Health Secretary intervenes in superbug row, 11 October 2007
The content on this page was first contributed by: Ellison L. Smith, M.D.
Further reading
- Dallal R, Harbrecht B, Boujoukas A, Sirio C, Farkas L, Lee K, Simmons R (2002). "Fulminant Clostridium difficile: an underappreciated and increasing cause of death and complications". Ann Surg. 235 (3): 363–72. PMID 11882758.
- Martin S, Jung R (2005). Gastrointestinal infections and enterotoxigenic poisonings. In: Pharmacotherapy: A Pathophysiologic Approach (DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, editors) (6th ed. ed.). McGraw-Hill. pp. pp. 2042-2043. ISBN.
- McDonald L, Killgore G, Thompson A, Owens R, Kazakova S, Sambol S, Johnson S, Gerding D (2005). "An epidemic, toxin gene-variant strain of Clostridium difficile". N Engl J Med. 353 (23): 2433–41. PMID 16322603.
- Yamada T; Alpers DH (editors) (2003). Textbook of Gastroenterology (4th ed. ed.). Lippincott Williams & Wilkins. pp. pp. 1870-1875. ISBN 0-7817-2861-4.
- van den Hof S, van der Kooi T, van den Berg R, Kuijper E, Notermans D (2006). "Clostridium difficile PCR ribotype 027 outbreaks in the Netherlands: recent surveillance data indicate that outbreaks are not easily controlled but interhospital transmission is limited". Euro Surveill. 11 (1): E060126.2. PMID 16801713.
- Sunenshine R, McDonald L (2006). "Clostridium difficile-associated disease: New challenges from an established pathogen". Cleveland Clinic J. Med. 73: 187.
External links
- UK Clostridium difficile Support Group
- Clostridium difficile Support Group
- "From hand to mouth" Article from The Economist discussing C. difficile (requires subscription)
- Pathema-Clostridium Resource
- US CDC Report on Severe Clostridium difficile--Associated Disease in Populations Previously at Low Risk--Four States, 2005