Cystinosis
| Cystinosis | |
 | |
|---|---|
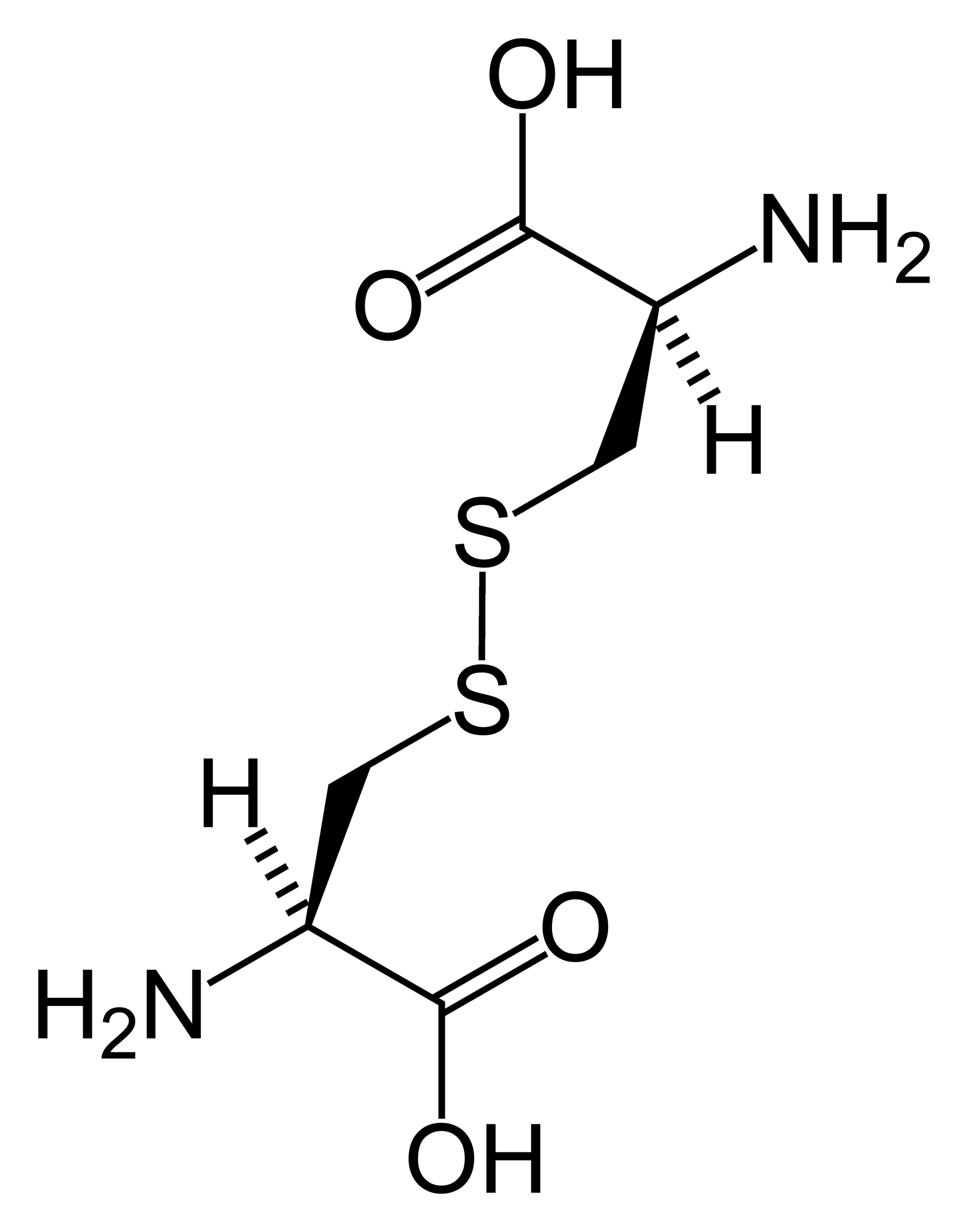
| Chemical structure of cystine formed from L-cysteine (under biological conditions) | |
| ICD-10 | E72.0 |
| ICD-9 | 270.0 |
| DiseasesDB | 3382 |
| eMedicine | ped/538 |
| MeSH | D003554 |
|
WikiDoc Resources for Cystinosis |
|
Articles |
|---|
|
Most recent articles on Cystinosis |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cystinosis at Clinical Trials.gov Clinical Trials on Cystinosis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cystinosis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cystinosis Discussion groups on Cystinosis Patient Handouts on Cystinosis Directions to Hospitals Treating Cystinosis Risk calculators and risk factors for Cystinosis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cystinosis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Cystinosis is a hereditary disorder of the renal tubules characterized by the presence of carbohydrates and amino acids in the urine, excessive urination, and low blood levels of potassium ions and phosphates. The body accumulates the amino acid cystine within cells. Excess cystine forms crystals that can build up and damage cells. These crystals negatively affect many systems in the body, especially the kidneys and eyes.
Historical Perspective
Classification
- Online Mendelian Inheritance in Man (OMIM) 219800 - Infantile nephropathic
- Online Mendelian Inheritance in Man (OMIM) 219900 - Adolescent nephropathic
- Online Mendelian Inheritance in Man (OMIM) 219750 - Adult nonnephropathic
Pathophysiology
Genetics
The cause of cystinosis is due to a mutation in the gene CTNS which codes for cystinosin, the lysosomal cystine transporter. Symptoms are first seen at about 3 to 18 months of age with profound polyuria (excessive urination), followed by poor growth, photophobia, and ultimately kidney failure by age 6 years in the nephropathic form. It is important for the child to see a biochemical geneticist and pediatric nephrologist to begin treatment with cysteamine as early as possible. Cysteamine decreases the amount of cystine stored in lysosomes and correlates with conservation of renal function and improved growth. Cysteamine eyedrops remove the cystine crystals in the cornea that can cause photophobia if left unchecked.
All forms of cystinosis (nephropathic, juvenile and ocular) are inherited as autosomal recessive traits, which means that there is a 25% recurrence risk to any couple who have had an affected child. The disease "breeds true" such that parents of a child with the juvenile variety of cystinosis will not have another child with the nephropathic form, etc. Cystinosis affects approximately 1 in 100,000 to 200,000 newborns. The incidence is higher in the province of Brittany, France, where the disorder affects 1 in 26,000 individuals.
Causes
It is caused by abnormal transport of the amino acid cystine from lysosomes of all tissues, resulting in a massive intra-lysosomal cystine accumulation. Via an as yet unknown mechanism, lysosomal cystine appears to amplify apoptosis such that cells die inappropriately, leading to loss of renal epithelial cells, accounting for the renal Fanconi syndrome, and similar loss in other tissues can account for the short stature, retinopathy, and other features of the disease.
Differentiating Cystinosis from Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Natural History
Complications
Prognosis
Diagnosis
Diagnostic Criteria
History and Symptoms
There are three distinct types of cystinosis each with slightly different symptoms: nephropathic cystinosis, intermediate cystinosis, and non-nephropathic or ocular cystinosis. Infants affected by nephropathic cystinosis initially exhibit poor growth and particular kidney problems (sometimes called renal Fanconi syndrome). The kidney problems lead to the loss of important minerals, salts, fluids, and other nutrients. The loss of nutrients not only impairs growth, but may result in soft, bowed bones (hypophosphatemic rickets), especially in the legs. The nutrient imbalances in the body lead to increased urination, thirst, dehydration, and abnormally acidic blood (acidosis). By about age two years, cystine crystals may be present in the cornea. The buildup of these crystals in the eye causes an increased sensitivity to light (photophobia). Untreated children will experience complete kidney failure by about age 10 years. Other signs and symptoms that may occur in untreated patients include muscle deterioration, blindness, inability to swallow, diabetes, and thyroid and nervous system problems.
Physical Examination
The signs and symptoms of intermediate cystinosis are the same as nephropathic cystinosis, but they occur at a later age. Intermediate cystinosis typically begins to affect individuals from age 12 years to age 15 years. Malfunctioning kidneys and corneal crystals are the main initial features of this disorder. If intermediate cystinosis is left untreated, complete kidney failure will occur, but usually not until the late teens to mid twenties.
People with non-nephropathic or ocular cystinosis do not usually experience growth impairment or kidney malfunction. The only symptom is photophobia due to cystine crystals in the cornea.
It is currently being researched at UC San Diego, Tulane University School of Medicine, and at the National Institutes of Health in Bethesda, Maryland as well as at Robert Gordon University in Aberdeen and in Sunderland, UK.
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Surgery
Prevention
See also
External links
- BC Health Guide
- Cystinosis Foundation UK - a UK Charity Supporting Families & Research
References
Cystinosis at NLM Genetics Home Reference