Cabozantinib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Cabozantinib is a multikinase inhibitor that is FDA approved for the treatment of patients with progressive, metastatic medullary thyroid cancer (MTC).. Common adverse reactions include diarrhea, stomatitis, palmar-plantar erythrodysesthesia syndrome (PPES), decreased weight, decreased appetite, nausea, fatigue, oral pain, hair color changes, dysgeusia, hypertension, abdominal pain, and constipation.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Medullary thyroid cancer
- Cabozantinib is indicated for the treatment of patients with progressive, metastatic medullary thyroid cancer (MTC)
Recommended Dose
- The recommended daily dose of Cabozantinib is 140 mg (one 80-mg and three 20-mg capsules). Do not administer Cabozantinib with food. Instruct patients not to eat for at least 2 hours before and at least 1 hour after taking Cabozantinib. Continue treatment until disease progression or unacceptable toxicity occurs.
- Swallow Cabozantinib capsules whole. Do not open Cabozantinib capsules.
- Do not take a missed dose within 12 hours of the next dose.
- Do not ingest foods (e.g., grapefruit, grapefruit juice) or nutritional supplements that are known to inhibit cytochrome P450 during Cabozantinib treatment.
Dosage Adjustments
- For Adverse Reactions
- Withhold Cabozantinib for NCI CTCAE Grade 4 hematologic adverse reactions, Grade 3 or greater non-hematologic adverse reactions or intolerable Grade 2 adverse reactions.
- Upon resolution/improvement of the adverse reaction (i.e., return to baseline or resolution to Grade 1), reduce the dose as follows:
- If previously receiving 140 mg daily dose, resume treatment at 100 mg daily (one 80-mg and one 20-mg capsule)
- If previously receiving 100 mg daily dose, resume treatment at 60 mg daily (three 20-mg capsules)
- If previously receiving 60 mg daily dose, resume at 60 mg if tolerated, otherwise, discontinue Cabozantinib
- Permanently discontinue Cabozantinib for any of the following:
- Development of visceral perforation or fistula formation
- Severe hemorrhage
- Serious arterial thromboembolic event (e.g., myocardial infarction, cerebral infarction)
- Nephrotic syndrome
- Malignant hypertension, hypertensive crisis, persistent uncontrolled hypertension despite optimal medical management
- Osteonecrosis of the jaw
- Reversible posterior leukoencephalopathy syndrome
- In Patients with Hepatic Impairment
- Cabozantinib is not recommended for use in patients with moderate and severe hepatic impairment .
- In Patients Taking CYP3A4 Inhibitors
- Avoid the use of concomitant strong CYP3A4 inhibitors (e.g., ketoconazole, itraconazole, clarithromycin, atazanavir, nefazodone, saquinavir, telithromycin, ritonavir, indinavir, nelfinavir, voriconazole) in patients receiving Cabozantinib.
- For patients who require treatment with a strong CYP3A4 inhibitor, reduce the daily Cabozantinib dose by 40 mg (for example, from 140 mg to 100 mg daily or from 100 mg to 60 mg daily). Resume the dose that was used prior to initiating the CYP3A4 inhibitor 2 to 3 days after discontinuation of the strong inhibitor.
- In Patients Taking Strong CYP3A4 Inducers
- Avoid the chronic use of concomitant strong CYP3A4 inducers (e.g., phenytoin, carbamazepine, rifampin, rifabutin, rifapentine, phenobarbital) if alternative therapy is available .
- Do not ingest foods or nutritional supplements (e.g., St. John’s Wort (Hypericum perforatum)) that are known to induce cytochrome P450 activity.
- For patients who require treatment with a strong CYP3A4 inducer, increase the daily Cabozantinib dose by 40 mg (for example, from 140 mg to 180 mg daily or from 100 mg to 140 mg daily) as tolerated. Resume the dose that was used prior to initiating the CYP3A4 inducer 2 to 3 days after discontinuation of the strong inducer. The daily dose of Cabozantinib should not exceed 180 mg.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Cabozantinib in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and effectiveness of Cabozantinib in pediatric patients have not been studied.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
The safety and effectiveness of Cabozantinib in pediatric patients have not been studied.
Non–Guideline-Supported Use
The safety and effectiveness of Cabozantinib in pediatric patients have not been studied.
Contraindications
- None
Warnings
Perforations and Fistulas
- Gastrointestinal (GI) perforations and fistulas were reported in 3% and 1% of Cabozantinib-treated patients, respectively. All were serious and one GI fistula was fatal (< 1%). Non-GI fistulas including tracheal/esophageal were reported in 4% of Cabozantinib-treated patients. Two (1%) of these were fatal.
- Monitor patients for symptoms of perforations and fistulas. Discontinue Cabozantinib in patients who experience a perforation or a fistula.
Hemorrhage
- Serious and sometimes fatal hemorrhage occurred with Cabozantinib. The incidence of Grade ≥3 hemorrhagic events was higher in Cabozantinib-treated patients compared with placebo (3% vs. 1%).
- Do not administer Cabozantinib to patients with a recent history of hemorrhage or hemoptysis.
Thrombotic Events
- Cabozantinib treatment results in an increased incidence of thrombotic events (venous thromboembolism: 6% vs. 3% and arterial thromboembolism: 2% vs. 0% in Cabozantinib-treated and placebo-treated patients, respectively).
- Discontinue Cabozantinib in patients who develop an acute myocardial infarction or any other clinically significant arterial thromboembolic complication.
Wound Complications
- Wound complications have been reported with Cabozantinib. Stop treatment with Cabozantinib at least 28 days prior to scheduled surgery. Resume Cabozantinib therapy after surgery based on clinical judgment of adequate wound healing. Withhold Cabozantinib in patients with dehiscence or wound healing complications requiring medical intervention.
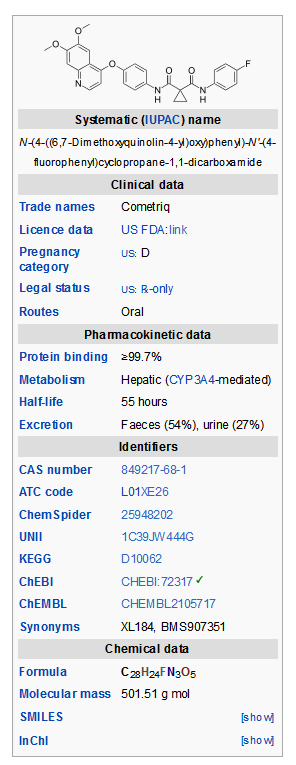
Hypertension
- Cabozantinib treatment results in an increased incidence of treatment-emergent hypertension with Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (modified JNC criteria) stage 1 or 2 hypertension identified in 61% in Cabozantinib-treated patients compared with 30% of placebo-treated patients in the randomized trial. Monitor blood pressure prior to initiation and regularly during Cabozantinib treatment. Withhold Cabozantinib for hypertension that is not adequately controlled with medical management; when controlled, resume Cabozantinib at a reduced dose. Discontinue Cabozantinib for severe hypertension that cannot be controlled with anti-hypertensive therapy.
Osteonecrosis of the Jaw
- Osteonecrosis of the jaw (ONJ) occurred in 1% of Cabozantinib-treated patients. ONJ can manifest as jaw pain, osteomyelitis, osteitis, bone erosion, tooth or periodontal infection, toothache, gingival ulceration or erosion, persistent jaw pain or slow healing of the mouth or jaw after dental surgery. Perform an oral examination prior to initiation of Cabozantinib and periodically during Cabozantinib therapy. Advise patients regarding good oral hygiene practices. For invasive dental procedures, withhold Cabozantinib treatment for at least 28 days prior to scheduled surgery, if possible.
Palmar-Plantar Erythrodysesthesia Syndrome
- Palmar-plantar erythrodysesthesia syndrome (PPES) occurred in 50% of patients treated with Cabozantinib and was severe (≥ Grade 3) in 13% of patients. Withhold Cabozantinib in patients who develop intolerable Grade 2 PPES or Grade 3-4 PPES until improvement to Grade 1; resume Cabozantinib at a reduced dose.
Proteinuria
- Proteinuria was observed in 4 (2%) of patients receiving Cabozantinib, including one with nephrotic syndrome, as compared to none of the patients receiving placebo. Monitor urine protein regularly during Cabozantinib treatment. Discontinue Cabozantinib in patients who develop nephrotic syndrome.
Reversible Posterior Leukoencephalopathy Syndrome
- Reversible Posterior Leukoencephalopathy Syndrome (RPLS), a syndrome of subcortical vasogenic edema diagnosed by characteristic finding on MRI, occurred in one (<1%) patient. Perform an evaluation for RPLS in any patient presenting with seizures, headache, visual disturbances, confusion or altered mental function. Discontinue Cabozantinib in patients who develop RPLS.
Drug Interactions
- Avoid administration of Cabozantinib with agents that are strong CYP3A4 inducers or inhibitors.
Hepatic Impairment
- Cabozantinib is not recommended for use in patients with moderate or severe hepatic impairment .
Embryo-fetal Toxicity
- Cabozantinib can cause fetal harm when administered to a pregnant woman. Cabozantinib was embryolethal in rats at exposures below the recommended human dose, with increased incidences of skeletal variations in rats and visceral variations and malformations in rabbits. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus
Adverse Reactions
Clinical Trials Experience
- The following serious adverse reactions are discussed elsewhere in the label:
Clinical Trial Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The safety of Cabozantinib was evaluated in 330 patients with progressive metastatic medullary thyroid cancer randomized to receive 140 mg Cabozantinib (n = 214) or placebo (n = 109) administered daily until disease progression or intolerable toxicity in a randomized, doubleblind, controlled trial.The data described below reflect a median exposure to Cabozantinib for 204 days. The population exposed to Cabozantinib was 70% male, 90% white, and had a median age of 55 years.
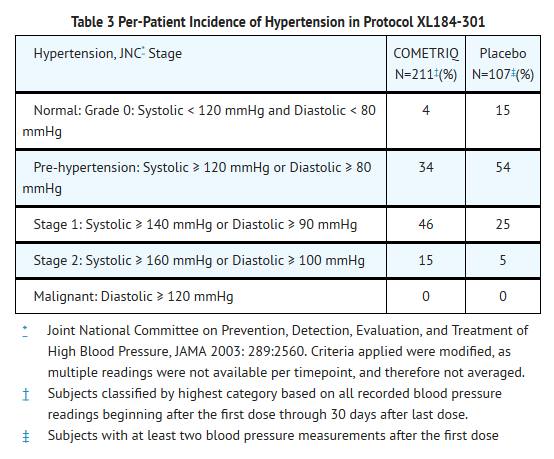
- Adverse reactions which occurred in ≥ 25% of Cabozantinib-treated patients occurring more frequently in the Cabozantinib arm with a between-arm difference of ≥ 5% included, in order of decreasing frequency: diarrhea, stomatitis, palmar-plantar erythrodysesthesia syndrome (PPES), decreased weight, decreased appetite, nausea, fatigue, oral pain, hair color changes, dysgeusia, hypertension, abdominal pain, and constipation. The most common laboratory abnormalities (>25%) were increased AST, increased ALT, lymphopenia, increased ALP, hypocalcemia, neutropenia, thrombocytopenia, hypophosphatemia, and hyperbilirubinemia. Grade 3-4 adverse reactions and laboratory abnormalities which occurred in ≥ 5% of Cabozantinib-treated patients occurring more frequently in the Cabozantinib arm with a between-arm difference of ≥ 2% included, in order of decreasing frequency; diarrhea, PPES, lymphopenia, hypocalcemia, fatigue, hypertension, asthenia, increased ALT, decreased weight, stomatitis, and decreased appetite.
- Fatal adverse reactions occurred in 6% of patients receiving Cabozantinib and resulted from hemorrhage, pneumonia, septicemia, fistulas, cardiac arrest, respiratory failure, and unspecified death. Fatal adverse reactions occurred in 5% of patients receiving placebo and resulted from septicemia, pneumonia, and general deterioration.
- The dose was reduced in 79% of patients receiving Cabozantinib compared to 9% of patients receiving placebo. The median number of dosing delays was one in patients receiving Cabozantinib compared to none in patients receiving placebo. Adverse reactions led to study treatment discontinuation in 16% of patients receiving Cabozantinib and in 8% of patients receiving placebo. The most frequent adverse reactions leading to permanent discontinuation in patients treated with Cabozantinib were: hypocalcemia, increased lipase, PPES, diarrhea, fatigue, hypertension, nausea, pancreatitis, tracheal fistula formation and vomiting.
- Increased levels of thyroid stimulating hormone (TSH) were observed in 57% of patients receiving Cabozantinib after the first dose compared to 19% of patients receiving placebo (regardless of baseline value). Ninety-two percent (92%) of patients on the Cabozantinib arm had a prior thyroidectomy, and 89% were taking thyroid hormone replacement prior to the first dose.
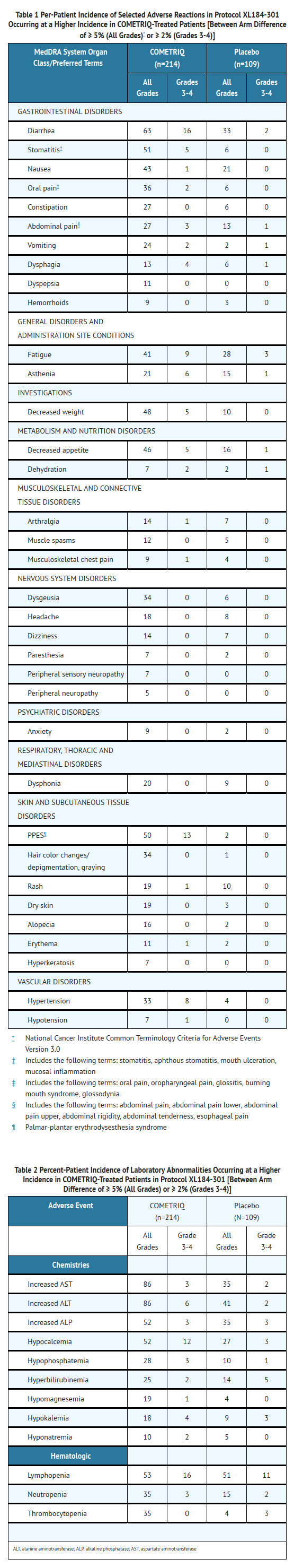
- Nearly all Cabozantinib-treated patients (96% vs. 84% placebo) experienced elevated blood pressure and there was a doubling in the incidence of overt hypertension in Cabozantinib-treated patients over placebo-treated patients (61% vs. 30%) according to modified Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC) staging criteria. No patients developed malignant hypertension.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Cabozantinib in the drug label.
Drug Interactions
Effect of CYP3A4 Inhibitors
- Administration of a strong CYP3A4 inhibitor, ketoconazole (400 mg daily for 27 days) to healthy subjects increased single-dose plasma cabozantinib exposure (AUC0-inf) by 38%. Avoid taking a strong CYP3A4 inhibitor (e.g., ketoconazole, itraconazole, clarithromycin, atazanavir, indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, voriconazole) when taking Cabozantinib.
Effect of CYP3A4 Inducers
- Administration of a strong CYP3A4 inducer, rifampin (600 mg daily for 31 days) to healthy subjects decreased single-dose plasma cabozantinib exposure (AUC0-inf) by 77%. Avoid chronic co-administration of strong CYP3A4 inducers (e.g., dexamethasone, phenytoin, carbamazepine, rifampin, rifabutin, rifapentine, phenobarbital, St.John’s Wort) with Cabozantinib
Use in Specific Populations
Pregnancy
Risk Summary
- Based on its mechanism of action, Cabozantinib can cause fetal harm when administered to a pregnant woman. Cabozantinib was embryolethal in rats at exposures below the recommended human dose, with increased incidences of skeletal variations in rats and visceral variations and malformations in rabbits. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
Animal Data
- In an embryo-fetal development study in which pregnant rats were administered daily doses of cabozantinib during organogenesis, increased loss of pregnancy compared to controls was observed at doses as low as 0.03 mg/kg (less than 1% of the human exposure by AUC at the recommended dose). Findings included delayed ossifications and skeletal variations at doses equal to or greater than 0.01 mg/kg/day (approximately 0.03% of the human exposure by AUC at the recommended dose).
- In pregnant rabbits administered cabozantinib daily during organogenesis there were findings of visceral malformations and variations including reduced spleen size and missing lung lobe at 3 mg/kg (approximately 11% of the human exposure by AUC at the recommended dose).
- There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Cabozantinib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Cabozantinib during labor and delivery.
Nursing Mothers
- It is unknown whether cabozantinib or its metabolites are excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Cabozantinib, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and effectiveness of Cabozantinib in pediatric patients have not been studied.
Geriatic Use
- Clinical studies of Cabozantinib did not include sufficient numbers of patients aged 65 years and over to determine whether they respond differently from younger patients
Gender
Females and Males of Reproductive Potential
- Contraception
- Use effective contraception during treatment with Cabozantinib and up to 4 months after completion of therapy.
- There are no data on the effect of Cabozantinib on human fertility. Cabozantinib impaired male and female fertility in animal studies
Race
There is no FDA guidance on the use of Cabozantinib with respect to specific racial populations.
Renal Impairment
- No dose adjustment is recommended for patients with mild or moderate renal impairment. There is no experience with Cabozantinib in patients with severe renal impairment.
Hepatic Impairment
- Cabozantinib pharmacokinetics has not been studied in patients with hepatic impairment. There are limited data in patients with liver impairment (serum bilirubin greater than 1.5 times the upper limit of normal). Cabozantinib is not recommended for use in patients with moderate or severe hepatic impairment, as safety and efficacy have not been established
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Cabozantinib in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Cabozantinib in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Cabozantinib in the drug label.
- Description
IV Compatibility
There is limited information regarding IV Compatibility of Cabozantinib in the drug label.
Overdosage
- One case of overdosage was reported in a patient who inadvertently took twice the intended dose (200 mg daily) for nine days. The patient suffered Grade 3 memory impairment, Grade 3 mental status changes, Grade 3 cognitive disturbance, Grade 2 weight loss, and Grade 1 increase in BUN. The extent of recovery was not documented
Pharmacology
Mechanism of Action
- In vitro biochemical and/or cellular assays have shown that cabozantinib inhibits the tyrosine kinase activity of RET, MET, VEGFR-1, -2 and -3, KIT, TRKB, FLT-3, AXL, and TIE-2. These receptor tyrosine kinases are involved in both normal cellular function and pathologic processes such as oncogenesis, metastasis, tumor angiogenesis, and maintenance of the tumor microenvironment.
Structure
- Cabozantinib is the (S)-malate salt of cabozantinib. Cabozantinib (S)-malate is described chemically as N-(4-(6,7-dimethoxyquinolin-4-yloxy)phenyl)-N'-(4-fluorophenyl)cyclopropane- 1,1-dicarboxamide, (2S)-hydroxybutanedioate. The molecular formula is C28H24FN3O5.C4H6O5 and the molecular weight is 635.6 Daltons as malate salt. The chemical structure of cabozantinib (S)-malate salt is:
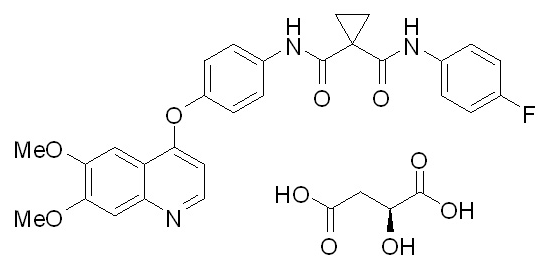
- Cabozantinib (S)-malate salt is a white to off-white solid that is practically insoluble in aqueous media.
- Cabozantinib (cabozantinib) capsules are supplied as printed hard gelatin capsules containing cabozantinib (S)-malate equivalent to 20 mg or 80 mg cabozantinib and the following inactive ingredients: silicified microcrystalline cellulose, croscarmellose sodium, sodium starch glycolate, fumed silica, and stearic acid.
- The grey gelatin capsule shells contain black iron oxide and titanium dioxide and the Swedish orange gelatin capsule shells contain red iron oxide, and titanium dioxide. The printing ink contains shellac glaze, black iron oxide, N-butyl alcohol, isopropyl alcohol, propylene glycol, and ammonium hydroxide.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Cabozantinib in the drug label.
Pharmacokinetics
- A population pharmacokinetic analysis of cabozantinib was performed using data collected from 289 patients with solid tumors including MTC following oral administration of 140 mg daily doses. The predicted effective half-life is approximately 55 hours, the oral volume of distribution (V/F) is approximately 349 L, and the clearance (CL/F) at steady-state is estimated to be 4.4 L/hr.
Absorption and Distribution
- Following oral administration of Cabozantinib, median time to peak cabozantinib plasma concentrations (Tmax) ranged from 2 to 5 hours post-dose. Repeat daily dosing of Cabozantinib at 140 mg for 19 days resulted in 4- to 5-fold mean cabozantinib accumulation (based on AUC) compared to a single dose administration; steady state was achieved by Day 15. Cabozantinib is highly protein bound in human plasma (≥ 99.7%).
- A high-fat meal increased Cmax and AUC values by 41% and 57%, respectively relative to fasted conditions in healthy subjects administered a single 140 mg oral Cabozantinib dose.
Metabolism and Elimination
- Cabozantinib is a substrate of CYP3A4 in vitro. Inhibition of CYP3A4 reduced the formation of the XL184 N-oxide metabolite by >80%. Inhibition of CYP2C9 had a minimal effect on cabozantinib metabolite formation (i.e., a <20% reduction). Inhibition of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C19, CYP2D6 and CYP2E1 had no effect on cabozantinib metabolite formation.
- Within a 48-day collection period after a single dose of 14C-cabozantinib in healthy subjects, approximately 81% of the total administered radioactivity was recovered with 54% in feces and 27% in urine.
Specific Populations
- Renal Impairment: No formal pharmacokinetic study of cabozantinib has been conducted in patients with renal impairment. The results of a population pharmacokinetic analysis suggested that mild to moderate renal impairment (creatinine clearance value ≥30 mL/min) does not have a clinically relevant effect on the clearance of cabozantinib.
- Hepatic Impairment: The pharmacokinetics of cabozantinib has not been studied in patients with hepatic impairment .
- Pediatric Population: The pharmacokinetics of cabozantinib has not been studied in the pediatric population .
- Effects of Age, Gender and Race: A population PK analysis did not identify clinically relevant differences in clearance of cabozantinib between females and males or between Whites (89%) and non-Whites (11%). Cabozantinib pharmacokinetics was not affected by age (20-86 years).
Drug Interactions
- CYP Enzyme Inhibition and Induction: Cabozantinib is a noncompetitive inhibitor of CYP2C8 (Kiapp = 4.6 μM), a mixed-type inhibitor of both CYP2C9 (Kiapp = 10.4 μM) and CYP2C19 (Kiapp = 28.8 μM), and a weak competitive inhibitor of CYP3A4 (estimated Kiapp = 282 μM) in human liver microsomal (HLM) preparations. IC50 values >20 μM were observed for CYP1A2, CYP2D6, and CYP3A4 isozymes in both recombinant and HLM assay systems.
- Cabozantinib is an inducer of CYP1A1 mRNA in human hepatocyte incubations (i.e., 75-100% of CYP1A1 positive control β-naphthoflavone induction), but not of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19 or CYP3A4 mRNA or isozyme-associated enzyme activities.
- Cabozantinib at steady-state plasma concentrations (≥100 mg/day daily for a minimum of 21 days) showed no effect on single-dose rosiglitazone (a CYP2C8 substrate) plasma exposure (Cmax and AUC) in patients with solid tumors.
- P-glycoprotein Inhibition: Cabozantinib is an inhibitor (IC50 = 7.0 μM), but not a substrate, of P-gp transport activities in a bi-directional assay system using MDCK-MDR1 cells. Therefore, cabozantinib may have the potential to increase plasma concentrations of co-administered substrates of P-gp.
Cardiac Electrophysiology
- The effect of orally administered Cabozantinib 140 mg on QTc interval was evaluated in a randomized, double-blinded, placebo-controlled study in patients with MTC. A mean increase in QTcF of 10 - 15 ms was observed at 4 weeks after initiating Cabozantinib. A concentration-QTc relationship could not be definitively established. Changes in cardiac wave form morphology or new rhythms were not observed. No Cabozantinib-treated patients had a QTcF > 500 ms.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Studies examining the carcinogenic potential of cabozantinib have not been conducted.
- Cabozantinib was not mutagenic in vitro in the bacterial reverse mutation (Ames) assay and was not clastogenic in both the in vitro cytogenetic assay using human lymphocytes or in the in vivo mouse micronucleus assay.
- Based on nonclinical findings, male and female fertility may be impaired by treatment with Cabozantinib. In a fertility study in which cabozantinib was administered to male and female rats at doses of 1, 2.5, and 5 mg/kg/day, male fertility was significantly compromised at doses equal to or greater than 2.5 mg/kg/day (approximately equal to the human exposure by AUC at the recommended dose), with a decrease in sperm counts and reproductive organ weights. In females, fertility was significantly reduced at doses equal to or greater than 1 mg/kg/day (approximately 50% of the human exposure by AUC at the recommended dose) with a significant decrease in the number of live embryos and a significant increase in pre- and postimplantation losses.
- Observations of effects on reproductive tract tissues in general toxicology studies were supportive of effects noted in the dedicated fertility study and included hypospermia and absence of corpora luteain male and female dogs in a 6-month repeat dose study at exposures equal to 6% and 3%, respectively, the human exposure by AUC at the recommended dose. In addition, female rats administered 5 mg/kg/day for 14 days (approximately equal to the human exposure by AUC at the recommended dose) exhibited ovarian necrosis.
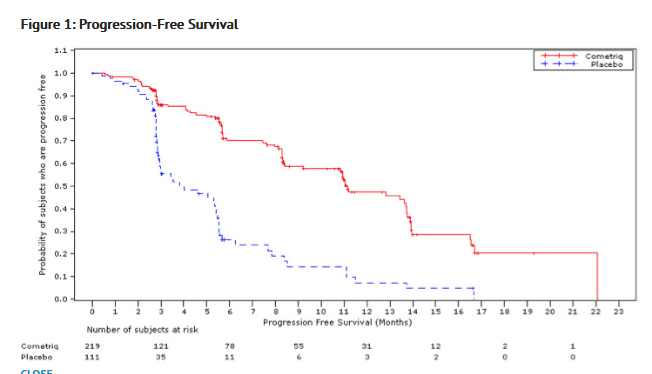
Clinical Studies
- The safety and efficacy of Cabozantinib was assessed in an international, multi-center, randomized, double-blind, controlled trial (Study 1) of 330 patients with metastatic medullary thyroid carcinoma (MTC). Patients were required to have evidence of actively progressive disease within 14 months prior to study entry confirmed by an Independent Radiology Review Committee (IRRC) masked to treatment assignment (89%) or the treating physician (11%). Patients were randomized (2:1) to receive Cabozantinib 140 mg (n = 219) or placebo (n = 111) orally once daily, without food, until disease progression determined by the treating physician or until intolerable toxicity. Randomization was stratified by age (≤ 65 years vs. > 65 years) and prior use of a tyrosine kinase inhibitor (TKI) (yes vs. no). No cross-over was allowed at the time of progression. The main efficacy outcome measures of progression-free survival (PFS), objective response (OR), and response duration were based on IRRC-confirmed events using modified RECIST criteria.
- Of 330 patients randomized, 67% were male, the median age was 55 years, 23% were 65 years or older, 89% were white, 54% had a baseline ECOG performance status of 0, 92% had undergone a thyroidectomy, and 48% were reported to be RET mutation positive according to research-use assays. Twenty-five percent (25%) had two or more prior systemic therapies and 21% had been previously treated with a TKI.
- A statistically significant prolongation in PFS was demonstrated among Cabozantinib-treated patients compared to those receiving placebo [HR 0.28 (95% CI: 0.19, 0.40); p <0.0001], with median PFS times of 11.2 months and 4.0 months in the Cabozantinib and placebo arms, respectively.
- Partial responses were observed only among patients in the Cabozantinib arm (27% vs. 0; p<0.0001). The median duration of objective responses was 14.7 months (95% CI: 11.1, 19.3) for patients treated with Cabozantinib. There was no statistically significant difference in overall survival between the treatment arms at the planned interim analysis.
How Supplied
- Cabozantinib 20 mg capsules are supplied as hard gelatin capsules with grey cap and grey body, printed with "XL184 20mg" in black ink and containing cabozantinib (S)-malate salt equivalent to 20 mg cabozantinib.
- Cabozantinib 80 mg capsules are supplied as hard gelatin capsules with Swedish orange cap and Swedish orange body, printed with "XL184 80mg" in black ink and containing cabozantinib (S)- malate salt equivalent to 80 mg cabozantinib.
- Cabozantinib capsules are supplied as follows:
Cartons
- 140 mg daily-dose carton NDC#42388-011-14
Containing four 140 mg daily-dose blister cards (each blister card contains seven 80-mg and twenty-one 20-mg capsules)
- 100 mg daily-dose carton NDC#42388-012-14
Containing four 100 mg daily-dose blister cards (each blister card contains seven 80-mg and seven 20-mg capsules)
- 60 mg daily-dose carton NDC#42388-013-14
Containing four 60 mg daily-dose blister cards (each blister card contains twenty-one 20-mg capsules)
- Bottle containing sixty 20-mg Cabozantinib capsules NDC#42388-014-25
Storage
- Store Cabozantinib at 20°C to 25°C (68°F to 77°F); excursions are permitted from 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Images
Drug Images
{{#ask: Page Name::Cabozantinib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Cabozantinib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Inform patients of the following:
- Cabozantinib often causes diarrhea which may be severe in some cases. Inform patients of the need to contact their healthcare provider if severe diarrhea occurs during treatment with Cabozantinib.
- Cabozantinib often causes palmar plantar erythrodysesthesia syndrome. Advise patients to contact their healthcare provider for progressive or intolerable rash.
- Cabozantinib often causes sores in the mouth, oral pain, changes in taste, nausea or vomiting. Advise patients to contact their healthcare provider if any of these symptoms are severe or prevent patients from eating and drinking.
- Cabozantinib often causes weight loss which may be significant in some cases. Advise patients to report significant weight loss.
- To contact their healthcare provider before any planned surgeries, including dental procedures.
- Cabozantinib may interact with other drugs; advise patients to inform their healthcare provider of all prescription or nonprescription medication or herbal products that they are taking.
- Patients of childbearing potential must use effective contraception during therapy and for at least four months following their last dose of Cabozantinib.
- Breast-feeding mothers must discontinue nursing while receiving Cabozantinib therapy.
- Cabozantinib should not be taken with food. Instruct patients not to eat for at least 2 hours before and at least 1 hour after taking Cabozantinib. Cabozantinib capsules should not be opened or crushed but should be taken with a full glass (at least 8 ounces) of water.
- Patients should not consume grapefruits or grapefruit juice while taking Cabozantinib treatment.
Precautions with Alcohol
- Alcohol-Cabozantinib interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Cometriq®
Look-Alike Drug Names
- A® — B®
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Cabozantinib
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Cabozantinib |Label Name=Cabozantinib08.png
}}
{{#subobject:
|Label Page=Cabozantinib |Label Name=Cabozantinib09.png
}}