Ambien CR
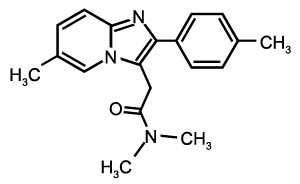
| N,N,6-trimethyl-2-(4-methylphenyl)- imidazo(1,2-a)pyridine-3-acetamide | |
| CAS number not known |
ATC code not known |
| Chemical formula | C19H21N3O |
| Molecular weight | 764.88 |
| Bioavailability | 92% bound in plasma |
| Metabolism | Hepatic |
| Elimination half-life | 2.8 hours (normal liver function) |
| Excretion | Renal |
| Pregnancy category | Category B |
| Legal status | Schedule IV |
| Routes of administration | Oral |
| Formulation(s) | Ambien CR: 6.25mg tablet, 12.5mg tablet |
Ambien CR (zolpidem tartrate extended release) is different from Ambien (zolpidem tartrate) in that the medication is formulated in a 2 layer tablet. The first layer of the Ambien CR tablet dissolves quickly to help people fall asleep, while the 2nd layer dissolves slowly over the night to help people stay asleep (something Ambien has not demonstrated in trials). The action of both immediate and continuous release with Ambien CR allows for increased effectiveness over the night (since blood levels are more stable 3 to 6 hours after taking medication) and is proven to be more effective than traditional Ambien in quality of sleep. Ambien CR and Ambien have the same active ingredient so the safety and tolerability profiles are similar. Even though Ambien CR helps maintain sleep throughout the middle of the night it does not increase the risk of "hangover" effects (same as regular Ambien). A recent long term study found effectiveness over 6-months, improved morning concentration and daytime function, and no risk of abuse with Ambien CR (Krystal 2007).
Uses
Ambien CR is FDA-approved for both short and long-term treatment of insomnia.
Pharmacodynamics
Subunit modulation of the GABA receptor chloride channel macromolecular complex is hypothesized to be responsible for sedative, anticonvulsant, anxiolytic, and myorelaxant drug properties. The major modulatory site of the GABA receptor complex is located on its alpha-(a) subunit and is referred to as the benzodiazepine (BZ) receptor.
Zolpidem, the active moiety of zolpidem tartrate, is a hypnotic agent with a chemical structure unrelated to benzodiazepines, barbiturates, pyrrolopyrazines, pyrazolopyrimidines, or other drugs with known hypnotic properties. In contrast to the benzodiazepines, which nonselectively bind to and activate all BZ receptor subtypes, zolpidem in vitro binds the BZ1 receptor preferentially with a high affinity ratio of the alpha1/alpha5 subunits. The BZ1 receptor is found primarily on the Lamina IV of the sensorimotor cortical regions, substantia nigra (pars reticulata), cerebellum's molecular layer, olfactory bulb, ventral thalamic complex, pons, inferior colliculus, and globus pallidus. This selective binding of zolpidem on the BZ1 receptor is not absolute, but it may explain the relative absence of myorelaxant and anticonvulsant effects in animal studies as well as the preservation of deep sleep (stages 3 and 4) in human studies of zolpidem at hypnotic doses.
Pharmacokinetics
Ambien CR exhibits biphasic absorption characteristics, which results in rapid initial absorption from the gastrointestinal tract similar to zolpidem tartrate immediate-release, then provides extended plasma concentrations beyond three hours after administration. A study in 24 healthy male subjects was conducted to compare mean zolpidem plasma concentration-time profiles obtained after single oral administration of Ambien CR (12.5 mg) and of an immediate-release formulation of zolpidem tartrate (10 mg). The terminal elimination half-life observed with Ambien CR (12.5 mg) was similar to that obtained with immediate-release zolpidem tartrate (10 mg). The mean plasma concentration time profiles for Ambien CR (12.5 mg) and for zolpidem tartrate (10 mg) are shown below:
Absorption
Following administration of Ambien CR, administered as a single 12.5-mg dose in healthy male adult subjects, the mean peak concentration (cmax) of zolpidem was 134 ng/mL (range: 68.9 to 197 ng/ml) occurring at a median time (tmax) of 1.5 hours. The mean AUC of zolpidem was 740 ng·hr/mL (range: 295 to 1359 ng·hr/mL).
A food-effect study in 45 healthy volunteers compared the pharmacokinetics of Ambien CR 12.5 mg when administered while fasting or within 30 minutes after a meal. Results demonstrated that with food, mean AUC and cmax were decreased by 23% and 30%, respectively, while median tmax was increased from 2 hours to 4 hours. The half-life was not changed. These results suggest that, for faster sleep onset, Ambien CR should not be administered with or immediately after a meal.
Total protein binding was found to be 92.5 ± 0.1% and remained constant, independent of concentration between 40 and 790 ng/mL.
Ambien CR administered as a single 12.5 mg dose in healthy male adult subjects, the mean zolpidem elimination half-life was 2.8 hours (range: 1.62 to 4.05 hr).
Controlled Trials
Ambien CR was evaluated in two placebo-controlled studies for the treatment of patients with chronic primary insomnia (as defined in the APA Diagnostic and Statistical Manual of Mental Disorders, DSM IV).
Adult outpatients (18-64 years) with primary insomnia (N=212) were evaluated in a double-blind, randomized, parallel-group, 3-week trial comparing Ambien CR 12.5 mg and placebo. Ambien CR 12.5 mg decreased wake time after sleep onset (WASO) for the first 7 hours during the first 2 nights and for the first 5 hours after 2 weeks of treatment. Ambien CR 12.5 mg was superior to placebo on objective measures (polysomnography recordings) of sleep induction (by decreasing latency to persistent sleep [LPS]) during the first 2 nights of treatment and after 2 weeks of treatment. Ambien CR 12.5 mg was also superior to placebo on the patient reported global impression regarding the aid to sleep after the first 2 nights and after 3 weeks of treatment.
Elderly outpatients (³ 65 years) with primary insomnia (N=205) were evaluated in a double-blind, randomized, parallel-group, 3-week trial comparing Ambien CR 6.25 mg and placebo. Ambien CR 6.25 mg decreased wake time after sleep onset (WASO) for the first 6 hours during the first 2 nights and the first 4 hours after 2 weeks of treatment. Ambien CR 6.25 mg was superior to placebo on objective measures (polysomnography recordings) of sleep induction (by decreasing latency to persistent sleep [LPS]) during the first 2 nights of treatment and after 2 weeks on treatment. Ambien CR 6.25 mg was superior to placebo on the patient reported global impression regarding the aid to sleep after the first 2 nights and after 3 weeks of treatment.
In both studies, in patients treated with Ambien CR, polysomnography showed increased wakefulness at the end of the night compared to placebo-treated patients.
Side-Effects
Next-day residual effects: In five clinical studies; three controlled studies in adults (18-64 years of age) administered Ambien CR 12.5 mg and two controlled studies in the elderly (³ 65 years of age) administered Ambien CR 6.25 mg or 12.5 mg, the effect of Ambien CR on vigilance, memory, or motor function were assessed using neurocognitive tests. In these studies, no significant decrease in performance was observed eight hours after a nighttime dose. In addition, no evidence of next-day residual effects were detected with Ambien CR 12.5 mg and 6.25 mg using self-ratings of sedation.
Next day somnolence was reported by 15% of the adult patients who received 12.5 mg Ambien CR versus 2% of the placebo group. Next day somnolence was reported by 6% of the elderly patients who received 6.25 mg Ambien CR versus 5% of the placebo group. (See Adverse Reactions.)
Rebound effects: Rebound insomnia, defined as a dose-dependent worsening in sleep parameters (latency, sleep efficiency, and number of awakenings) compared with baseline following discontinuation of treatment, is observed with short- and intermediate-acting hypnotics. In the two placebo-controlled studies in patients with primary insomnia, a rebound effect was only observed on the first night after abrupt discontinuation of Ambien CR. On the second night, there was no worsening compared to baseline in the Ambien CR group.
References
is this safe for people with liver desease?