Vertebral artery dissection: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| (8 intermediate revisions by 3 users not shown) | |||
| Line 16: | Line 16: | ||
==Overview== | ==Overview== | ||
'''Vertebral artery dissection''' is the development of [[Dissection (medical)|dissection]] (a flap-like tear) in the [[vertebral artery]]. It is commonly associated with [[physical trauma]] but may also develop spontaneously. It is a major cause of [[stroke]] in young people. | '''Vertebral artery dissection''' is the development of [[Dissection (medical)|dissection]] (a flap-like tear) in the [[vertebral artery]]. It is commonly associated with [[physical trauma]] but may also develop spontaneously. It is a major cause of [[ischemic stroke]] in young people. | ||
== | ==Epdidemiology and Demographics== | ||
The annual incidence is about 1 per 100,000 in America and 1.5 per 100,000 in France.<ref name=Santos-Franco/> | The annual incidence is about 1 per 100,000 in America and 1.5 per 100,000 in France.<ref name=Santos-Franco/> | ||
==Diagnosis== | ==Diagnosis== | ||
=== | ===Symptoms=== | ||
Typical features are [[pain and nociception|pain]] in the [[neck]] associated with stroke-like symptoms of the "posterior circulation": [[cranial nerve]] palsies, [[ataxia]], and cortical visual loss.<ref>{{cite journal |author=Thanvi B, Munshi SK, Dawson SL, Robinson TG |title=Carotid and vertebral artery dissection syndromes |journal=Postgrad Med J |volume=81 |issue=956 |pages=383–8 |year=2005 |pmid=15937204 |doi=10.1136/pgmj.2003.016774|url= http://pmj.bmj.com/cgi/content/full/81/956/383}}</ref> It can also cause [[subarachnoid hemorrhage]] (bleeding into the area around the brain); dissecting aneurysms of the vertebral artery represent about 4% of all [[aneurysm]]s.<ref name=Santos-Franco>{{cite journal |journal= Neurosurg Rev |date=2008 |title= Dissecting aneurysms of the vertebrobasilar system. A comprehensive review on natural history and treatment options |author= Santos-Franco JA, Zenteno M, Lee A |doi=10.1007/s10143-008-0124-x |pmid=18309525}}</ref> | |||
| | |||
| | |||
| | |||
| | |||
| | |||
===CT=== | ===CT=== | ||
<div align="left"> | <div align="left"> | ||
| Line 60: | Line 32: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
<div align="left"> | <div align="left"> | ||
| Line 68: | Line 39: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
<div align="left"> | <div align="left"> | ||
| Line 78: | Line 48: | ||
</div> | </div> | ||
== | ==2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS: Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease (DO NOT EDIT)<ref name="pmid21282505">{{cite journal| author=Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL et al.| title=2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. | journal=Circulation | year= 2011 | volume= 124 | issue= 4 | pages= 489-532 | pmid=21282505 | doi=10.1161/CIR.0b013e31820d8d78 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21282505 }} </ref>== | ||
===Management of Patients with Cervical Artery Dissection (DO NOT EDIT)<ref name="pmid21282505">{{cite journal| author=Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL et al.| title=2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. | journal=Circulation | year= 2011 | volume= 124 | issue= 4 | pages= 489-532 | pmid=21282505 | doi=10.1161/CIR.0b013e31820d8d78 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21282505 }} </ref>=== | |||
{|class="wikitable" | {|class="wikitable" | ||
|- | |- | ||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | | colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | ||
|- | |- | ||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' | | bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' Contrast-enhanced [[CTA]], [[MRA]], and catheter-based contrast angiography are useful for diagnosis of cervical artery dissection. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])'' <nowiki>"</nowiki> | ||
|} | |||
{|class="wikitable" | |||
|- | |- | ||
| | | colspan="1" style="text-align:center; background:LemonChiffon"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | ||
|- | |- | ||
| bgcolor=" | | bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' Antithrombotic treatment with either an anticoagulant ([[heparin]], [[low-molecular-weight heparin]], or [[warfarin]]) or a platelet inhibitor ([[aspirin]], [[clopidogrel]], or the combination of extended-release [[dipyridamole]] plus aspirin) for at least 3 to 6 months is reasonable for patients with extracranial carotid or [[vertebral arterial dissection]] associated with [[ischemic stroke]] or [[TIA]]<ref name="pmid17495218">{{cite journal |author=Metso TM, Metso AJ, Helenius J, ''et al.'' |title=Prognosis and safety of anticoagulation in intracranial artery dissections in adults |journal=Stroke |volume=38 |issue=6 |pages=1837–42 |year=2007 |month=June |pmid=17495218 |doi=10.1161/STROKEAHA.106.479501 |url=}}</ref><ref name="pmid17656656">{{cite journal |author=Engelter ST, Brandt T, Debette S, ''et al.'' |title=Antiplatelets versus anticoagulation in cervical artery dissection |journal=Stroke |volume=38 |issue=9 |pages=2605–11 |year=2007 |month=September |pmid=17656656 |doi=10.1161/STROKEAHA.107.489666 |url=}}</ref><ref name="pmid18303104">{{cite journal |author=Menon R, Kerry S, Norris JW, Markus HS |title=Treatment of cervical artery dissection: a systematic review and meta-analysis |journal=J. Neurol. Neurosurg. Psychiatr. |volume=79 |issue=10 |pages=1122–7 |year=2008 |month=October |pmid=18303104 |doi=10.1136/jnnp.2007.138800 |url=}}</ref><ref name="pmid19321846">{{cite journal |author=Georgiadis D, Arnold M, von Buedingen HC, ''et al.'' |title=Aspirin vs anticoagulation in carotid artery dissection: a study of 298 patients |journal=Neurology |volume=72 |issue=21 |pages=1810–5 |year=2009 |month=May |pmid=19321846 |doi=10.1212/WNL.0b013e3181a2a50a |url=}}</ref>. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: B]])'' <nowiki>"</nowiki> | ||
|} | |} | ||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIb]] | |||
|- | |||
| bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' Carotid angioplasty and stenting might be considered when ischemic neurological symptoms have not responded to antithrombotic therapy after acute carotid dissection. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])'' <nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''2.''' The safety and effectiveness of pharmacological therapy with a [[beta-adrenergic antagonist]], [[angiotensin inhibitor]], or nondihydropyridine calcium channel antagonist ([[verapamil]] or [[diltiazem]]) to lower blood pressure to the normal range and reduce arterial wall stress are not well established. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])'' <nowiki>"</nowiki> | |||
|} | |||
==Related Chapters== | |||
*[[Vertebral artery disease]] | |||
*[[Ischemic stroke]] | |||
==References== | ==References== | ||
| Line 102: | Line 90: | ||
[[Category:Neurological disorders]] | [[Category:Neurological disorders]] | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
{{WH}} | |||
Latest revision as of 16:30, 5 November 2012
| Vertebral artery dissection | |
 | |
|---|---|
| Arteries of the neck | |
| ICD-9 | 443.24 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Vertebral artery dissection is the development of dissection (a flap-like tear) in the vertebral artery. It is commonly associated with physical trauma but may also develop spontaneously. It is a major cause of ischemic stroke in young people.
Epdidemiology and Demographics
The annual incidence is about 1 per 100,000 in America and 1.5 per 100,000 in France.[1]
Diagnosis
Symptoms
Typical features are pain in the neck associated with stroke-like symptoms of the "posterior circulation": cranial nerve palsies, ataxia, and cortical visual loss.[2] It can also cause subarachnoid hemorrhage (bleeding into the area around the brain); dissecting aneurysms of the vertebral artery represent about 4% of all aneurysms.[1]
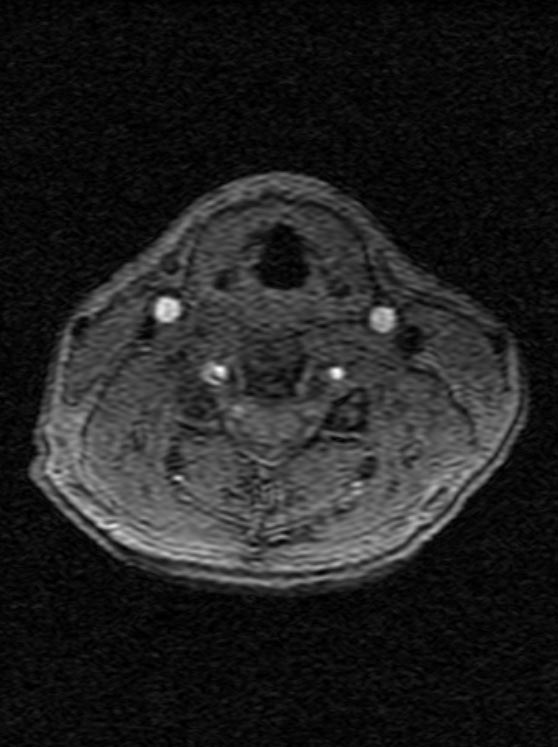
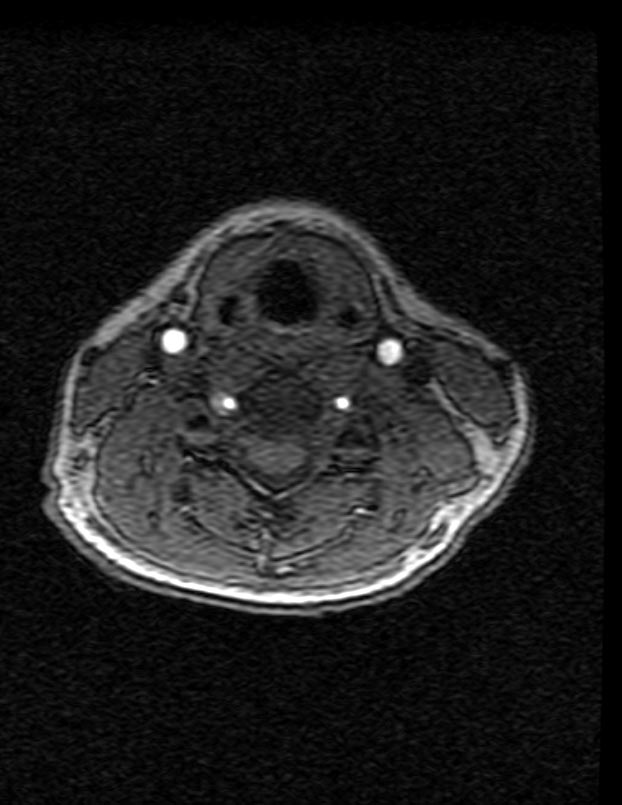
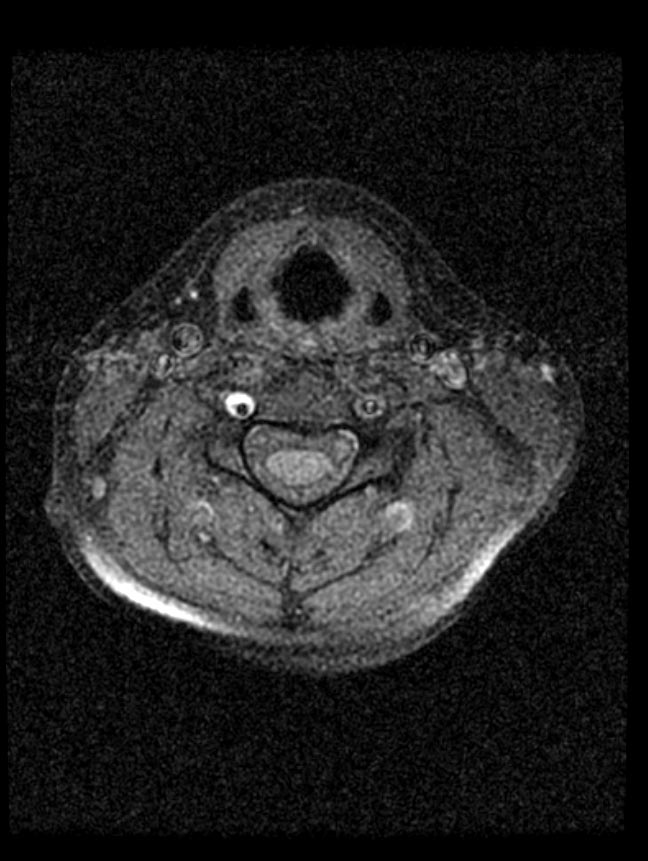
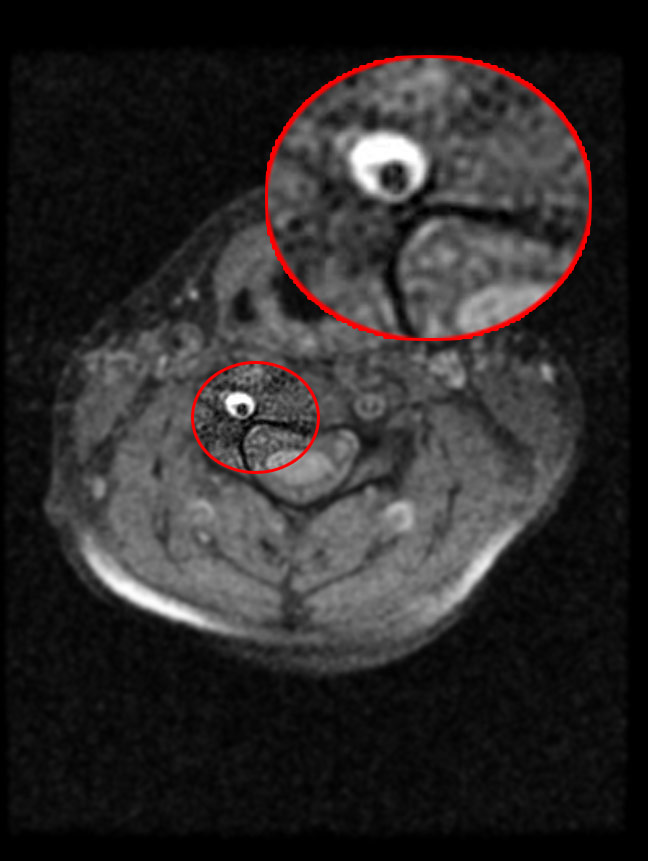
CT
2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS: Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease (DO NOT EDIT)[3]
Management of Patients with Cervical Artery Dissection (DO NOT EDIT)[3]
| Class I |
| "1. Contrast-enhanced CTA, MRA, and catheter-based contrast angiography are useful for diagnosis of cervical artery dissection. (Level of Evidence: C) " |
| Class IIa |
| "1. Antithrombotic treatment with either an anticoagulant (heparin, low-molecular-weight heparin, or warfarin) or a platelet inhibitor (aspirin, clopidogrel, or the combination of extended-release dipyridamole plus aspirin) for at least 3 to 6 months is reasonable for patients with extracranial carotid or vertebral arterial dissection associated with ischemic stroke or TIA[4][5][6][7]. (Level of Evidence: B) " |
| Class IIb |
| "1. Carotid angioplasty and stenting might be considered when ischemic neurological symptoms have not responded to antithrombotic therapy after acute carotid dissection. (Level of Evidence: C) " |
| "2. The safety and effectiveness of pharmacological therapy with a beta-adrenergic antagonist, angiotensin inhibitor, or nondihydropyridine calcium channel antagonist (verapamil or diltiazem) to lower blood pressure to the normal range and reduce arterial wall stress are not well established. (Level of Evidence: C) " |
Related Chapters
References
- ↑ 1.0 1.1 Santos-Franco JA, Zenteno M, Lee A (2008). "Dissecting aneurysms of the vertebrobasilar system. A comprehensive review on natural history and treatment options". Neurosurg Rev. doi:10.1007/s10143-008-0124-x. PMID 18309525.
- ↑ Thanvi B, Munshi SK, Dawson SL, Robinson TG (2005). "Carotid and vertebral artery dissection syndromes". Postgrad Med J. 81 (956): 383–8. doi:10.1136/pgmj.2003.016774. PMID 15937204.
- ↑ 3.0 3.1 Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL; et al. (2011). "2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery". Circulation. 124 (4): 489–532. doi:10.1161/CIR.0b013e31820d8d78. PMID 21282505.
- ↑ Metso TM, Metso AJ, Helenius J; et al. (2007). "Prognosis and safety of anticoagulation in intracranial artery dissections in adults". Stroke. 38 (6): 1837–42. doi:10.1161/STROKEAHA.106.479501. PMID 17495218. Unknown parameter
|month=ignored (help) - ↑ Engelter ST, Brandt T, Debette S; et al. (2007). "Antiplatelets versus anticoagulation in cervical artery dissection". Stroke. 38 (9): 2605–11. doi:10.1161/STROKEAHA.107.489666. PMID 17656656. Unknown parameter
|month=ignored (help) - ↑ Menon R, Kerry S, Norris JW, Markus HS (2008). "Treatment of cervical artery dissection: a systematic review and meta-analysis". J. Neurol. Neurosurg. Psychiatr. 79 (10): 1122–7. doi:10.1136/jnnp.2007.138800. PMID 18303104. Unknown parameter
|month=ignored (help) - ↑ Georgiadis D, Arnold M, von Buedingen HC; et al. (2009). "Aspirin vs anticoagulation in carotid artery dissection: a study of 298 patients". Neurology. 72 (21): 1810–5. doi:10.1212/WNL.0b013e3181a2a50a. PMID 19321846. Unknown parameter
|month=ignored (help)