Torsades de pointes differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 38: | Line 38: | ||
*[[Long QT syndrome]] | *[[Long QT syndrome]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Ventricular tachycardia originates from a ventricular focus. | *[[Ventricular tachycardia]] originates from a [[ventricular]] focus. | ||
* Lasts more than 30 seconds. | * Lasts more than 30 seconds. | ||
* [[Broad QRS complex]]es: rate of >90 BPM. | * [[Broad QRS complex]]es: rate of >90 BPM. | ||
| Line 46: | Line 46: | ||
! style="padding: 5px 5px; background: #DCDCDC; " align="left"| '''[[Ventricular fibrillation]]''' <ref name="pmid19252119">{{cite journal |vauthors=Koplan BA, Stevenson WG |title=Ventricular tachycardia and sudden cardiac death |journal=Mayo Clin. Proc. |volume=84 |issue=3 |pages=289–97 |date=March 2009 |pmid=19252119 |pmc=2664600 |doi=10.1016/S0025-6196(11)61149-X |url=}}</ref><ref name="pmid28222965">{{cite journal |vauthors=Maury P, Sacher F, Rollin A, Mondoly P, Duparc A, Zeppenfeld K, Hascoet S |title=Ventricular arrhythmias and sudden death in tetralogy of Fallot |journal=Arch Cardiovasc Dis |volume=110 |issue=5 |pages=354–362 |date=May 2017 |pmid=28222965 |doi=10.1016/j.acvd.2016.12.006 |url=}}</ref><ref name="pmid1638716">{{cite journal |vauthors=Saumarez RC, Camm AJ, Panagos A, Gill JS, Stewart JT, de Belder MA, Simpson IA, McKenna WJ |title=Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms |journal=Circulation |volume=86 |issue=2 |pages=467–74 |date=August 1992 |pmid=1638716 |doi=10.1161/01.cir.86.2.467 |url=}}</ref><ref name="BektasSoyuncu2012">{{cite journal|last1=Bektas|first1=Firat|last2=Soyuncu|first2=Secgin|title=Hypokalemia-induced Ventricular Fibrillation|journal=The Journal of Emergency Medicine|volume=42|issue=2|year=2012|pages=184–185|issn=07364679|doi=10.1016/j.jemermed.2010.05.079}}</ref> | ! style="padding: 5px 5px; background: #DCDCDC; " align="left"| '''[[Ventricular fibrillation]]''' <ref name="pmid19252119">{{cite journal |vauthors=Koplan BA, Stevenson WG |title=Ventricular tachycardia and sudden cardiac death |journal=Mayo Clin. Proc. |volume=84 |issue=3 |pages=289–97 |date=March 2009 |pmid=19252119 |pmc=2664600 |doi=10.1016/S0025-6196(11)61149-X |url=}}</ref><ref name="pmid28222965">{{cite journal |vauthors=Maury P, Sacher F, Rollin A, Mondoly P, Duparc A, Zeppenfeld K, Hascoet S |title=Ventricular arrhythmias and sudden death in tetralogy of Fallot |journal=Arch Cardiovasc Dis |volume=110 |issue=5 |pages=354–362 |date=May 2017 |pmid=28222965 |doi=10.1016/j.acvd.2016.12.006 |url=}}</ref><ref name="pmid1638716">{{cite journal |vauthors=Saumarez RC, Camm AJ, Panagos A, Gill JS, Stewart JT, de Belder MA, Simpson IA, McKenna WJ |title=Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms |journal=Circulation |volume=86 |issue=2 |pages=467–74 |date=August 1992 |pmid=1638716 |doi=10.1161/01.cir.86.2.467 |url=}}</ref><ref name="BektasSoyuncu2012">{{cite journal|last1=Bektas|first1=Firat|last2=Soyuncu|first2=Secgin|title=Hypokalemia-induced Ventricular Fibrillation|journal=The Journal of Emergency Medicine|volume=42|issue=2|year=2012|pages=184–185|issn=07364679|doi=10.1016/j.jemermed.2010.05.079}}</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Acute coronary ischemia | *[[Coronary ischemia|Acute coronary ischemia]] | ||
*[[cardiomyopathy|Cardiomyopathies]] | *[[cardiomyopathy|Cardiomyopathies]] | ||
*[[Congenital heart disease]] | *[[Congenital heart disease]] | ||
*[[Myocardial infarction]] | *[[Myocardial infarction]] | ||
*[[Heart surgery]] | *[[Heart surgery]] | ||
*Electrolyte abnormalities | *[[Electrolyte abnormalities]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Poorly identifiable QRS complexes and absent P waves | * Poorly identifiable [[QRS complexes]] and absent [[P waves]] | ||
* The heart rate is >300 BPM | * The [[heart rate]] is >300 BPM | ||
* Rhythm is irregular | *[[Rhythm]] is irregular | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
[[File:Capture VF.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | [[File:Capture VF.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | ||
| Line 62: | Line 62: | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*[[Electrolyte disturbances]] | *[[Electrolyte disturbances]] | ||
*Medications such as: | *[[Medications]] such as: | ||
**[[ | **[[Disopyramide]] | ||
**[[Quinidine]] | **[[Quinidine]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
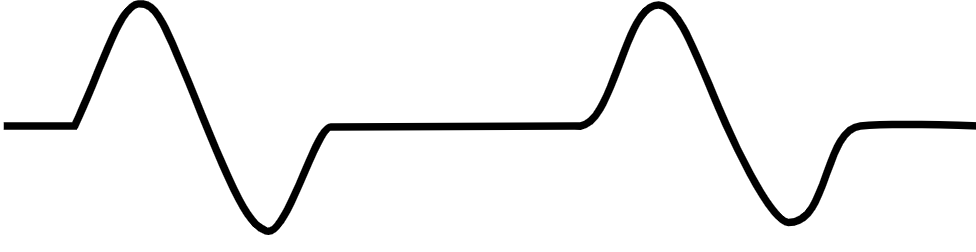
*The ECG shows: | *The [[ECG]] shows: | ||
**A typical sinusoidal pattern | **A typical [[sinusoidal]] pattern | ||
**Frequency of 300 bpm | **Frequency of 300 bpm | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
[[File:Capture Ven Flu.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | [[File:Capture Ven Flu.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | ||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | '''[[Asystole]]''' <ref name=ACLS_2003_H_T>''ACLS: Principles and Practice''. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.</ref><ref name=ACLS_2003_EP_HT>''ACLS for Experienced Providers''. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.</ref> | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | '''[[Asystole]]''' <ref name="ACLS_2003_H_T">''ACLS: Principles and Practice''. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.</ref><ref name="ACLS_2003_EP_HT">''ACLS for Experienced Providers''. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*[[Hypovolemia]] | *[[Hypovolemia]] | ||
| Line 96: | Line 96: | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | '''[[Pulseless electrical activity]]''' <ref name="ECC_2005_7.2">"2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." ''Circulation'' 2005; '''112''': IV-58 - IV-66.</ref><ref>Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007</ref> | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | '''[[Pulseless electrical activity]]''' <ref name="ECC_2005_7.2">"2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." ''Circulation'' 2005; '''112''': IV-58 - IV-66.</ref><ref>Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Hypovolemia | *[[Hypovolemia]] | ||
*Hypoxia | *[[Hypoxia]] | ||
*Hydrogen ions (Acidosis) | *Hydrogen ions ([[Acidosis]]) | ||
*Hypothermia | *[[Hypothermia]] | ||
*[[Electrolyte disturbances]] | *[[Electrolyte disturbances]] | ||
*Hypoglycemia | *[[Hypoglycemia]] | ||
*Tablets or Toxins (Drug overdose) such as beta blockers, tricyclic antidepressants, or calcium channel blockers | *[[Tablets]] or [[Toxins]] (Drug overdose) such as [[beta blockers]], [[tricyclic antidepressants]], or [[Calcium channel blocker|calcium channel blockers]] | ||
*Tamponade | *[[Cardiac tamponade|Tamponade]] | ||
*Tension pneumothorax | *[[Tension pneumothorax]] | ||
*Thrombosis (Myocardial infarction) | *[[Thrombosis]] ([[Myocardial infarction]]) | ||
*Thrombosis (Pulmonary embolism) | *[[Thrombosis]] ([[Pulmonary embolism]]) | ||
*Trauma (Hypovolemia from blood loss) | *[[Trauma]] ([[Hypovolemia]] from [[blood loss]]) | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Several | *Several pattern are possible including: | ||
**Normal sinus rhythm | **[[Normal sinus rhythm]] | ||
**Sinus tachycardia, with discernible P waves and QRS complexes | **[[Sinus tachycardia]], with discernible [[P waves]] and [[QRS complexes]] | ||
**Bradycardia, with or without P waves | **[[Bradycardia]], with or without [[P waves]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
[[File:Capture PEA.PNG|center|300px]]<ref> ECG found in wikimedia Commons </ref> | [[File:Capture PEA.PNG|center|300px]]<ref> ECG found in wikimedia Commons </ref> | ||
| Line 135: | Line 135: | ||
** [[Ziprasidone]] | ** [[Ziprasidone]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
# Paroxysms of VT with irregular RR intervals. | # Paroxysms of [[VT]] with irregular RR intervals. | ||
# A ventricular rate between 200 and 250 beats per minute. | # A [[ventricular]] rate between 200 and 250 beats per minute. | ||
# Two or more cycles of [[QRS complex]]es with alternating polarity. | # Two or more cycles of [[QRS complex]]es with alternating polarity. | ||
# Changing amplitude of the QRS complexes in each cycle in a sinusoidal fashion. | # Changing amplitude of the [[QRS complexes]] in each cycle in a sinusoidal fashion. | ||
# Prolongation of the [[QT interval]]. | # Prolongation of the [[QT interval]]. | ||
# Is often initiated by a [[PVC]] with a long coupling interval, R on T phenomenon. | # Is often initiated by a [[PVC]] with a long coupling interval, R on T phenomenon. | ||
Latest revision as of 18:13, 29 January 2020
|
Torsades de pointes Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Torsades de pointes differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Torsades de pointes differential diagnosis |
|
Risk calculators and risk factors for Torsades de pointes differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Torsades de pointes should be differentiated from other conditions or disorders that may present in a similar way, such as other arrhythmias, drug toxicity, syncope and other cardiac conditions.
Differential Diagnosis
- Ventricular Tachycardia (polymorphic, monomorphic)
- Supraventricular tachycardia
- Ventricular Fibrillation
- Sudden Cardiac Death
- Syncope
- Renal Failure
- Complication dialysis
- Drug toxicity like antiarrhythmic, antihistaminics
The table below provides information on the differential diagnosis of torsades de pointes in terms of ECG appearance:
| Disease Name | Causes | ECG Characteristics | ECG view |
|---|---|---|---|
| Ventricular tachycardia [1][2][3][4][5] |
|
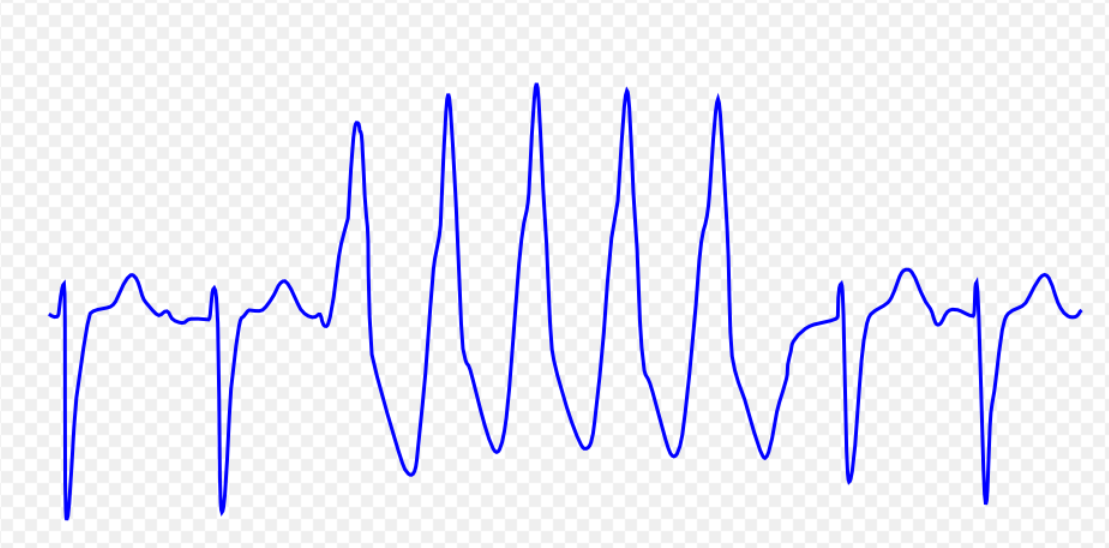 | |
| Ventricular fibrillation [7][8][9][10] |
|
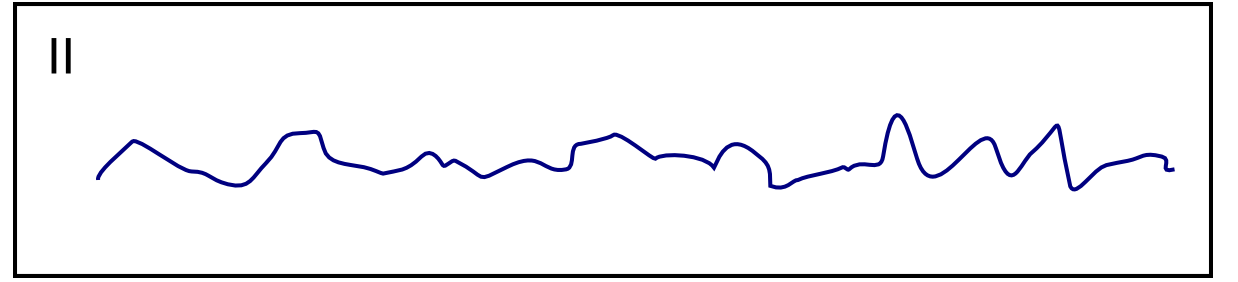 | |
| Ventricular flutter [12][13][14] |
|
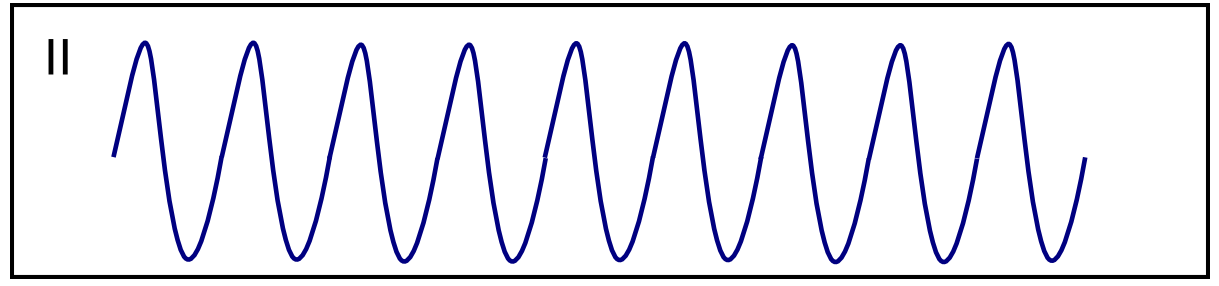 | |
| Asystole [16][17] |
|
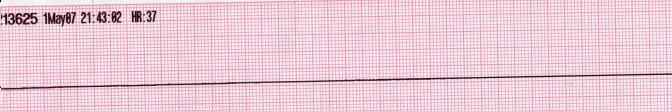 | |
| Pulseless electrical activity [19][20] |
|
|
 |
| Torsade de Pointes [22][23][24] |
|
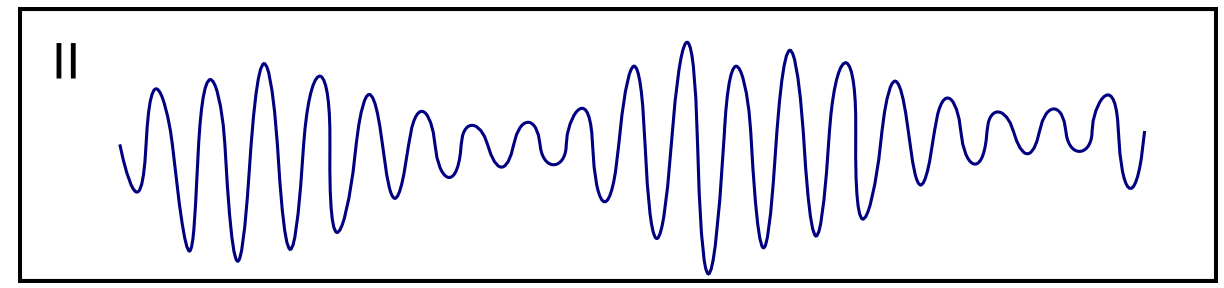 |
References
- ↑ Ajijola, Olujimi A.; Tung, Roderick; Shivkumar, Kalyanam (2014). "Ventricular tachycardia in ischemic heart disease substrates". Indian Heart Journal. 66: S24–S34. doi:10.1016/j.ihj.2013.12.039. ISSN 0019-4832.
- ↑ Meja Lopez, Eliany; Malhotra, Rohit (2019). "Ventricular Tachycardia in Structural Heart Disease". Journal of Innovations in Cardiac Rhythm Management. 10 (8): 3762–3773. doi:10.19102/icrm.2019.100801. ISSN 2156-3977.
- ↑ Coughtrie, Abigail L; Behr, Elijah R; Layton, Deborah; Marshall, Vanessa; Camm, A John; Shakir, Saad A W (2017). "Drugs and life-threatening ventricular arrhythmia risk: results from the DARE study cohort". BMJ Open. 7 (10): e016627. doi:10.1136/bmjopen-2017-016627. ISSN 2044-6055.
- ↑ El-Sherif, Nabil (2001). "Mechanism of Ventricular Arrhythmias in the Long QT Syndrome: On Hermeneutics". Journal of Cardiovascular Electrophysiology. 12 (8): 973–976. doi:10.1046/j.1540-8167.2001.00973.x. ISSN 1045-3873.
- ↑ de Riva, Marta; Watanabe, Masaya; Zeppenfeld, Katja (2015). "Twelve-Lead ECG of Ventricular Tachycardia in Structural Heart Disease". Circulation: Arrhythmia and Electrophysiology. 8 (4): 951–962. doi:10.1161/CIRCEP.115.002847. ISSN 1941-3149.
- ↑ ECG found in of https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ Koplan BA, Stevenson WG (March 2009). "Ventricular tachycardia and sudden cardiac death". Mayo Clin. Proc. 84 (3): 289–97. doi:10.1016/S0025-6196(11)61149-X. PMC 2664600. PMID 19252119.
- ↑ Maury P, Sacher F, Rollin A, Mondoly P, Duparc A, Zeppenfeld K, Hascoet S (May 2017). "Ventricular arrhythmias and sudden death in tetralogy of Fallot". Arch Cardiovasc Dis. 110 (5): 354–362. doi:10.1016/j.acvd.2016.12.006. PMID 28222965.
- ↑ Saumarez RC, Camm AJ, Panagos A, Gill JS, Stewart JT, de Belder MA, Simpson IA, McKenna WJ (August 1992). "Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms". Circulation. 86 (2): 467–74. doi:10.1161/01.cir.86.2.467. PMID 1638716.
- ↑ Bektas, Firat; Soyuncu, Secgin (2012). "Hypokalemia-induced Ventricular Fibrillation". The Journal of Emergency Medicine. 42 (2): 184–185. doi:10.1016/j.jemermed.2010.05.079. ISSN 0736-4679.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ Thies, Karl-Christian; Boos, Karin; Müller-Deile, Kai; Ohrdorf, Wolfgang; Beushausen, Thomas; Townsend, Peter (2000). "Ventricular flutter in a neonate—severe electrolyte imbalance caused by urinary tract infection in the presence of urinary tract malformation". The Journal of Emergency Medicine. 18 (1): 47–50. doi:10.1016/S0736-4679(99)00161-4. ISSN 0736-4679.
- ↑ Koster, Rudolph W.; Wellens, Hein J.J. (1976). "Quinidine-induced ventricular flutter and fibrillation without digitalis therapy". The American Journal of Cardiology. 38 (4): 519–523. doi:10.1016/0002-9149(76)90471-9. ISSN 0002-9149.
- ↑ Dhurandhar RW, Nademanee K, Goldman AM (1978). "Ventricular tachycardia-flutter associated with disopyramide therapy: a report of three cases". Heart Lung. 7 (5): 783–7. PMID 250503.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ ACLS: Principles and Practice. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.
- ↑ ACLS for Experienced Providers. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." Circulation 2005; 112: IV-58 - IV-66.
- ↑ Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007
- ↑ ECG found in wikimedia Commons
- ↑ Li M, Ramos LG (July 2017). "Drug-Induced QT Prolongation And Torsades de Pointes". P T. 42 (7): 473–477. PMC 5481298. PMID 28674475.
- ↑ Sharain, Korosh; May, Adam M.; Gersh, Bernard J. (2015). "Chronic Alcoholism and the Danger of Profound Hypomagnesemia". The American Journal of Medicine. 128 (12): e17–e18. doi:10.1016/j.amjmed.2015.06.051. ISSN 0002-9343.
- ↑ Khan IA (2001). "Twelve-lead electrocardiogram of torsades de pointes". Tex Heart Inst J. 28 (1): 69. PMC 101137. PMID 11330748.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page