Thyroid-stimulating hormone
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
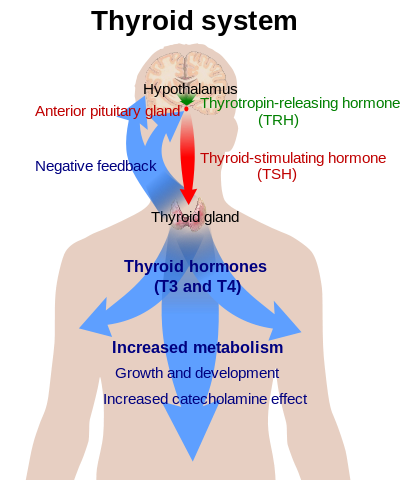
Thyroid-stimulating hormone (also known as thyrotropin, TSH, or hTSH for human TSH) is a pituitary hormone that stimulates the thyroid gland to produce thyroxine (T4), and then triiodothyronine (T3) which stimulates the metabolism of almost every tissue in the body.[1] It is a glycoprotein hormone synthesized and secreted by thyrotrope cells in the anterior pituitary gland, which regulates the endocrine function of the thyroid.[2][3]
Physiology
Regulation of thyroid hormone levels
TSH (with a half life of about an hour) stimulates the thyroid gland to secrete the hormone thyroxine (T4), which has only a slight effect on metabolism. T4 is converted to triiodothyronine (T3), which is the active hormone that stimulates metabolism. About 80% of this conversion is in the liver and other organs, and 20% in the thyroid itself.[1]
TSH is secreted throughout life but particularly reaches high levels during the periods of rapid growth and development.
The hypothalamus, in the base of the brain, produces thyrotropin-releasing hormone (TRH). TRH stimulates the pituitary gland to produce TSH.
Somatostatin is also produced by the hypothalamus, and has an opposite effect on the pituitary production of TSH, decreasing or inhibiting its release.
The concentration of thyroid hormones (T3 and T4) in the blood regulates the pituitary release of TSH; when T3 and T4 concentrations are low, the production of TSH is increased, and, conversely, when T3 and T4 concentrations are high, TSH production is decreased. This is an example of a negative feedback loop.[5] Any inappropriateness of measured values, for instance a low-normal TSH together with a low-normal T4 may signal tertiary (central)disease and a TSH to TRH pathology. Elevated reverse T3 (RT3) together with low-normal TSH and low-normal T3, T4 values, which is regarded as indicative for euthyroid sick syndrome, may also have to be investigated for chronic subacute thyroiditis (SAT) with output of subpotent hormones. Absence of antibodies in patients with diagnoses of an autoimmune thyroid in their past would always be suspicious for development to SAT even in the presence of a normal TSH because there is no known recovery from autoimmunity.
Subunits
TSH is a glycoprotein and consists of two subunits, the alpha and the beta subunit.
- The α (alpha) subunit (i.e., chorionic gonadotropin alpha) is nearly identical to that of human chorionic gonadotropin (hCG), luteinizing hormone (LH), and follicle-stimulating hormone (FSH). The α subunit is thought to be the effector region responsible for stimulation of adenylate cyclase (involved the generation of cAMP).[6] The α chain has a 92-amino acid sequence.
- The β (beta) subunit (TSHB) is unique to TSH, and therefore determines its receptor specificity.[7] The β chain has a 118-amino acid sequence.
The TSH receptor
The TSH receptor is found mainly on thyroid follicular cells.[8] Stimulation of the receptor increases T3 and T4 production and secretion. Stimulating antibodies to this receptor mimic TSH and cause Graves' disease. In addition, hCG shows some cross-reactivity to the TSH receptor and therefore can stimulate production of thyroid hormones. In pregnancy, prolonged high concentrations of hCG can produce a transient condition termed gestational hyperthyroidism.[9] This is also the mechanism of trophoblastic tumors increasing the production of thyroid hormones.
Applications
Diagnostics
Reference ranges for TSH may vary slightly, depending on the method of analysis, and do not necessarily equate to cut-offs for diagnosing thyroid dysfunction. In the UK, guidelines issued by the Association for Clinical Biochemistry suggest a reference range of 0.4-4.5 µIU/mL.[10] The National Academy of Clinical Biochemistry (NACB) stated that it expected the reference range for adults to be reduced to 0.4–2.5 µIU/mL, because research had shown that adults with an initially measured TSH level of over 2.0 µIU/mL had "an increased odds ratio of developing hypothyroidism over the [following] 20 years, especially if thyroid antibodies were elevated".[11]
TSH concentrations in children are normally higher than in adults. In 2002, the NACB recommended age-related reference limits starting from about 1.3 to 19 µIU/mL for normal-term infants at birth, dropping to 0.6–10 µIU/mL at 10 weeks old, 0.4–7.0 µIU/mL at 14 months and gradually dropping during childhood and puberty to adult levels, 0.3–3.0 µIU/mL.[12]:Section 2
Diagnosis of disease
TSH concentrations are measured as part of a thyroid function test in patients suspected of having an excess (hyperthyroidism) or deficiency (hypothyroidism) of thyroid hormones. Interpretation of the results depends on both the TSH and T4 concentrations. In some situations measurement of T3 may also be useful.
| Source of pathology | TSH level | Thyroid hormone level | Disease causing conditions |
|---|---|---|---|
| Hypothalamus/pituitary | High | High | Benign tumor of the pituitary (adenoma) or thyroid hormone resistance |
| Hypothalamus/pituitary | Low | Low | Secondary hypothyroidism or "central" hypothyroidism |
| Thyroid | Low | High | Primary hyperthyroidism i.e. Graves' disease |
| Thyroid | High | Low | Congenital hypothyroidism (cretinism), Primary hypothyroidism i.e. Hashimoto's thyroiditis |
A TSH assay is now also the recommended screening tool for thyroid disease. Recent advances in increasing the sensitivity of the TSH assay make it a better screening tool than free T4.[3]
Monitoring
The therapeutic target range TSH level for patients on treatment ranges between 0.3 to 3.0 μIU/mL.[12]
For hypothyroid patients on thyroxine, measurement of TSH alone is generally considered sufficient. An increase in TSH above the normal range indicates under-replacement or poor compliance with therapy. A significant reduction in TSH suggests over-treatment. In both cases, a change in dose may be required. A low or low-normal TSH value may also signal pituitary disease. TSH measurements could not be applied any more, however, treatment would have to be continued.
For hyperthyroid patients, both TSH and T4 are usually monitored.
Therapeutic
A synthetic drug called recombinant human TSH alpha (rhTSHα or simply rhTSH, (trade name Thyrogen), is manufactured by Genzyme Corp. The rhTSH is used to treat thyroid cancer.[13]
References
- ↑ 1.0 1.1 Merck Manual of Diagnosis and Therapy, Thyroid gland disorders.
- ↑ The American Heritage Dictionary of the English Language, Fourth Edition. Houghton Mifflin Company. 2006. ISBN 0-395-82517-2.
- ↑ 3.0 3.1 Sacher, Ronald; Richard A. McPherson (2000). Widmann's Clinical Interpretation of Laboratory Tests, 11th ed. F.A. Davis Company. ISBN 0-8036-0270-7.
- ↑ References used in image are found in image article in Commons:Commons:File:Thyroid system.png#References.
- ↑ Thyroid volume 24;#3;p. 411
- ↑ Lalli, E; Sassone-Corsi, P (Oct 10, 1995). "Thyroid-stimulating hormone (TSH)-directed induction of the CREM gene in the thyroid gland participates in the long-term desensitization of the TSH receptor" (PDF). Proceedings of the National Academy of Sciences of the United States of America. 92 (21): 9633–7. doi:10.1073/pnas.92.21.9633. PMC 40856. PMID 7568187.
- ↑ Porcellini, A (Oct 17, 2003). "The expression of the thyroid-stimulating hormone (TSH) receptor and the cAMP-dependent protein kinase RII beta regulatory subunit confers TSH-cAMP-dependent growth to mouse fibroblasts". The Journal of Biological Chemistry. 278 (42): 40621–30. doi:10.1074/jbc.M307501200. PMID 12902333. Unknown parameter
|coauthors=ignored (help) - ↑ Parmentier M, Libert F, Maenhaut C, Lefort A, Gérard C, Perret J, Van Sande J, Dumont JE, Vassart G (December 1989). "Molecular cloning of the thyrotropin receptor". Science. 246 (4937): 1620–2. doi:10.1126/science.2556796. PMID 2556796.
- ↑ Fantz CR, Dagogo-Jack S, Ladenson JH, Gronowski AM (December 1999). "Thyroid function during pregnancy". Clin. Chem. 45 (12): 2250–8. PMID 10585360.
- ↑ Use of thyroid function tests: guidelines development group (2006-06-01). "UK Guidelines for the Use of Thyroid Function Tests" (pdf). Retrieved 2014-01-14.
- ↑ Baloch Z, Carayon P, Conte-Devolx B, Demers LM, Feldt-Rasmussen U, Henry JF, LiVosli VA, Niccoli-Sire P, John R, Ruf J, Smyth PP, Spencer CA, Stockigt JR (January 2003). "Laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease". Thyroid. 13 (1): 3–126. doi:10.1089/105072503321086962. PMID 12625976.
- ↑ 12.0 12.1 Baskin; et al. (2002). "AACE Medical Guidelines for Clinical Practice for Evaluation and Treatment of Hyperthyroidism and Hypothyroidism" (PDF). American Association of Clinical Endocrinologists. pp. 462, 465.
- ↑ Duntas LH, Tsakalakos N, Grab-Duntas B, Kalarritou M, Papadodima E (2003). "The use of recombinant human thyrotropin (Thyrogen) in the diagnosis and treatment of thyroid cancer". Hormones (Athens). 2 (3): 169–74. doi:10.14310/horm.2002.1197. PMID 17003018.
External links
- TSH at Lab Tests Online
- MedlinePlus Encyclopedia 003684
- Thyrotropin at the US National Library of Medicine Medical Subject Headings (MeSH)