Spinal cord: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 15:25, 7 July 2010
|
WikiDoc Resources for Spinal cord |
|
Articles |
|---|
|
Most recent articles on Spinal cord Most cited articles on Spinal cord |
|
Media |
|
Powerpoint slides on Spinal cord |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Spinal cord at Clinical Trials.gov Clinical Trials on Spinal cord at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Spinal cord
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Spinal cord Discussion groups on Spinal cord Patient Handouts on Spinal cord Directions to Hospitals Treating Spinal cord Risk calculators and risk factors for Spinal cord
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Spinal cord |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview


The spinal cord is a thin, tubular bundle of nerves that is an extension of the central nervous system from the brain and is enclosed in and protected by the bony vertebral column. The main function of the spinal cord is transmission of neural inputs between the periphery and the brain.
Structure
The human spinal cord extends from the medulla oblongata in the brain and continues to the conus medullaris near the lumbar level at L1-2, terminating in a fibrous extension known as the filum terminale.
It is about 45 cm long in men and 42 cm long in women, ovoid-shaped, and is enlarged in the cervical and lumbar regions. The peripheral regions of the cord contains neuronal white matter tracts containing sensory and motor neurons. The central region is a four-leaf clover shape that surrounds the central canal (an anatomic extension of the fourth ventricle) and contains nerve cell bodies.
The three meninges that cover the spinal cord -- the outer dura mater, the arachnoid membrane, and the innermost pia mater -- are continuous with that in the brainstem and cerebral hemispheres, with cerebrospinal fluid found in the subarachnoid space. The cord within the pia mater is stabilized within the dura mater by the connecting denticulate ligaments which extends from the pia mater laterally between the dorsal and ventral roots. The dural sac ends at the vertebral level of S2.
Sensory Organization
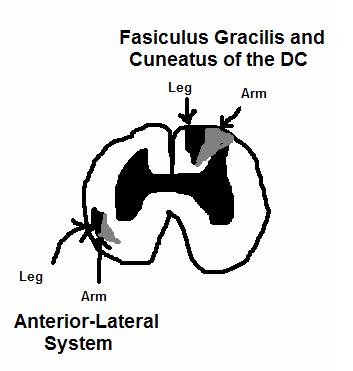
Somatosensory organization is divided into a touch/proprioception/vibration sensory pathway and a pain/temperature sensory pathway, which are more formally known as the dorsal column-medial lemniscus tract and the spinothalamic tract, respectively.
Each of these sensory pathways utilizes three different neurons to get from the sensory receptors to the cerebral cortex. These neurons are designated primary, secondary and tertiary sensory neurons. The primary neuron has its cell body in the dorsal root ganglia and its axon projects into the spinal cord.
In the case of the touch/proprioception/vibration sensory pathway, the primary neuron enters the spinal cord and travels in the dorsal column. Below level T6, the neuron travels in the fasciculus gracilis - the most medial part of the column. Above level T6, the neuron enters the fasciculus cuneatus - lateral to the fasiculus gracilis.
As the primary axons reach the caudal medulla, they leave their respective fasiculi and enter and synapse on secondary neurons within the nucleus gracilis and the nucleus cuneatus, respectively. At this point, the seconday neuronal axons decussate and continue to ascend as the medial leminiscus. They run up to the VPL nucleus of the thalamus,and synapse there on the tertiary neurons. From there, the tertiary neurons ascend via the posterior limb of the internal capsule to the post central gyrus, or Brodmann's Area 3,1,2.
The pain/temperature sensory pathway differs from that of the touch/proprioception/vibration pathway. The pain neurons enter as primary neurons and ascend 1-2 levels before synapsing in the substantia gelatinosa. The tract that ascends those 1-2 levels before synapsing is known as Lissauer's tract. After synapsing, the secondary neurons cross decussate and ascend as the spinothalamic tract in the anterior lateral portion of the spinal cord. Hence, the spinothalamic tract is also known as the anterior lateral system (ALS). The tract ascends all the way to the VPL of the thalamus where it synapses on the tertiary neurons. The tertiary neuronal axons then project via the posterior limb of the internal capsule to the post-central gyrus or Broadmann's Area 3,1,2.
It should be noted that the pain fibers in the ALS can also deviate in their pathway towards the VPL. In one pathway, the axons project towards the reticular formation in the midbrain. The reticular formation then project to a number of places including the hippocampus (to create memories about the pain), to the centromedian nucleus (to cause diffuse, non-specific pain) and the various places on the cortex. The third place that the neurons project to is the periaqueductal gray in the pons. The neurons form the periaqueductal gray then project to the nucleus raphe magnus which projects back down to where the pain signal is coming in from and inhibits it. This reduces the pain sensation to some degree.
Motor Organization
Upper motor neuronal input comes from two places- first from the cerebral cortex and second from more primitive brain stem nuclei. Cortical upper motor neurons originate in Brodmann Areas 4, 6, 3, 1 and 2. They then descend through the genu and the posterior limb of the internal capsule. This pathway is known as the corticospinal tract. After passing through the internal capsule, the tract descends through the cerebral peduncles, down through the pons and to the medullary pyramids. At this point, ~85% of these upper motor neuronal axons decussate. These fibers then descend as the lateral corticospinal tract. The remaining ~15% descend as the anterior corticospinal tract.
The midbrain nuclei include four motor tracts that send upper motor neuronal axons down the spinal cord to lower motor neurons. These are the rubrospinal tract, the vestibulospinal tract, the tectospinal tract and the reticulospinal tract. The rubrospinal tract descends with the lateral corticospinal tract and the remaining three descend with the anterior corticospinal tract.
The function of lower motor neurons can be divided into two different groups--first,the lateral corticospinal tract and second, the anterior cortical spinal tract. The lateral tract contains upper motor neuronal axons which synapse on dorsal lateral (DL) lower motor neurons. The DL neurons are involved in distal limb control. Therefore, these DL neurons are found specifically only in the cervical and lumbosaccral enlargements within the spinal cord. There is no decussation in the lateral corticospinal tract after the decussation at the medullary pyramids.
The anterior corticospinal tract descends ipsilaterally in the anterior column where the axons emerge and either synapse on lower motor neurons, known as ventromedial (VM) lower motor neurons, in the ventral horn ipsilaterally, or descussate at the anterior white commissure where they synapse on VM lower motor neurons contralaterally . The tectospinal, vestibulospinal and reticulospinal descend ipsilaterally in the anterior column, but do not synapse across the anterior white commissure. Rather, they only synapse on VM lower motor neurons ipsilaterally. The VM lower motor neurons control axial motor function-- the large, postural muscles. These lower motor neurons, unlike those of the DL, are located in the ventral horn all the way throughout the spinal cord.
Spinocerebellar Tracts
Proprioceptiveinformation in the body travels up the spinal cord via three tracts. Below L2 the proprioceptive information travels up the spinal cord in the ventral spinocerebellar tract. Also known as the anterior spinocerebellar tract, sensory receptors take in the information and travel into the spinal cord. The cell bodies of these primary neurons are located in the dorsal root ganglia. In the spinal cord, the axons synapse and the secondary neuronal axons decussate and then travel up to the superior cerebellar peduncle where they decussate again. From here, the information is brought to deep nuclei of the cerebellum including the fastigial and interposed nuclei.
From the levels of L2 to T1, the proprioceptive information enters the spinal cord and ascends ipsilaterally where it synapses in the Dorsal Nucleus of Clark. The secondary neuronal axons continue to ascend ispilaterally and enter the pass into the cerebellum via the inferior cerebellar peduncle. This tract is known as the dorsal spinocerebellar tract and also as the posterior spinocerebellar tract.
From above T1, proprioceptive primary axons enter the spinal cord and ascend ipsilaterally until reaching the accessory cuneate nucleus, where they synapse. The secondary axons pass into the cerebellum via the inferior cerebellar peduncle where again, these axons synapse on cerebellar deep nuclei. This tract is known as the cuneocerebellar tract.
Spinal cord segments
The human spinal cord is divided into 31 different segments, with motor nerve roots exiting in the ventral aspects and sensory nerve roots entering in the dorsal aspects. The ventral and dorsal roots later join to form paired spinal nerves, one on each side of the spinal cord.
There are 31 spinal cord nerve segments in a human spinal cord:
- 8 cervical segments (cervical nerves exit spinal column above C1 and below C1-C7)
- 12 thoracic segments (nerves exit spinal column below T1-T12)
- 5 lumbar segments (nerves exit spinal column below L1-L5)
- 5 sacral segments (nerves exit spinal column below S1-S5)
- 1 coccygeal segment (nerves exit spinal column at coccyx)
Because the vertebral column grows longer than the spinal cord, spinal cord segments become higher than the corresponding vertebra, especially in the lower spinal cord segments in adults. In a fetus, the vertebral levels originally correspond with the spinal cord segments. In the adult, the cord ends around the L1/L2 vertebral level at the conus medullaris, with all of the spinal cord segments located superiorly to this. For example, the segments for the lumbar and sacral regions are found between the vertebral levels of T9 and L2. The S4 spinal nerve roots arise from the cord around the upper lumbar/lower thoracic vertebral region, and descend downward in the vertebral canal. After they pass the end of the spinal cord, they are considered to be part of the cauda equina. The roots for S4 finally leave the vertebral canal in the sacrum.
There are two regions where the spinal cord enlarges:
- Cervical enlargement - corresponds roughly to the brachial plexus nerves, which innervate the upper limb. It includes spinal cord segments from about C4 to T1. The vertebral levels of the enlargement are roughly the same (C4 to T1).
- Lumbosacral enlargement - corresponds to the lumbosacral plexus nerves, which innervate the lower limb. It comprises the spinal cord segments from L2 to S3, and is found about the vertebral levels of T9 to T12.
Embryology
The spinal cord is made from part of the neural tube during development. As the neural tube begins to develop, the notochord begins to secrete a factor known as Sonic hedgehog or SHH. As a result, the floor plate then also begins to secrete SHH and this will induce the basal plate to develop motor neurons. Meanwhile, the overlying ectoderm secretes bone morphogenetic protein (BMP). This will induce the roof plate to begin to also secrete BMP which will induce the alar plate to develop sensory neurons. The alar plate and the basal plate are separated by the sulcus limitans.
Additionally, the floor plate will also secrete netrins. The netrins act as chemoattractants to decussation of pain and temperature sensory neurons in the alar plate across the anterior white commissure where they will then ascend towards the thalamus.
Lastly it is important to note that the past studies of Viktor Hamburger and Rita Levi-Montalcini in the chick embryo have been further proven by more recent studies which demonstrated that the elimination of neuronal cells by programmed cell death (PCD) is necessary for the correct assembly of the nervous system.
Overall, spontaneous embryonic activity has been shown to play a role in neuron and muscle development, but is probably not involved in the initial formation of connections between spinal neurons.
Injury
Spinal cord injuries can be caused by falling on the neck or back, or having the spinal cord moved or disrupted in another way. The vertebral bones or intervertebral disks can shatter, causing the spinal cord to be punctured by a sharp fragment of bone. Usually victims of spinal cord injuries will suffer loss of feeling in certain parts of their body. In milder cases a victim might only suffer loss of hand or foot function. More severe injury may result in paraplegia, tetraplegia, or full body paralysis below the site of injury to the spinal cord.
Damage to upper motor neurons axons in the spinal cord results in a characteristic pattern of ipsilateral deficits. These include hyperreflexia, hypertonia and muscle weakness. Lower motor neuronal damage results in its own characteristic pattern of deficits. Rather than an entire side of deficits, there is a pattern relating to the myotome affected by the damage. Additionally, lower motor neurons are characterized by muscle weakness, hypotonia, hyporeflexia and muscle atrophy.
The two areas of the spinal cord most commonly injured are the cervical spine (C1-C7) and the lumbar spine (L1-L5). (The notation C1, C7, L1, L5 refer to the location of a specific vertebra in either the cervical, thoracic, or lumbar region of the spine.)
Additional images
-
Diagrams of the spinal cord.
-
Cross-section through the spinal cord at the mid-thoracic level.
-
Cross-sections of the spinal cord at varying levels.
See also
External links
- Spinal Cord Histology - A multitude of great Images from the University of Cincinnati
- Spinal Cord Medical Notes - Online medical notes on the Spinal Cord
- eMedicine: Spinal Cord, Topographical and Functional Anatomy
- WebMD. May 17, 2005. Spina Bifida - Topic Overview Information about Spina Bifida in fetuses and throughout adulthood. WebMD children's health. Retrieved March 19, 2007.
Template:SIB Template:Nervous system Template:Spinal cord Template:Vertebral column and spinal cord
bs:Kičmena moždina ca:Medul·la espinal cs:Mícha de:Rückenmark eo:Mjelo id:Sumsum tulang belakang is:Mæna it:Midollo spinale he:חוט השדרה la:Medulla spinalis lt:Nugaros smegenys mk:‘Рбетен мозок nl:Ruggenmerg sk:Miecha sl:Hrbtenjača sr:Кичмена мождина fi:Selkäydin sv:Ryggmärg uk:Спинний мозок tl:Kurdong panggulugod