Sandbox:Sahar: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{| class="wikitable" | |||
|+ | |||
|- | |||
| align="center" style="background:#4479BA; color: #FFFFFF;" |'''Type of paraneoplastic syndrome''' | |||
| align="center" style="background:#4479BA; color: #FFFFFF;" |'''Subtype''' | |||
| align="center" style="background:#4479BA; color: #FFFFFF;" |'''Associated Cancers''' | |||
|- | |||
| rowspan="5" align="center" style="background:#f0f0f0;" |[[Endocrine]] | |||
| | |||
* [[Hypercalcemia]]<ref name="Stewart2005">{{cite journal|last1=Stewart|first1=Andrew F.|title=Hypercalcemia Associated with Cancer|journal=New England Journal of Medicine|volume=352|issue=4|year=2005|pages=373–379|issn=0028-4793|doi=10.1056/NEJMcp042806}}</ref> | |||
| | |||
* [[Breast cancer]] and [[lung cancer]] (typically [[Squamous cell carcinoma|squamous cell]]) due to the production of [[Parathyroid hormone-related protein|PTHrP]] ([[Parathyroid hormone]]-related [[protein]])[[multiple myeloma]], [[renal cell carcinoma]], [[ovarian cancer]], [[endometrial cancer]], and [[lymphoma]] | |||
* | |||
|- | |||
| | |||
* [[Syndrome of inappropriate antidiuretic hormone|SIADH]]<ref name="Raftopoulos2007">{{cite journal|last1=Raftopoulos|first1=Harry|title=Diagnosis and management of hyponatremia in cancer patients|journal=Supportive Care in Cancer|volume=15|issue=12|year=2007|pages=1341–1347|issn=0941-4355|doi=10.1007/s00520-007-0309-9}}</ref> | |||
| | |||
* [[Small cell lung cancer|Small-cell lung cancer]], [[mesothelioma]], [[breast]], [[prostate]], [[adrenal]], [[urethral]], [[thymoma]], [[lymphoma]], GI, CNS, and [[Ewing sarcoma]] | |||
* | |||
|- | |||
| | |||
* [[Ectopic]] [[ACTH]] [[secretion]]<ref name="BarbosaRodien2005">{{cite journal|last1=Barbosa|first1=Sandrine Laboureau-Soares|last2=Rodien|first2=Patrice|last3=Leboulleux|first3=Sophie|last4=Niccoli-Sire|first4=Patricia|last5=Kraimps|first5=Jean-Louis|last6=Caron|first6=Philippe|last7=Archambeaud-Mouveroux|first7=Françoise|last8=Conte-Devolx|first8=Bernard|last9=Rohmer|first9=Vincent|title=Ectopic Adrenocorticotropic Hormone-Syndrome in Medullary Carcinoma of the Thyroid: A Retrospective Analysis and Review of the Literature|journal=Thyroid|volume=15|issue=6|year=2005|pages=618–623|issn=1050-7256|doi=10.1089/thy.2005.15.618}}</ref> | |||
| | |||
* [[Small cell lung cancer|Small-cell lung cancer]], [[carcinoid tumor]], [[thymoma]], [[medullary carcinoma of the thyroid]] and other [[Cancer|cancers]] | |||
|- | |||
| | |||
* [[Tumor induced osteomalacia]]<ref name="FlorenzanoGafni2017">{{cite journal|last1=Florenzano|first1=Pablo|last2=Gafni|first2=Rachel I.|last3=Collins|first3=Michael T.|title=Tumor-induced osteomalacia|journal=Bone Reports|volume=7|year=2017|pages=90–97|issn=23521872|doi=10.1016/j.bonr.2017.09.002}}</ref> | |||
| | |||
* [[Metastatic]] [[breast cancer]] | |||
* | |||
|- | |||
| | |||
* [[Hypoglycemia]]<ref name="NauckReinecke2007">{{cite journal|last1=Nauck|first1=Michael A.|last2=Reinecke|first2=Manfred|last3=Perren|first3=Aurel|last4=Frystyk|first4=Jan|last5=Berishvili|first5=Giorgi|last6=Zwimpfer|first6=Cornelia|last7=Figge|first7=Anja M.|last8=Flyvbjerg|first8=Allan|last9=Lankisch|first9=Paul G.|last10=Blum|first10=Werner F.|last11=Klöppel|first11=Günter|last12=Schmiegel|first12=Wolff|last13=Zapf|first13=Jürgen|title=Hypoglycemia due to Paraneoplastic Secretion of Insulin-Like Growth Factor-I in a Patient with Metastasizing Large-Cell Carcinoma of the Lung|journal=The Journal of Clinical Endocrinology & Metabolism|volume=92|issue=5|year=2007|pages=1600–1605|issn=0021-972X|doi=10.1210/jc.2006-2573}}</ref> | |||
| | |||
* [[Gastrointestinal tract|GI]] cancers, [[mesothelioma]], [[lung]], [[real cancer]], and [[sarcomas]] | |||
|- | |||
| rowspan="6" align="center" style="background:#f0f0f0;" |[[Mucocutaneous|Musculocutaneous]] | |||
| | |||
* [[Dermatomyositis]]<ref name="ThiersSahn2009">{{cite journal|last1=Thiers|first1=B. H.|last2=Sahn|first2=R. E.|last3=Callen|first3=J. P.|title=Cutaneous Manifestations of Internal Malignancy|journal=CA: A Cancer Journal for Clinicians|volume=59|issue=2|year=2009|pages=73–98|issn=0007-9235|doi=10.3322/caac.20005}}</ref> | |||
| | |||
* [[Breast cancer|Breast]], [[Ovarian cancer|ovarian]], [[Lung cancer|lung]], and [[prostate cancer]] | |||
* | |||
|- | |||
| | |||
* [[Leser-Trelat sign|Leser-Trélat sign]]<ref name="GaduputiChandrala2014">{{cite journal|last1=Gaduputi|first1=Vinaya|last2=Chandrala|first2=Chaitanya|last3=Tariq|first3=Hassan|last4=Kanneganti|first4=Kalyan|title=Sign of Leser-Trélat Associated with Esophageal Squamous Cell Cancer|journal=Case Reports in Oncological Medicine|volume=2014|year=2014|pages=1–3|issn=2090-6706|doi=10.1155/2014/825929}}</ref> | |||
| | |||
* Gastrointestinal [[adenocarcinomas]] ([[Gastric adenocarcinoma|gastric]], [[Colon adenocarcinoma|colon]], rectal), [[breast cancer]], [[lymphoproliferative disorders]]/[[lymphoma]], and [[melanoma]]. | |||
* | |||
|- | |||
| | |||
* [[Acanthosis nigricans]]<ref name="ThiersSahn2009">{{cite journal|last1=Thiers|first1=B. H.|last2=Sahn|first2=R. E.|last3=Callen|first3=J. P.|title=Cutaneous Manifestations of Internal Malignancy|journal=CA: A Cancer Journal for Clinicians|volume=59|issue=2|year=2009|pages=73–98|issn=0007-9235|doi=10.3322/caac.20005}}</ref> | |||
| | |||
* [[Gastric adenocarcinoma]], [[endometrial cancer]]. | |||
* | |||
|- | |||
| | |||
* [[Necrolytic migratory erythema]]<ref name="TremblayMarcil2017">{{cite journal|last1=Tremblay|first1=Catherine|last2=Marcil|first2=Isabelle|title=Necrolytic Migratory Erythema: A Forgotten Paraneoplastic Condition|journal=Journal of Cutaneous Medicine and Surgery|volume=21|issue=6|year=2017|pages=559–561|issn=1203-4754|doi=10.1177/1203475417719051}}</ref> | |||
| | |||
* [[Glucagonoma]] | |||
* | |||
|- | |||
| | |||
* [[Sweet's syndrome]]<ref name="CohenKurzrock1987">{{cite journal|last1=Cohen|first1=Philip R.|last2=Kurzrock|first2=Razelle|title=Sweet's syndrome and malignancy|journal=The American Journal of Medicine|volume=82|issue=6|year=1987|pages=1220–1226|issn=00029343|doi=10.1016/0002-9343(87)90229-4}}</ref> | |||
| | |||
* [[Acute myeloid leukemia|Acute myelogenous leukemia]], [[Myeloproliferative disease|myeloproliferative disorders]], [[lymphoproliferative disorders]], [[myelodysplastic syndrome]], and [[carcinoma]] | |||
* | |||
|- | |||
| | |||
* [[Pyoderma gangrenosum]]<ref name="YouJu2018">{{cite journal|last1=You|first1=Hye Rin|last2=Ju|first2=Jae-Kyun|last3=Yun|first3=Sook Jung|last4=Lee|first4=Jee-Bum|last5=Kim|first5=Seong-Jin|last6=Won|first6=Young Ho|last7=Lee|first7=Seung-Chul|title=Paraneoplastic Pyoderma Gangrenosum Associated with Rectal Adenocarcinoma|journal=Annals of Dermatology|volume=30|issue=1|year=2018|pages=79|issn=1013-9087|doi=10.5021/ad.2018.30.1.79}}</ref> | |||
| | |||
* [[Rectal Adenocarcinoma]], [[myeloproliferative disorders]], [[colon cancer]] | |||
* | |||
|- | |||
|+ | |||
|- | |||
| rowspan="11" align="center" style="background:#f0f0f0;" |[[Neurological]]<ref name="PelosofGerber2010">{{cite journal|last1=Pelosof|first1=Lorraine C.|last2=Gerber|first2=David E.|title=Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment|journal=Mayo Clinic Proceedings|volume=85|issue=9|year=2010|pages=838–854|issn=00256196|doi=10.4065/mcp.2010.0099}}</ref> | |||
| | |||
* [[Paraneoplastic cerebellar degeneration]]<ref name="AbdulazizYu2018">{{cite journal|last1=Abdulaziz|first1=Ammar Taha Abdullah|last2=Yu|first2=Xiao Qing|last3=Zhang|first3=Le|last4=Jiang|first4=Xin Yue|last5=Zhou|first5=Dong|last6=Li|first6=Jin Mei|title=Paraneoplastic cerebellar degeneration associated with cerebellar hypermetabolism|journal=Medicine|volume=97|issue=24|year=2018|pages=e10717|issn=0025-7974|doi=10.1097/MD.0000000000010717}}</ref> | |||
| | |||
* [[Breast cancer|Breast]] and [[gynecological malignancies]] | |||
* | |||
|- | |||
| | |||
* [[Encephalomyelitis]]<ref name="Graus2001">{{cite journal|last1=Graus|first1=F.|title=Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients|journal=Brain|volume=124|issue=6|year=2001|pages=1138–1148|issn=14602156|doi=10.1093/brain/124.6.1138}}</ref> | |||
| | |||
* [[Bronchial cancer]] (typically [[small cell lung carcinoma]]) | |||
* | |||
|- | |||
| | |||
* [[Limbic encephalitis]]<ref name="ShenXu2018">{{cite journal|last1=Shen|first1=Kaini|last2=Xu|first2=Yan|last3=Guan|first3=Hongzhi|last4=Zhong|first4=Wei|last5=Chen|first5=Minjiang|last6=Zhao|first6=Jing|last7=Li|first7=Longyun|last8=Wang|first8=Mengzhao|title=Paraneoplastic limbic encephalitis associated with lung cancer|journal=Scientific Reports|volume=8|issue=1|year=2018|issn=2045-2322|doi=10.1038/s41598-018-25294-y}}</ref> | |||
| | |||
* [[Lung cancer]] | |||
* | |||
|- | |||
| | |||
* [[Encephalitis|Brainstem encephalitis]]<ref name="Blaes2013">{{cite journal|last1=Blaes|first1=Franz|title=Paraneoplastic Brain Stem Encephalitis|journal=Current Treatment Options in Neurology|volume=15|issue=2|year=2013|pages=201–209|issn=1092-8480|doi=10.1007/s11940-013-0221-1}}</ref><ref name="PelosofGerber2010">{{cite journal|last1=Pelosof|first1=Lorraine C.|last2=Gerber|first2=David E.|title=Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment|journal=Mayo Clinic Proceedings|volume=85|issue=9|year=2010|pages=838–854|issn=00256196|doi=10.4065/mcp.2010.0099}}</ref> | |||
| | |||
* [[Lung cancer]], [[testicular cancer]], [[neuroendocrine]] [[tumors]] | |||
* | |||
|- | |||
| | |||
* [[Opsoclonus]] (involving eye movement)<ref name="Blaes2013">{{cite journal|last1=Blaes|first1=Franz|title=Paraneoplastic Brain Stem Encephalitis|journal=Current Treatment Options in Neurology|volume=15|issue=2|year=2013|pages=201–209|issn=1092-8480|doi=10.1007/s11940-013-0221-1}}</ref> | |||
| | |||
* [[Neuroblastoma]], [[small cell lung cancer]] and [[gynecological]] [[tumors]] | |||
* | |||
|- | |||
| | |||
* [[Encephalitis]] | |||
| | |||
* [[Teratoma]] | |||
|- | |||
| | |||
* [[Polymyositis]] | |||
| | |||
* [[Squamous cell lung cancer]], [[breast cancer]]<ref name="GabrilovichRaza2006">{{cite journal|last1=Gabrilovich|first1=Mikhail|last2=Raza|first2=Mohammad|last3=Dolan|first3=Stephen|last4=Raza|first4=Tasleem|title=Paraneoplastic Polymyositis Associated With Squamous Cell Carcinoma of the Lung|journal=Chest|volume=129|issue=6|year=2006|pages=1721–1723|issn=00123692|doi=10.1378/chest.129.6.1721}}</ref> | |||
|- | |||
| | |||
* [[Autonomic neuropathy]]<ref name="urlParaneoplastic autonomic neuropathy: a case report | GM">{{cite web |url=https://www.gmjournal.co.uk/paraneoplastic-autonomic-neuropathy-a-case-report |title=Paraneoplastic autonomic neuropathy: a case report | GM |format= |work= |accessdate=}}</ref> | |||
| | |||
* [[Carcinomas]],[[small cell lung cancer]], [[thymoma]] | |||
|- | |||
| | |||
* [[Lambert-Eaton myasthenic syndrome]] ([[LEMS]]) | |||
| | |||
* [[Small cell lung cancer|Small-cell lung cancer]], [[prostate cancer]], [[lymphomas]], [[adenocarcinomas]] | |||
|- | |||
| | |||
* [[Myasthenia gravis]] | |||
| | |||
* [[Thymoma]] | |||
|- | |||
| | |||
* Subacute (peripheral) [[sensory neuropathy]] | |||
| | |||
* [[Small cell lung cancer]], [[breast cancer]], [[sarcomas]], [[Hodgkin lymphoma]], and [[ovarian cancer]] | |||
|- | |||
| rowspan="4" align="center" style="background:#f0f0f0;" |[[Hematological]]<ref name="PelosofGerber2010">{{cite journal|last1=Pelosof|first1=Lorraine C.|last2=Gerber|first2=David E.|title=Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment|journal=Mayo Clinic Proceedings|volume=85|issue=9|year=2010|pages=838–854|issn=00256196|doi=10.4065/mcp.2010.0099}}</ref> | |||
| | |||
* [[Granulocytosis]]<ref name="AscensaoOken1987">{{cite journal|last1=Ascensao|first1=Joad L.|last2=Oken|first2=Martin M.|last3=Ewing|first3=Stephen L.|last4=Goldberg|first4=Robert J.|last5=Kaplan|first5=Manuel E.|title=Leukocytosis and large cell lung cancer. A frequent association|journal=Cancer|volume=60|issue=4|year=1987|pages=903–905|issn=0008-543X|doi=10.1002/1097-0142(19870815)60:4<903::AID-CNCR2820600431>3.0.CO;2-6}}</ref><ref name="AhnPark2005">{{cite journal|last1=Ahn|first1=Heui June|last2=Park|first2=Yeon Hee|last3=Chang|first3=Yoon Hwan|last4=Park|first4=Sun Hoo|last5=Kim|first5=Min-Suk|last6=Ryoo|first6=Baek Yeol|last7=Yang|first7=Sung Hyun|title=A Case of Uterine Cervical Cancer Presenting with Granulocytosis|journal=The Korean Journal of Internal Medicine|volume=20|issue=3|year=2005|pages=247|issn=1226-3303|doi=10.3904/kjim.2005.20.3.247}}</ref> | |||
| | |||
* [[Lung cancer]] (particularly [[large cell lung cancer]]), [[Gastrointestinal cancer|gastrointestinal]], [[Brain cancer|brain]], [[Breast cancer|breast]], [[Renal cancer|renal]], and [[gynecologic cancers]] | |||
|- | |||
| | |||
* [[Thrombocytosis]]<ref name="StoneNick2012">{{cite journal|last1=Stone|first1=Rebecca L.|last2=Nick|first2=Alpa M.|last3=McNeish|first3=Iain A.|last4=Balkwill|first4=Frances|last5=Han|first5=Hee Dong|last6=Bottsford-Miller|first6=Justin|last7=Rupaimoole|first7=Rajesha|last8=Armaiz-Pena|first8=Guillermo N.|last9=Pecot|first9=Chad V.|last10=Coward|first10=Jermaine|last11=Deavers|first11=Michael T.|last12=Vasquez|first12=Hernan G.|last13=Urbauer|first13=Diana|last14=Landen|first14=Charles N.|last15=Hu|first15=Wei|last16=Gershenson|first16=Hannah|last17=Matsuo|first17=Koji|last18=Shahzad|first18=Mian M.K.|last19=King|first19=Erin R.|last20=Tekedereli|first20=Ibrahim|last21=Ozpolat|first21=Bulent|last22=Ahn|first22=Edward H.|last23=Bond|first23=Virginia K.|last24=Wang|first24=Rui|last25=Drew|first25=Angela F.|last26=Gushiken|first26=Francisca|last27=Lamkin|first27=Donald|last28=Collins|first28=Katherine|last29=DeGeest|first29=Koen|last30=Lutgendorf|first30=Susan K.|last31=Chiu|first31=Wah|last32=Lopez-Berestein|first32=Gabriel|last33=Afshar-Kharghan|first33=Vahid|last34=Sood|first34=Anil K.|title=Paraneoplastic Thrombocytosis in Ovarian Cancer|journal=New England Journal of Medicine|volume=366|issue=7|year=2012|pages=610–618|issn=0028-4793|doi=10.1056/NEJMoa1110352}}</ref> | |||
| | |||
* [[Ovarian cancer]] | |||
|- | |||
| | |||
* [[Pure red cell aplasia]]<ref name="RosuCohen2011">{{cite journal|last1=Rosu|first1=Cristian|last2=Cohen|first2=Sandra|last3=Meunier|first3=Caroline|last4=Ouellette|first4=Denise|last5=Beauchamp|first5=Gilles|last6=Rakovich|first6=George|title=Pure red cell aplasia and associated thymoma|journal=Clinics and Practice|volume=1|issue=1|year=2011|pages=1|issn=2039-7283|doi=10.4081/cp.2011.e1}}</ref> | |||
| | |||
* [[Thymoma]], [[lymphoma]], [[leukemia]] | |||
|- | |||
| | |||
* [[Eosinophilia]]<ref name="PelosofGerber2010">{{cite journal|last1=Pelosof|first1=Lorraine C.|last2=Gerber|first2=David E.|title=Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment|journal=Mayo Clinic Proceedings|volume=85|issue=9|year=2010|pages=838–854|issn=00256196|doi=10.4065/mcp.2010.0099}}</ref> | |||
| | |||
* [[Lymphomas]], [[leukemias]], [[lung]], [[Gastrointestinal tumor|gastrointestinal]], and [[Genital cancer|gynecologic]] [[tumors]] | |||
|- | |||
| align="center" style="background:#f0f0f0;" |Others | |||
| | |||
* [[Membranous glomerulonephritis]]<ref name="LeeaphornKue-A-Pai2014">{{cite journal|last1=Leeaphorn|first1=Napat|last2=Kue-A-Pai|first2=Pogsathorn|last3=Thamcharoen|first3=Natanong|last4=Ungprasert|first4=Patompong|last5=Stokes|first5=Michael B.|last6=Knight|first6=Eric L.|title=Prevalence of Cancer in Membranous Nephropathy: A Systematic Review and Meta-Analysis of Observational Studies|journal=American Journal of Nephrology|volume=40|issue=1|year=2014|pages=29–35|issn=1421-9670|doi=10.1159/000364782}}</ref> | |||
| | |||
* [[Lung cancer]], [[prostate cancer]], and [[Hematologic malignancy|hematologic malignancies]] | |||
|- | |||
|} | |||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | |||
|+ | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|- | |||
|} | |||
{| border="3" | {| border="3" | ||
|+ | |+ | ||
Revision as of 22:30, 6 December 2019
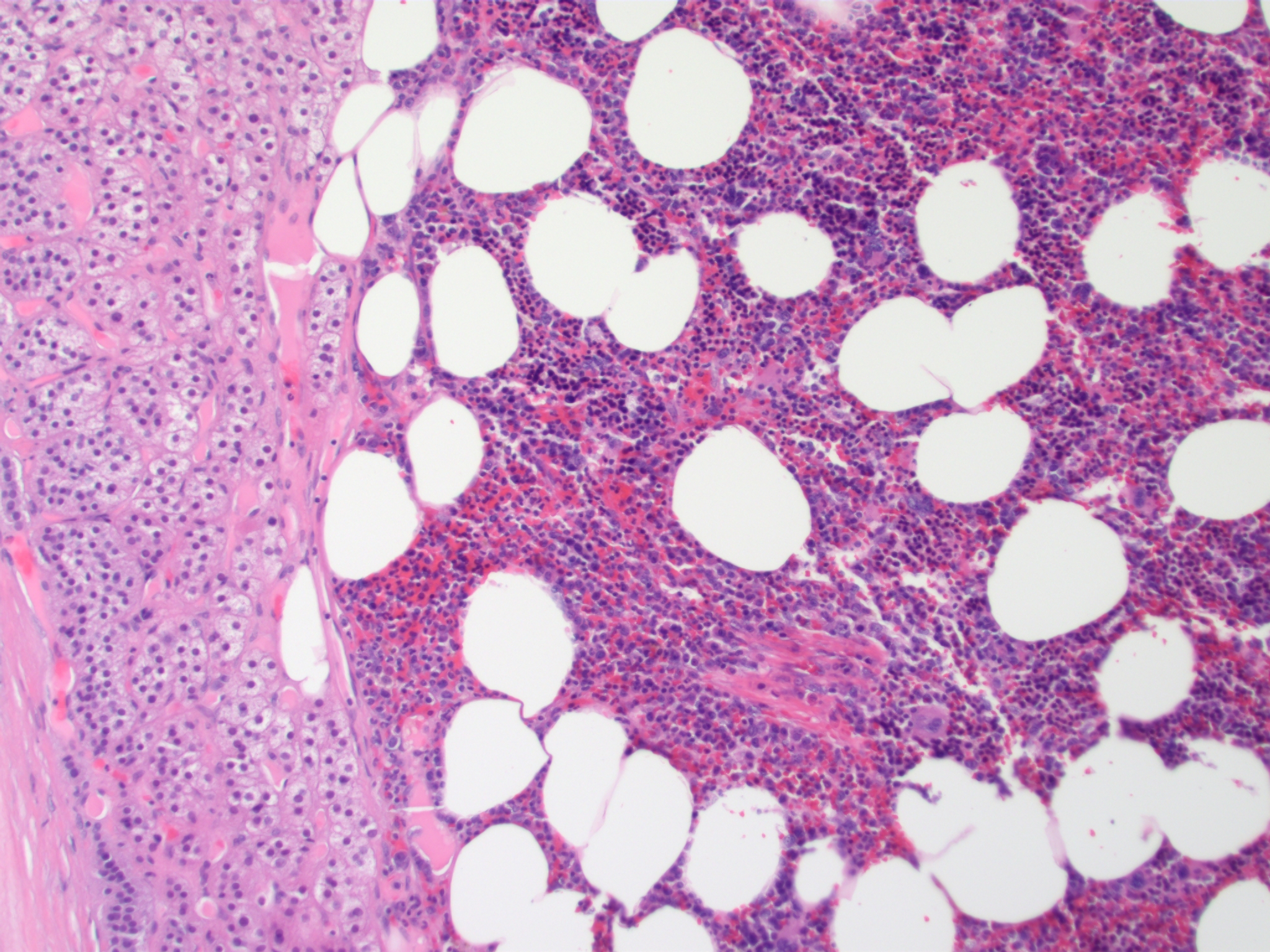
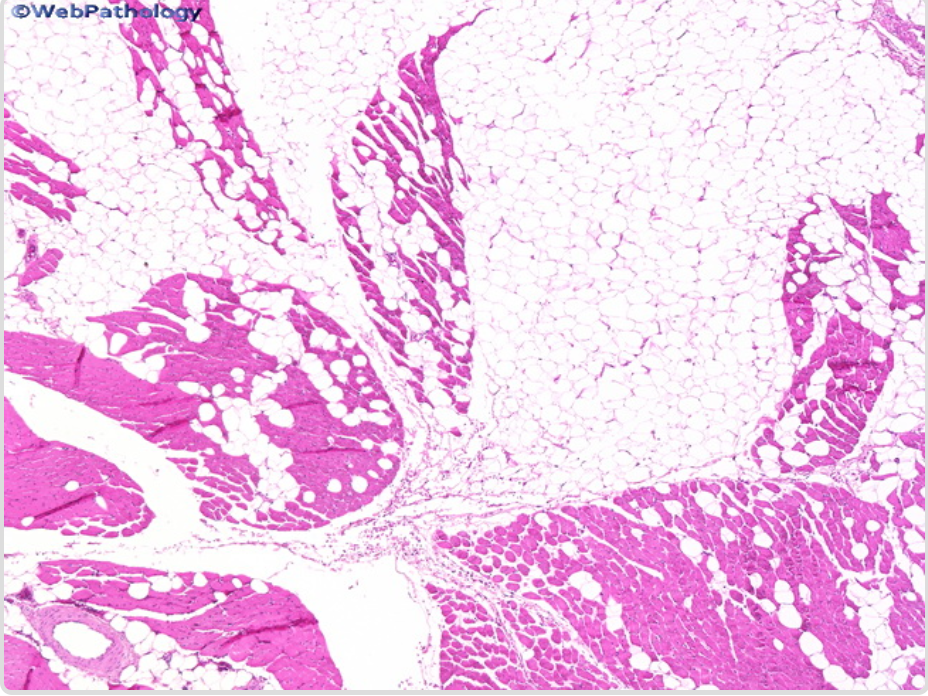
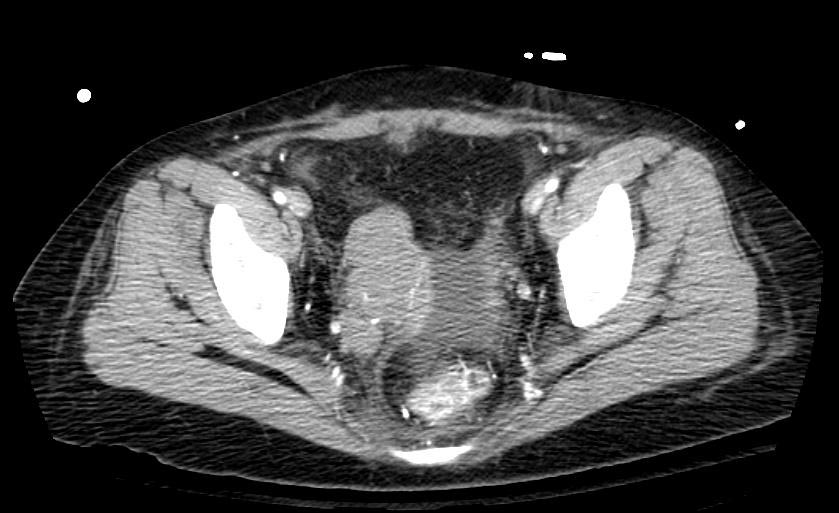
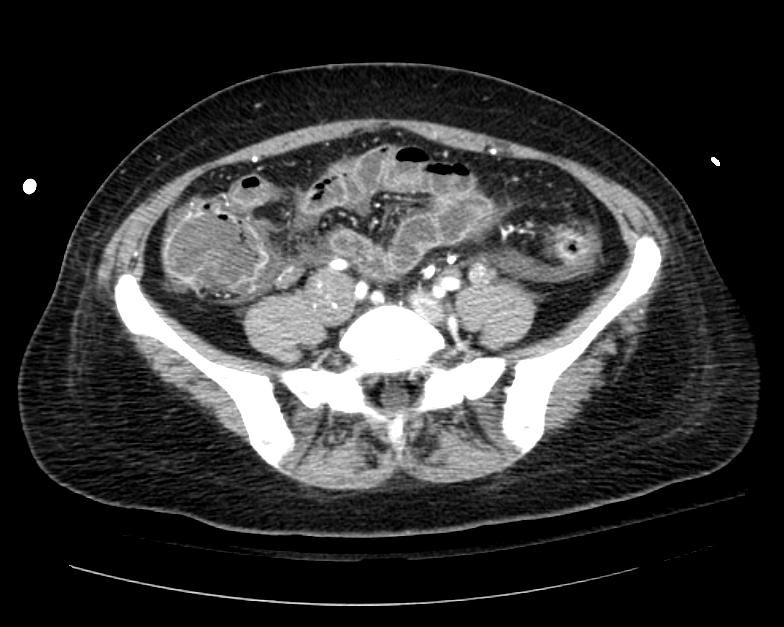
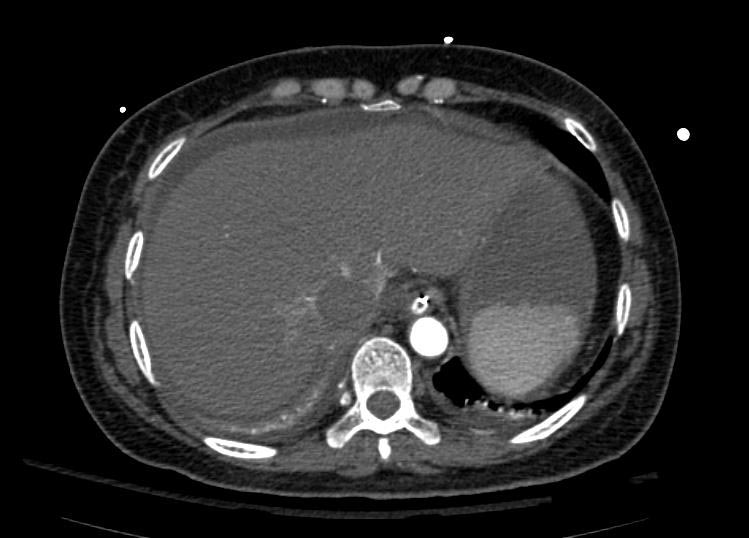
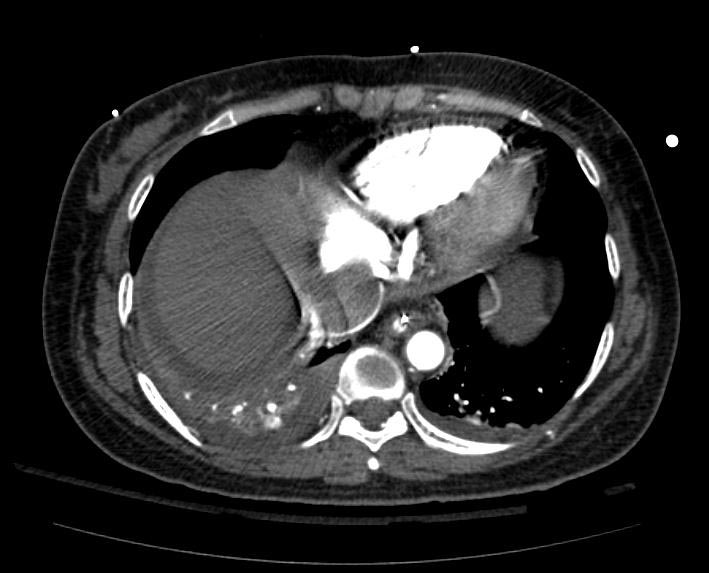
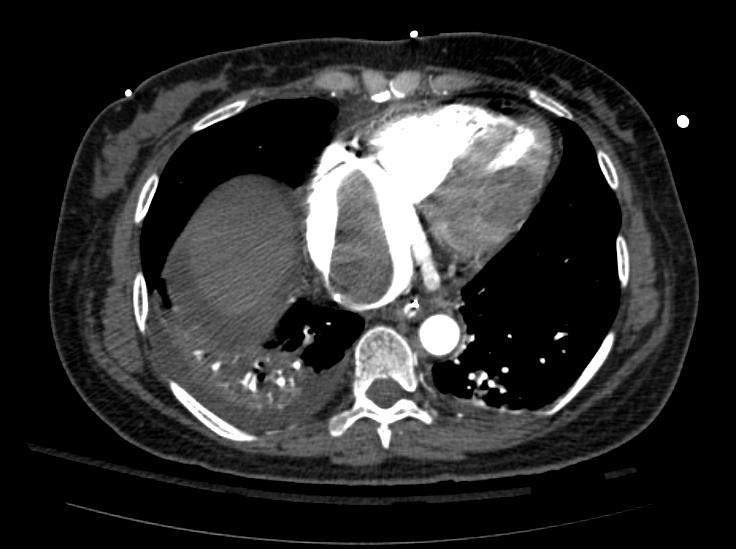
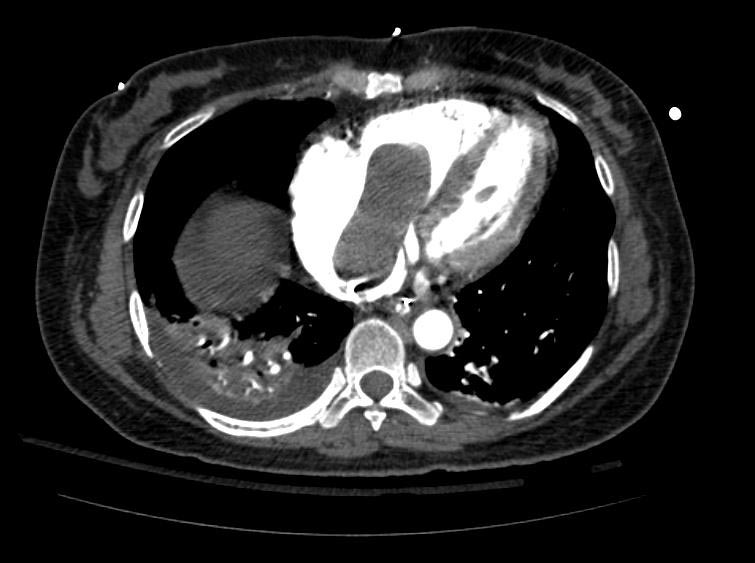
Example #1
The patient presented with S.O.B. one year after hysterectomy for a leiomyomatous uterus.
- ↑ Stewart, Andrew F. (2005). "Hypercalcemia Associated with Cancer". New England Journal of Medicine. 352 (4): 373–379. doi:10.1056/NEJMcp042806. ISSN 0028-4793.
- ↑ Raftopoulos, Harry (2007). "Diagnosis and management of hyponatremia in cancer patients". Supportive Care in Cancer. 15 (12): 1341–1347. doi:10.1007/s00520-007-0309-9. ISSN 0941-4355.
- ↑ Barbosa, Sandrine Laboureau-Soares; Rodien, Patrice; Leboulleux, Sophie; Niccoli-Sire, Patricia; Kraimps, Jean-Louis; Caron, Philippe; Archambeaud-Mouveroux, Françoise; Conte-Devolx, Bernard; Rohmer, Vincent (2005). "Ectopic Adrenocorticotropic Hormone-Syndrome in Medullary Carcinoma of the Thyroid: A Retrospective Analysis and Review of the Literature". Thyroid. 15 (6): 618–623. doi:10.1089/thy.2005.15.618. ISSN 1050-7256.
- ↑ Florenzano, Pablo; Gafni, Rachel I.; Collins, Michael T. (2017). "Tumor-induced osteomalacia". Bone Reports. 7: 90–97. doi:10.1016/j.bonr.2017.09.002. ISSN 2352-1872.
- ↑ Nauck, Michael A.; Reinecke, Manfred; Perren, Aurel; Frystyk, Jan; Berishvili, Giorgi; Zwimpfer, Cornelia; Figge, Anja M.; Flyvbjerg, Allan; Lankisch, Paul G.; Blum, Werner F.; Klöppel, Günter; Schmiegel, Wolff; Zapf, Jürgen (2007). "Hypoglycemia due to Paraneoplastic Secretion of Insulin-Like Growth Factor-I in a Patient with Metastasizing Large-Cell Carcinoma of the Lung". The Journal of Clinical Endocrinology & Metabolism. 92 (5): 1600–1605. doi:10.1210/jc.2006-2573. ISSN 0021-972X.
- ↑ 6.0 6.1 Thiers, B. H.; Sahn, R. E.; Callen, J. P. (2009). "Cutaneous Manifestations of Internal Malignancy". CA: A Cancer Journal for Clinicians. 59 (2): 73–98. doi:10.3322/caac.20005. ISSN 0007-9235.
- ↑ Gaduputi, Vinaya; Chandrala, Chaitanya; Tariq, Hassan; Kanneganti, Kalyan (2014). "Sign of Leser-Trélat Associated with Esophageal Squamous Cell Cancer". Case Reports in Oncological Medicine. 2014: 1–3. doi:10.1155/2014/825929. ISSN 2090-6706.
- ↑ Tremblay, Catherine; Marcil, Isabelle (2017). "Necrolytic Migratory Erythema: A Forgotten Paraneoplastic Condition". Journal of Cutaneous Medicine and Surgery. 21 (6): 559–561. doi:10.1177/1203475417719051. ISSN 1203-4754.
- ↑ Cohen, Philip R.; Kurzrock, Razelle (1987). "Sweet's syndrome and malignancy". The American Journal of Medicine. 82 (6): 1220–1226. doi:10.1016/0002-9343(87)90229-4. ISSN 0002-9343.
- ↑ You, Hye Rin; Ju, Jae-Kyun; Yun, Sook Jung; Lee, Jee-Bum; Kim, Seong-Jin; Won, Young Ho; Lee, Seung-Chul (2018). "Paraneoplastic Pyoderma Gangrenosum Associated with Rectal Adenocarcinoma". Annals of Dermatology. 30 (1): 79. doi:10.5021/ad.2018.30.1.79. ISSN 1013-9087.
- ↑ 11.0 11.1 11.2 11.3 Pelosof, Lorraine C.; Gerber, David E. (2010). "Paraneoplastic Syndromes: An Approach to Diagnosis and Treatment". Mayo Clinic Proceedings. 85 (9): 838–854. doi:10.4065/mcp.2010.0099. ISSN 0025-6196.
- ↑ Abdulaziz, Ammar Taha Abdullah; Yu, Xiao Qing; Zhang, Le; Jiang, Xin Yue; Zhou, Dong; Li, Jin Mei (2018). "Paraneoplastic cerebellar degeneration associated with cerebellar hypermetabolism". Medicine. 97 (24): e10717. doi:10.1097/MD.0000000000010717. ISSN 0025-7974.
- ↑ Graus, F. (2001). "Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients". Brain. 124 (6): 1138–1148. doi:10.1093/brain/124.6.1138. ISSN 1460-2156.
- ↑ Shen, Kaini; Xu, Yan; Guan, Hongzhi; Zhong, Wei; Chen, Minjiang; Zhao, Jing; Li, Longyun; Wang, Mengzhao (2018). "Paraneoplastic limbic encephalitis associated with lung cancer". Scientific Reports. 8 (1). doi:10.1038/s41598-018-25294-y. ISSN 2045-2322.
- ↑ 15.0 15.1 Blaes, Franz (2013). "Paraneoplastic Brain Stem Encephalitis". Current Treatment Options in Neurology. 15 (2): 201–209. doi:10.1007/s11940-013-0221-1. ISSN 1092-8480.
- ↑ Gabrilovich, Mikhail; Raza, Mohammad; Dolan, Stephen; Raza, Tasleem (2006). "Paraneoplastic Polymyositis Associated With Squamous Cell Carcinoma of the Lung". Chest. 129 (6): 1721–1723. doi:10.1378/chest.129.6.1721. ISSN 0012-3692.
- ↑ "Paraneoplastic autonomic neuropathy: a case report | GM".
- ↑ Ascensao, Joad L.; Oken, Martin M.; Ewing, Stephen L.; Goldberg, Robert J.; Kaplan, Manuel E. (1987). "Leukocytosis and large cell lung cancer. A frequent association". Cancer. 60 (4): 903–905. doi:10.1002/1097-0142(19870815)60:4<903::AID-CNCR2820600431>3.0.CO;2-6. ISSN 0008-543X.
- ↑ Ahn, Heui June; Park, Yeon Hee; Chang, Yoon Hwan; Park, Sun Hoo; Kim, Min-Suk; Ryoo, Baek Yeol; Yang, Sung Hyun (2005). "A Case of Uterine Cervical Cancer Presenting with Granulocytosis". The Korean Journal of Internal Medicine. 20 (3): 247. doi:10.3904/kjim.2005.20.3.247. ISSN 1226-3303.
- ↑ Stone, Rebecca L.; Nick, Alpa M.; McNeish, Iain A.; Balkwill, Frances; Han, Hee Dong; Bottsford-Miller, Justin; Rupaimoole, Rajesha; Armaiz-Pena, Guillermo N.; Pecot, Chad V.; Coward, Jermaine; Deavers, Michael T.; Vasquez, Hernan G.; Urbauer, Diana; Landen, Charles N.; Hu, Wei; Gershenson, Hannah; Matsuo, Koji; Shahzad, Mian M.K.; King, Erin R.; Tekedereli, Ibrahim; Ozpolat, Bulent; Ahn, Edward H.; Bond, Virginia K.; Wang, Rui; Drew, Angela F.; Gushiken, Francisca; Lamkin, Donald; Collins, Katherine; DeGeest, Koen; Lutgendorf, Susan K.; Chiu, Wah; Lopez-Berestein, Gabriel; Afshar-Kharghan, Vahid; Sood, Anil K. (2012). "Paraneoplastic Thrombocytosis in Ovarian Cancer". New England Journal of Medicine. 366 (7): 610–618. doi:10.1056/NEJMoa1110352. ISSN 0028-4793.
- ↑ Rosu, Cristian; Cohen, Sandra; Meunier, Caroline; Ouellette, Denise; Beauchamp, Gilles; Rakovich, George (2011). "Pure red cell aplasia and associated thymoma". Clinics and Practice. 1 (1): 1. doi:10.4081/cp.2011.e1. ISSN 2039-7283.
- ↑ Leeaphorn, Napat; Kue-A-Pai, Pogsathorn; Thamcharoen, Natanong; Ungprasert, Patompong; Stokes, Michael B.; Knight, Eric L. (2014). "Prevalence of Cancer in Membranous Nephropathy: A Systematic Review and Meta-Analysis of Observational Studies". American Journal of Nephrology. 40 (1): 29–35. doi:10.1159/000364782. ISSN 1421-9670.