Sandbox:Prince: Difference between revisions
Prince Djan (talk | contribs) No edit summary |
Prince Djan (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
{{Infobox_Disease | |||
| Name = Peritonsillar abscess | |||
| Image = | |||
| Caption = | |||
| DiseasesDB = 11141 | |||
| ICD10 = {{ICD10|J|36||j|30}} | |||
| ICD9 = {{ICD9|475}} | |||
| ICDO = | |||
| OMIM = | |||
| MedlinePlus = | |||
| eMedicineSubj = emerg | |||
| eMedicineTopic = 417 | |||
| MeshID = | |||
}} | |||
__Notoc__ | |||
{{SI}} | |||
{{CMG}}; {{KS}} {{PTD}} | |||
{{SK}} PTA, tonsillar abscess, intratonsillar abscess | |||
==Overview== | |||
Peritonsillar abscess (PTA), also commonly referred to as [[quinsy]], is defined as a collection of [[pus]] located between the tonsillar [[capsule]] and the [[pharyngeal]] [[Constrictor pharyngis medius|constrictor]] muscles. | |||
It is the most common deep tissue infection of the neck.<ref name="pmid18246890">{{cite journal| author=Galioto NJ| title=Peritonsillar abscess. | journal=Am Fam Physician | year= 2008 | volume= 77 | issue= 2 | pages= 199-202 | pmid=18246890 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18246890 }} </ref> | |||
Historically, it has been thought of as a complication of [[acute]] [[tonsillitis]]. However, recent studies have proposed additional [[hypothesis]] surrounding its [[pathogenesis]] making the understanding of the disease a medical dilemma.<ref name="pmid23612569">{{cite journal| author=Powell EL, Powell J, Samuel JR, Wilson JA| title=A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation. | journal=J Antimicrob Chemother | year= 2013 | volume= 68 | issue= 9 | pages= 1941-50 | pmid=23612569 | doi=10.1093/jac/dkt128 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23612569 }} </ref> | |||
==Historical perspective== | |||
The outline below shows the historical perspective of peritonsillar abscess.<ref name="pmid8302122">{{cite journal| author=Passy V| title=Pathogenesis of peritonsillar abscess. | journal=Laryngoscope | year= 1994 | volume= 104 | issue= 2 | pages= 185-90 | pmid=8302122 | doi=10.1288/00005537-199402000-00011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8302122 }} </ref> | |||
*In second and third century BC, Celcius was the first to document in literature the treatment and [[pathogenesis]] of tonsillar [[pathology]]. | |||
*In 1700s peritonsillar abscess was first described. | |||
*In the 1930s and 1940s prior to the advent of antibiotics, surgical management was the most common treatment option for peritonsillar abscess. Interval [[tonsillectomy]] was mostly done after symptom resolution. | |||
*By 1947, Chaud [[tonsillectomy]] or immediate surgical [[tonsillectomy]] became the treatment option. | |||
==Classification== | |||
On the basis of computed tomographical findings, peritonsillar abscess may be classified into 3 broad categories based on the following: | |||
1. '''Shape of the abscess''' | |||
On the basis of shape it may be classified as:<ref name="pmid26527518">{{cite journal| author=Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H et al.| title=Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy. | journal=Auris Nasus Larynx | year= 2016 | volume= 43 | issue= 2 | pages= 182-6 | pmid=26527518 | doi=10.1016/j.anl.2015.09.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26527518 }} </ref> | |||
*[[Oval]] type or | |||
*Cap type | |||
2. '''Location of the abscess''' | |||
On the basis of abscess location it may be differentiated into the following:<ref name="pmid26527518">{{cite journal| author=Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H et al.| title=Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy. | journal=Auris Nasus Larynx | year= 2016 | volume= 43 | issue= 2 | pages= 182-6 | pmid=26527518 | doi=10.1016/j.anl.2015.09.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26527518 }} </ref> | |||
*[[Superior]] or | |||
*Inferior | |||
3. '''Shape and location''' | |||
On the basis of shaped and location it may be classified as:<ref name="pmid26527518">{{cite journal| author=Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H et al.| title=Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy. | journal=Auris Nasus Larynx | year= 2016 | volume= 43 | issue= 2 | pages= 182-6 | pmid=26527518 | doi=10.1016/j.anl.2015.09.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26527518 }} </ref> | |||
*[[Superior]] [[Oval]] type | |||
*[[Superior]] Cap type | |||
*Inferior [[Oval]] type and | |||
*Inferior Cap type | |||
==Pathophysiology== | |||
===Anatomy=== | |||
A good understanding of the [[tonsil]] and its surrounding space is important in the [[pathogenesis]] of peritonsillar abscess. | |||
The [[palatine tonsils]] are found in an anatomical structure called [[tonsillar fossa]]. This [[fossa]] is bounded anteriorly by palatoglossal muscle, posteriorly by palatopharyngeal muscle, laterally by a [[fibrous]] [[capsule]] and tonsillar crypts [[medially]]. Contents of the tonsillar crypts are expelled by [[contraction]] of the tonsillopharyngeus muscle.<ref name=abd>L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286</ref> The [[tonsils]] form during the last months of [[pregnancy]] and becomes fully formed by 6 to 7 years of age. It then undergoes involution until small size remains in older population. | |||
Located within the soft palate is the supratonsillar space occupied by series of 20 to 25 [[salivary glands]] described as Weber's glands. The [[ducts]] of these [[glands]] form a common [[duct]] which opens onto the [[posterior]] surface of the [[tonsil]] after passing through the tonsillar [[capsule]]. It is proposed that the secretions from these [[glands]] play a rule in food [[digestion]]. | |||
Peritonsillar abscesses form in the area between the [[Palatine tonsils|palatine tonsil]] and its [[capsule]]. | |||
===Pathogenesis=== | |||
The [[pathogenesis]] of peritonsillar abscess is still not well-understood.<ref name="pmid23612569">{{cite journal| author=Powell EL, Powell J, Samuel JR, Wilson JA| title=A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation. | journal=J Antimicrob Chemother | year= 2013 | volume= 68 | issue= 9 | pages= 1941-50 | pmid=23612569 | doi=10.1093/jac/dkt128 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23612569 }} </ref> There are two proposed theories believed to be involved in the pathogensis of peritonsillar abscess formation.<ref name=abd>L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286</ref><ref name="pmid8302122">{{cite journal| author=Passy V| title=Pathogenesis of peritonsillar abscess. | journal=Laryngoscope | year= 1994 | volume= 104 | issue= 2 | pages= 185-90 | pmid=8302122 | doi=10.1288/00005537-199402000-00011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8302122 }} </ref><ref name="pmid25865201">{{cite journal| author=Blair AB, Booth R, Baugh R| title=A unifying theory of tonsillitis, intratonsillar abscess and peritonsillar abscess. | journal=Am J Otolaryngol | year= 2015 | volume= 36 | issue= 4 | pages= 517-20 | pmid=25865201 | doi=10.1016/j.amjoto.2015.03.002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25865201 }} </ref><ref name="pmid16643771">{{cite journal| author=Herzon FS, Martin AD| title=Medical and surgical treatment of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=Curr Infect Dis Rep | year= 2006 | volume= 8 | issue= 3 | pages= 196-202 | pmid=16643771 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16643771 }} </ref> | |||
*1. It is proposed to arise from an extension of [[exudative]] [[tonsillitis]]. | |||
Some authorities believe that blockage of drainage from tonsillar crypt in [[acute]] [[tonsillitis]] results in spread of infection into the peritonsillar space. | |||
*2. Involvement of Weber's [[gland]] account for the [[abscess]] formation. Some believe that peritonsillar abscess arises from [[infectious]] process involving group of [[salivary glands]] called Weber's glands located in the supratonsillar space. | |||
[[Antigenic]] response following any disturbance arising from within the tonsillar crypt [[Mucosal|mucosa]] allows for [[lymphocytic]] interaction. This disruption in the crypt [[epithelium]] may be preceded by [[infectious]] process. [[Invasion]] and [[proliferation]] of the tonsillar crypt by [[infectious]] [[pathogens]] results in localized [[edema]] and influx of [[neutrophils]]. This is clinically seen as [[inflamed]] [[tonsil]] with or without exudation.<ref name=abd>L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286</ref> Pus accumulation within tissue behind the supratonsillar space leads to tonsillar bulging, [[uvula]] and [[palate]] deviation. | |||
==Causes== | |||
Peritonsillar abscess (PTA) usually arises as a complication of an untreated or partially treated episode of [[acute]] [[tonsillitis]]. The infection, in these cases, spreads to the [[peritonsillar]] area (peritonsillitis). This region comprises of loose [[connective tissue]] and is hence susceptible to formation of [[abscess]]. Peritonsilar abscess can also occur ''de novo''. | |||
Both [[Aerobic organism|aerobic]] and [[Anaerobic organism|anaerobic]] bacteria can be causative.<ref name="pmid18039418">{{cite journal| author=Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S| title=Changing trends in bacteriology of peritonsillar abscess. | journal=J Laryngol Otol | year= 2008 | volume= 122 | issue= 9 | pages= 928-30 | pmid=18039418 | doi=10.1017/S0022215107001144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039418 }} </ref><ref name="pmid18039418">{{cite journal| author=Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S| title=Changing trends in bacteriology of peritonsillar abscess. | journal=J Laryngol Otol | year= 2008 | volume= 122 | issue= 9 | pages= 928-30 | pmid=18039418 | doi=10.1017/S0022215107001144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039418 }} </ref> | |||
===Life-threatening causes=== | |||
Life-threatening conditions may result in death or permanent disability within 24 hours if left untreated. Peritonsillar abscess may become a life-threatening condition and must be treated as such irrespective of the cause.<ref name="pmid15573356">{{cite journal| author=Brook I| title=Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=J Oral Maxillofac Surg | year= 2004 | volume= 62 | issue= 12 | pages= 1545-50 | pmid=15573356 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15573356 }} </ref><ref name="pmid18039418">{{cite journal| author=Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S| title=Changing trends in bacteriology of peritonsillar abscess. | journal=J Laryngol Otol | year= 2008 | volume= 122 | issue= 9 | pages= 928-30 | pmid=18039418 | doi=10.1017/S0022215107001144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039418 }} </ref> | |||
===Most common cause=== | |||
The most frequent pathogen of peritonsillar abscess is [[Streptococcus pyogenes]].<ref name="pmid15573356">{{cite journal| author=Brook I| title=Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=J Oral Maxillofac Surg | year= 2004 | volume= 62 | issue= 12 | pages= 1545-50 | pmid=15573356 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15573356 }} </ref><ref name="pmid18039418">{{cite journal| author=Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S| title=Changing trends in bacteriology of peritonsillar abscess. | journal=J Laryngol Otol | year= 2008 | volume= 122 | issue= 9 | pages= 928-30 | pmid=18039418 | doi=10.1017/S0022215107001144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039418 }} </ref><ref name="pmid1875138">{{cite journal| author=Snow DG, Campbell JB, Morgan DW| title=The microbiology of peritonsillar sepsis. | journal=J Laryngol Otol | year= 1991 | volume= 105 | issue= 7 | pages= 553-5 | pmid=1875138 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1875138 }} </ref><ref name="pmid12092281">{{cite journal| author=Matsuda A, Tanaka H, Kanaya T, Kamata K, Hasegawa M| title=Peritonsillar abscess: a study of 724 cases in Japan. | journal=Ear Nose Throat J | year= 2002 | volume= 81 | issue= 6 | pages= 384-9 | pmid=12092281 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12092281 }} </ref> | |||
===Common causes=== | |||
Some common causes of peritonsillar abscess include:<ref name="pmid15573356">{{cite journal| author=Brook I| title=Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=J Oral Maxillofac Surg | year= 2004 | volume= 62 | issue= 12 | pages= 1545-50 | pmid=15573356 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15573356 }} </ref><ref name="pmid18039418">{{cite journal| author=Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S| title=Changing trends in bacteriology of peritonsillar abscess. | journal=J Laryngol Otol | year= 2008 | volume= 122 | issue= 9 | pages= 928-30 | pmid=18039418 | doi=10.1017/S0022215107001144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039418 }} </ref> | |||
*[[Fusobacterium necrophorum]] | |||
*[[Streptococcus milleri]] | |||
*[[Staphylococci]] | |||
*[[Haemophilus]] | |||
*[[Fusobacterium]] | |||
*[[Prevotella]] | |||
*''[[Acinetobacter spp|Acinetobacter]]'' [[Acinetobacter spp|spp]]. | |||
*''[[Candida albicans]]'' | |||
*[[Peptostreptococcus]] spp. | |||
*[[Pseudomonas]] spp. | |||
*[[Enterobacter]] spp. | |||
*[[Klebsiella]] | |||
===Less common causes=== | |||
Less common causes of peritonsillar abscess include:<ref name="pmid15573356">{{cite journal| author=Brook I| title=Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=J Oral Maxillofac Surg | year= 2004 | volume= 62 | issue= 12 | pages= 1545-50 | pmid=15573356 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15573356 }} </ref><ref name="pmid18039418">{{cite journal| author=Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S| title=Changing trends in bacteriology of peritonsillar abscess. | journal=J Laryngol Otol | year= 2008 | volume= 122 | issue= 9 | pages= 928-30 | pmid=18039418 | doi=10.1017/S0022215107001144 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18039418 }} </ref> | |||
* [[Porphyromonas]] | |||
==Differentiating Peritonsillar abscess from Other Diseases== | |||
{| class="wikitable" | |||
!Disease/Variable | |||
!Presentation | |||
!Causes | |||
!Physical exams findings | |||
!Age commonly affected | |||
!Imaging finding | |||
!Treatment | |||
|- | |||
|[[Peritonsillar abscess]] | |||
|Severe [[sore throat]], [[otalgia]] [[fever]], a "hot potato" or muffled voice, [[drooling]], and [[trismus]]<ref name="pmid18246890" /> | |||
|[[Streptococcus pyogenes|Aerobic and anaerobic]] | |||
[[Streptococcus pyogenes|bacteria most common is]] | |||
[[Streptococcus pyogenes|Streptococcus]] | |||
[[Streptococcus pyogenes|pyogenes]].<ref name="pmid15573356" /><ref name="pmid18039418" /><ref name="pmid1875138" /><ref name="pmid12092281" /> | |||
|[[Contralateral]] deflection of the uvula, | |||
the [[tonsil]] is displaced [[inferiorly]] and [[medially]], tender [[submandibular]] and [[anterior]] [[cervical lymph nodes|cervical lymph nodes,]] [[Tonsillar abscess|tonsillar]] [[hypertrophy]] with likely peritonsillar [[edema]]. | |||
|The highest occurrence is in adults between 20 to 40 years of age.<ref name="pmid18246890" /> | |||
|On ultrasound peritonsillar abscess appears as focal irregularly marginated hypoechoic area.<ref name="pmid15635144" /><ref name="pmid1642863" /><ref name="pmid26637999" /><ref name="pmid10435129" /><ref name="pmid15635144" /><ref name="pmid1642863" /> | |||
|[[Ampicillin-sulbactam|Ampicillin-sulbactam,]] [[Clindamycin]], [[Vancomycin]] or [[Linezolid]] | |||
|- | |||
|[[Croup]] | |||
|Has [[cough]] and [[stridor]] but no [[drooling]]. Others are [[Hoarseness]], [[Difficulty breathing]], symptoms of the [[common cold]], [[Runny nose]], [[Fever]] | |||
|[[Parainfluenza virus]] | |||
|Suprasternal and [[intercostal]] [[Indrawing|indrawing,]]<ref name="pmid19445760" /> Inspiratory [[stridor]]<ref name="Cherry2008" />, expiratory [[wheezing]],<ref name="Cherry2008" /> [[Sternal]] wall retractions<ref name="pmid194457602" /> | |||
|Mainly 6 months and 3 years old | |||
rarely, adolescents and adults<ref name="pmid8769531" /> | |||
|[[Steeple sign]] on neck X-ray | |||
|[[Dexamethasone]] and nebulised [[epenephrine|epinephrine]] | |||
|- | |||
|[[Epiglottitis]] | |||
|Has [[stridor]] and [[drooling]] [[Difficulty breathing|but no cough. Other symptoms include difficulty breathing]], [[Difficulty swallowing|fever, chills, difficulty swallowing]], [[hoarseness]] of voice | |||
|[[Hemolysis|H. influenza type b,]] | |||
[[Hemolysis|beta-hemolytic]] [[streptococci]], ''[[Staphylococcus aureus]],'' | |||
[[fungi]] and [[viruses]]. | |||
|[[Cyanosis]], [[Cervical]] [[lymphadenopathy]], Inflammed [[epiglottis]] | |||
|Used to be mostly found in | |||
pediatric age group between 3 to 5 years, | |||
however, recent trend favors adults | |||
as most commonly affected individuals<ref name="pmid270310102" /> | |||
with a mean age of 44.94 years | |||
|[[Thumbprint sign]] on neck x-ray | |||
|Airway maintenance, p[[Parenteral|arenteral]] [[Cefotaxime]] or [[Ceftriaxone]] in combination with [[Vancomycin]]. Adjuvant therapy includes [[corticosteroids]] and [[racemic]] [[Epinephrine]].<ref name="pmid15983574" /><ref name="pmid12557859" /> | |||
|- | |||
|[[Pharyngitis]] | |||
|[[Sore throat]], pain on swallowing, [[fever]], [[headache]], [[Abdominal pain|abdominal]] pain, [[nausea]] and [[vomiting]] | |||
|[[Group A beta-hemolytic streptococci|Group A beta-hemolytic]] | |||
[[Group A beta-hemolytic streptococci|streptococcus]]. | |||
|Inflammed [[pharynx]] with or without [[exudate]] | |||
|Mostly in children and young adults, | |||
with 50% of cases identified | |||
between the ages of 5 to 24 years.<ref name=":0" /> | |||
|_ | |||
|[[Antimicrobial]] therapy mainly [[penicillin]]-based and [[analgesics]]. | |||
|- | |||
|[[Tonsilitis]] | |||
|[[Sore throat]], pain on swallowing, [[fever]], [[headache]], [[cough]] | |||
|Most common cause is | |||
viral including [[adenovirus]], | |||
[[rhinovirus]], [[influenza]], | |||
[[coronavirus]], and | |||
[[respiratory syncytial virus]]. | |||
Second most common | |||
causes are bacterial; | |||
''[[Group A streptococcal infection|Group A streptococcal]]'' | |||
''[[Group A streptococcal infection|bacteria]]'',<ref name="pmid3601520" /> | |||
|[[Fever]], especially 100°F or higher.<ref name="Tonsillitis" /><ref name="urlTonsillitis - NHS Choices" />[[Erythema]], [[edema]] and [[Exudate]] of the [[tonsils]].<ref name="pmid25587367" /> cervical [[lymphadenopathy]], [[Dysphonia]].<ref name="urlTonsillitis - Symptoms - NHS Choices" /> | |||
|Primarily affects children | |||
between 5 and 15 years old.<ref name="Oroface" /> | |||
|Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.<ref name="pmid26527518" /><ref name="pmid25946659" /><ref name="pmid25945805" /> | |||
|[[Antimicrobial]] therapy mainly [[penicillin]]-based and [[analgesics]] with [[tonsilectomy]] in selected cases. | |||
|- | |||
|[[Retropharyngeal abscess]] | |||
|[[Neck pain]], [[stiff neck]], [[torticollis]] | |||
[[fever]], [[malaise]], [[stridor]], and barking [[cough]] | |||
|Polymicrobial infection. | |||
Mostly; [[Streptococcus pyogenes|Streptococcus]] | |||
[[Streptococcus pyogenes|pyogenes]], [[Staphylococcus aureus]] and respiratory anaerobes (example; Fusobacteria, [[Prevotella species|Prevotella]], | |||
and Veillonella species)<ref name="pmid23520072" /><ref name="pmid22481424" /><ref name="pmid18948832" /><ref name="pmid15573356" /><ref name="pmid18427007" /><ref name="pmid2235179" /> | |||
|Child may be unable to open the mouth widely. May have enlarged | |||
[[cervical]] [[lymph nodes]] and neck mass. | |||
|Mostly between 2-4 years, but can occur in other age groups.<ref name="pmid12777558" /><ref name="pmid1876473" /> | |||
|On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen<ref name="pmid15667676" /><ref name="pmid12761699" /> | |||
|Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; [[ampicillin]]-[[sulbactam]] or [[clindamycin]]. | |||
|} | |||
==Epidemiology and Demographics== | |||
===Prevalence and incidence=== | |||
The incidence of peritonsillar abscess is highest between November to December and April to May in the northern hemisphere. This has been associated with the highest rates of streptococcal pharyngitis and [[exudative]] [[tonsillitis]] around that these times.<ref name="pmid16448878">{{cite journal| author=Belleza WG, Kalman S| title=Otolaryngologic emergencies in the outpatient setting. | journal=Med Clin North Am | year= 2006 | volume= 90 | issue= 2 | pages= 329-53 | pmid=16448878 | doi=10.1016/j.mcna.2005.12.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16448878 }} </ref><ref name="pmid12087516">{{cite journal| author=Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH, Infectious Diseases Society of America| title=Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America. | journal=Clin Infect Dis | year= 2002 | volume= 35 | issue= 2 | pages= 113-25 | pmid=12087516 | doi=10.1086/340949 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12087516 }} </ref> | |||
===Age=== | |||
Peritonsillar abscess occur in all age groups. The highest occurrence is in adults between 20 to 40 years of age.<ref name="pmid18246890">{{cite journal| author=Galioto NJ| title=Peritonsillar abscess. | journal=Am Fam Physician | year= 2008 | volume= 77 | issue= 2 | pages= 199-202 | pmid=18246890 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18246890 }} </ref><ref name="pmid11804446">{{cite journal| author=Steyer TE| title=Peritonsillar abscess: diagnosis and treatment. | journal=Am Fam Physician | year= 2002 | volume= 65 | issue= 1 | pages= 93-6 | pmid=11804446 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11804446 }} </ref><ref name="pmid16041198">{{cite journal| author=Khayr W, Taepke J| title=Management of peritonsillar abscess: needle aspiration versus incision and drainage versus tonsillectomy. | journal=Am J Ther | year= 2005 | volume= 12 | issue= 4 | pages= 344-50 | pmid=16041198 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16041198 }} </ref> | |||
===Race=== | |||
There is no racial predilection to developing peritonsillar abscess. | |||
===Gender=== | |||
Males are more commonly affected with peritonsillar abscess than female with male to female ratio of approximately 1.4:1. However, equal male to female ratios have been reported in some studies as well.<ref name="pmid15029410">{{cite journal| author=Ong YK, Goh YH, Lee YL| title=Peritonsillar infections: local experience. | journal=Singapore Med J | year= 2004 | volume= 45 | issue= 3 | pages= 105-9 | pmid=15029410 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15029410 }} </ref><ref name="pmid20015734">{{cite journal| author=Marom T, Cinamon U, Itskoviz D, Roth Y| title=Changing trends of peritonsillar abscess. | journal=Am J Otolaryngol | year= 2010 | volume= 31 | issue= 3 | pages= 162-7 | pmid=20015734 | doi=10.1016/j.amjoto.2008.12.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20015734 }} </ref><ref name="pmid24474247">{{cite journal| author=Klug TE| title=Incidence and microbiology of peritonsillar abscess: the influence of season, age, and gender. | journal=Eur J Clin Microbiol Infect Dis | year= 2014 | volume= 33 | issue= 7 | pages= 1163-7 | pmid=24474247 | doi=10.1007/s10096-014-2052-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24474247 }} </ref><ref name="pmid18612664">{{cite journal| author=Gavriel H, Lazarovitch T, Pomortsev A, Eviatar E| title=Variations in the microbiology of peritonsillar abscess. | journal=Eur J Clin Microbiol Infect Dis | year= 2009 | volume= 28 | issue= 1 | pages= 27-31 | pmid=18612664 | doi=10.1007/s10096-008-0583-6 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18612664 }} </ref><ref name="pmid19086341">{{cite journal| author=Sunnergren O, Swanberg J, Mölstad S| title=Incidence, microbiology and clinical history of peritonsillar abscesses. | journal=Scand J Infect Dis | year= 2008 | volume= 40 | issue= 9 | pages= 752-5 | pmid=19086341 | doi=10.1080/00365540802040562 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19086341 }} </ref><ref name="pmid21086007">{{cite journal| author=Hidaka H, Kuriyama S, Yano H, Tsuji I, Kobayashi T| title=Precipitating factors in the pathogenesis of peritonsillar abscess and bacteriological significance of the Streptococcus milleri group. | journal=Eur J Clin Microbiol Infect Dis | year= 2011 | volume= 30 | issue= 4 | pages= 527-32 | pmid=21086007 | doi=10.1007/s10096-010-1114-9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21086007 }} </ref><ref name="pmid22425204">{{cite journal| author=Costales-Marcos M, López-Álvarez F, Núñez-Batalla F, Moreno-Galindo C, Alvarez Marcos C, Llorente-Pendás JL| title=[Peritonsillar infections: prospective study of 100 consecutive cases]. | journal=Acta Otorrinolaringol Esp | year= 2012 | volume= 63 | issue= 3 | pages= 212-7 | pmid=22425204 | doi=10.1016/j.otorri.2012.01.001 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22425204 }} </ref> | |||
===Developed and developing countries=== | |||
Peritonsillar abscess has not been found to vary significantly among countries. | |||
==Risk Factors== | |||
Common risk factors in the development of peritonsillar abscess include:<ref name="pmid16142623">{{cite journal| author=Lehnerdt G, Senska K, Fischer M, Jahnke K| title=[Smoking promotes the formation of peritonsillar abscesses]. | journal=Laryngorhinootologie | year= 2005 | volume= 84 | issue= 9 | pages= 676-9 | pmid=16142623 | doi=10.1055/s-2005-870289 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16142623 }} </ref><ref name="pmid1351238">{{cite journal| author=Dilkes MG, Dilkes JE, Ghufoor K| title=Smoking and quinsy. | journal=Lancet | year= 1992 | volume= 339 | issue= 8808 | pages= 1552 | pmid=1351238 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1351238 }} </ref> | |||
* [[Smoking]] | |||
*Previous peritonsillar abscess episodes | |||
*History of recurrent pharyngotonsillitis | |||
*Poor [[oral hygiene]] | |||
==Screening== | |||
There are no screening recommendations for peritonsillar abscess. | |||
==Natural History, Complications, and Prognosis== | |||
===Natural history=== | |||
Peritonsillar abscess if left untreated may result in extraperitonsillar extension.<ref name="pmid25255362">{{cite journal| author=Coughlin AM, Baugh RF, Pine HS| title=Lingual tonsil abscess with parapharyngeal extension: a case report. | journal=Ear Nose Throat J | year= 2014 | volume= 93 | issue= 9 | pages= E7-8 | pmid=25255362 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25255362 }} </ref><ref name="pmid26591220">{{cite journal| author=Deeva YV| title=[SURGICAL TREATMENT OF TONSILLAR NECK PHLEGMON]. | journal=Klin Khir | year= 2015 | volume= | issue= 7 | pages= 47-8 | pmid=26591220 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26591220 }} </ref> | |||
===Complications=== | |||
The following are some complications that may follow peritonsillar abscess:<ref name="pmid18246890">{{cite journal| author=Galioto NJ| title=Peritonsillar abscess. | journal=Am Fam Physician | year= 2008 | volume= 77 | issue= 2 | pages= 199-202 | pmid=18246890 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18246890 }} </ref><ref name="pmid9231089">{{cite journal| author=Goldenberg D, Golz A, Joachims HZ| title=Retropharyngeal abscess: a clinical review. | journal=J Laryngol Otol | year= 1997 | volume= 111 | issue= 6 | pages= 546-50 | pmid=9231089 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9231089 }} </ref><ref name="pmid2355414">{{cite journal| author=Stevens HE| title=Vascular complication of neck space infection: case report and literature review. | journal=J Otolaryngol | year= 1990 | volume= 19 | issue= 3 | pages= 206-10 | pmid=2355414 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2355414 }} </ref><ref name="pmid7857015">{{cite journal| author=Greinwald JH, Wilson JF, Haggerty PG| title=Peritonsillar abscess: an unlikely cause of necrotizing fasciitis. | journal=Ann Otol Rhinol Laryngol | year= 1995 | volume= 104 | issue= 2 | pages= 133-7 | pmid=7857015 | doi=10.1177/000348949510400209 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7857015 }} </ref><ref name="pmid6594557">{{cite journal| author=Wenig BL, Shikowitz MJ, Abramson AL| title=Necrotizing fasciitis as a lethal complication of peritonsillar abscess. | journal=Laryngoscope | year= 1984 | volume= 94 | issue= 12 Pt 1 | pages= 1576-9 | pmid=6594557 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6594557 }} </ref> | |||
*Extraperitonsillar spread example [[Parapharyngeal space infection|parapharyngeal]] extension, deep neck tissues and [[posterior]] [[mediastinum]]<ref name="pmid25255362">{{cite journal| author=Coughlin AM, Baugh RF, Pine HS| title=Lingual tonsil abscess with parapharyngeal extension: a case report. | journal=Ear Nose Throat J | year= 2014 | volume= 93 | issue= 9 | pages= E7-8 | pmid=25255362 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25255362 }} </ref><ref name="pmid26591220">{{cite journal| author=Deeva YV| title=[SURGICAL TREATMENT OF TONSILLAR NECK PHLEGMON]. | journal=Klin Khir | year= 2015 | volume= | issue= 7 | pages= 47-8 | pmid=26591220 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26591220 }} </ref><ref name="pmid26527518">{{cite journal| author=Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H et al.| title=Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy. | journal=Auris Nasus Larynx | year= 2016 | volume= 43 | issue= 2 | pages= 182-6 | pmid=26527518 | doi=10.1016/j.anl.2015.09.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26527518 }} </ref> | |||
Peritonsillar abscess may spread through the deep fascia of the neck with associated rapid progression to a more serious infection. | |||
*Airway obstruction | |||
*[[Aspiration]] [[pneumonitis]] or lung abscess secondary to peritonsillar abscess rupture | |||
*[[Hemorrhage]] from erosion or septic [[necrosis]] into [[carotid]] sheath | |||
*[[Mediastinitis]] | |||
*Poststreptococcal sequelae (e.g., [[glomerulonephritis]], [[rheumatic fever]]) when infection is caused by [[Group A streptococcus]] | |||
*[[Necrotizing fasciitis]] | |||
===Prognosis=== | |||
The prognosis of peritonsillar abscess is good with early and appropriate treatment.<ref name="pmid22321140">{{cite journal| author=Powell J, Wilson JA| title=An evidence-based review of peritonsillar abscess. | journal=Clin Otolaryngol | year= 2012 | volume= 37 | issue= 2 | pages= 136-45 | pmid=22321140 | doi=10.1111/j.1749-4486.2012.02452.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22321140 }} </ref><ref name="pmid7782170">{{cite journal| author=Apostolopoulos NJ, Nikolopoulos TP, Bairamis TN| title=Peritonsillar abscess in children. Is incision and drainage an effective management? | journal=Int J Pediatr Otorhinolaryngol | year= 1995 | volume= 31 | issue= 2-3 | pages= 129-35 | pmid=7782170 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7782170 }} </ref><ref name="pmid12646835">{{cite journal| author=Johnson RF, Stewart MG, Wright CC| title=An evidence-based review of the treatment of peritonsillar abscess. | journal=Otolaryngol Head Neck Surg | year= 2003 | volume= 128 | issue= 3 | pages= 332-43 | pmid=12646835 | doi=10.1067/mhn.2003.93 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12646835 }} </ref><ref name="pmid7630308">{{cite journal| author=Herzon FS| title=Harris P. Mosher Award thesis. Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines. | journal=Laryngoscope | year= 1995 | volume= 105 | issue= 8 Pt 3 Suppl 74 | pages= 1-17 | pmid=7630308 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7630308 }} </ref> | |||
==Diagnosis== | |||
===History and Symptoms=== | |||
* Unlike [[tonsillitis]], which is more common in the pediatric age group, peritonsillar abscess has a more even age spread — from children to adults. | |||
* Symptoms start appearing 2-8 days before the formation of [[abscess]]. Common symptoms are:<ref name="pmid18246890">{{cite journal| author=Galioto NJ| title=Peritonsillar abscess. | journal=Am Fam Physician | year= 2008 | volume= 77 | issue= 2 | pages= 199-202 | pmid=18246890 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18246890 }} </ref> | |||
:*[[Drooling]] | |||
:*[[Dysphagia]] | |||
:*Foul smelling breath | |||
:*[[Fever]] | |||
:*[[Headache]] | |||
:*[[Hoarseness]], muffled voice (also called ''hot potato voice'') | |||
:*[[Odynophagia]] | |||
:*[[Otalgia]] (on the side of the abscess) | |||
:*[[Sore throat]] ( may be severe and unilateral) | |||
:*[[Stridor]]<ref>{{cite book | last = Ferri | first = Fred | title = Ferri's clinical advisor 2015 : 5 books in 1 | publisher = Elsevier/Mosby | location = Philadelphia, PA | year = 2015 | isbn = 978-0323083751 }}</ref> | |||
:*[[Malaise]] | |||
===Physical Examination=== | |||
Physical examination findings suggestive of peritonsillar abscess include the following:<ref name="pmid18246890">{{cite journal| author=Galioto NJ| title=Peritonsillar abscess. | journal=Am Fam Physician | year= 2008 | volume= 77 | issue= 2 | pages= 199-202 | pmid=18246890 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18246890 }} </ref><ref>{{cite book | last = Ferri | first = Fred | title = Ferri's clinical advisor 2015 : 5 books in 1 | publisher = Elsevier/Mosby | location = Philadelphia, PA | year = 2015 | isbn = 978-0323083751 }}</ref><ref name="pmid8302122">{{cite journal| author=Passy V| title=Pathogenesis of peritonsillar abscess. | journal=Laryngoscope | year= 1994 | volume= 104 | issue= 2 | pages= 185-90 | pmid=8302122 | doi=10.1288/00005537-199402000-00011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8302122 }} </ref><ref name="pmid11127146">{{cite journal| author=Nwe TT, Singh B| title=Management of pain in peritonsillar abscess. | journal=J Laryngol Otol | year= 2000 | volume= 114 | issue= 10 | pages= 765-7 | pmid=11127146 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11127146 }} </ref> | |||
====Appearance of the Patient==== | |||
* They are usually acutely-ill looking. | |||
====Vital Signs==== | |||
* High [[temperature]] | |||
====HEENT==== | |||
*Muffled voice (also called "hot potato voice") | |||
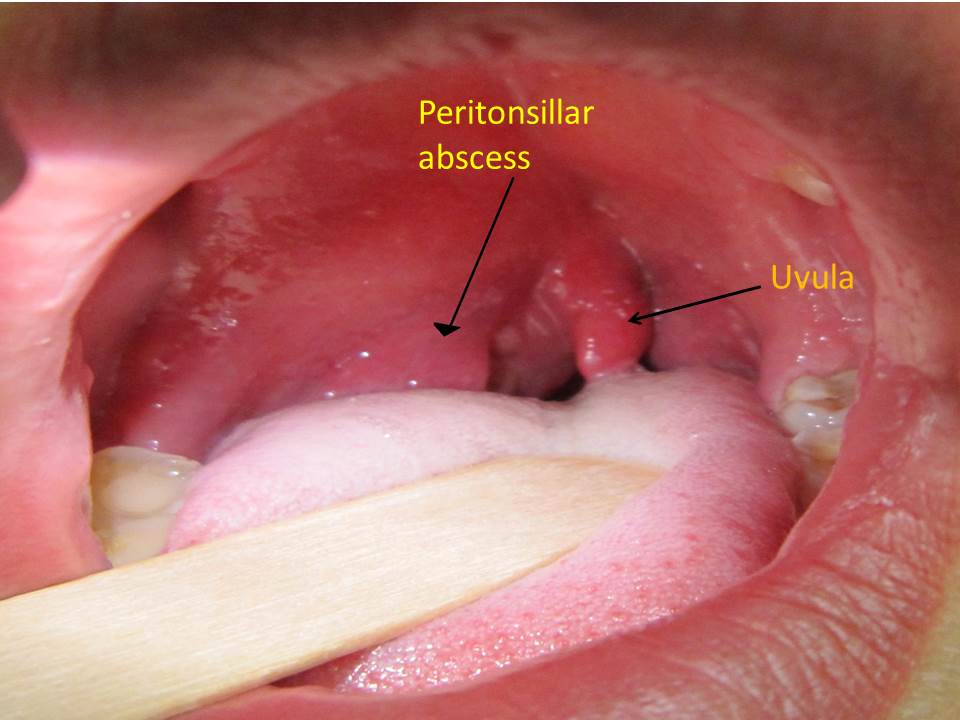
* [[Contralateral]] deflection of the uvula (see image below) | |||
*The [[tonsil]] is generally displaced [[inferiorly]] and [[medially]] | |||
* Facial swelling | |||
* [[Tonsillar abscess|Tonsillar]] [[hypertrophy]] with likely Peritonsillar [[edema]] (see image below) | |||
* [[Trismus]] | |||
* [[Drooling]] | |||
* [[Rancidification|Rancid]] or [[Fetor oris|fetor]] breath | |||
Image below shows edematous and [[inflamed]] tonsillar with contralacteral uvula deviation:<ref name =abc>DescriptionEnglish: A right sided peritonsilar abscess Date 13 May 2011 Source Own work Author James Heilman,MD wikimedia commons https://commons.wikimedia.org/wiki/File:PeritonsilarAbsess.jpg</ref> | |||
[[Image:PTA2.jpg|200PX]] | |||
====Neck==== | |||
* [[Tenderness]] of [[anterior]] neck | |||
* Tender [[submandibular]] and [[anterior]] [[cervical lymph nodes]] | |||
====Lungs==== | |||
* May be in obvious respiratory distress with flaring of ala nasi, subcostal and intercostal recessions. | |||
* Increased respiratory rate in both children and adults | |||
* Decreased air-entry depending of degree of airway obstruction | |||
====Extremities==== | |||
* [[Cyanosis]] | |||
===Laboratory Findings=== | |||
Although the diagnosis of peritonsillar abscess may be made without the use of laboratory findings, the following nonspecific laboratory findings may be seen:<ref name="pmid23612569">{{cite journal| author=Powell EL, Powell J, Samuel JR, Wilson JA| title=A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation. | journal=J Antimicrob Chemother | year= 2013 | volume= 68 | issue= 9 | pages= 1941-50 | pmid=23612569 | doi=10.1093/jac/dkt128 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23612569 }} </ref><ref name=abd>L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286</ref><ref name="pmid8302122">{{cite journal| author=Passy V| title=Pathogenesis of peritonsillar abscess. | journal=Laryngoscope | year= 1994 | volume= 104 | issue= 2 | pages= 185-90 | pmid=8302122 | doi=10.1288/00005537-199402000-00011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8302122 }} </ref><ref name="pmid25865201">{{cite journal| author=Blair AB, Booth R, Baugh R| title=A unifying theory of tonsillitis, intratonsillar abscess and peritonsillar abscess. | journal=Am J Otolaryngol | year= 2015 | volume= 36 | issue= 4 | pages= 517-20 | pmid=25865201 | doi=10.1016/j.amjoto.2015.03.002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25865201 }} </ref><ref name="pmid16643771">{{cite journal| author=Herzon FS, Martin AD| title=Medical and surgical treatment of peritonsillar, retropharyngeal, and parapharyngeal abscesses. | journal=Curr Infect Dis Rep | year= 2006 | volume= 8 | issue= 3 | pages= 196-202 | pmid=16643771 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16643771 }} </ref> | |||
*[[Complete blood count]] with differential | |||
:*This usually shows [[leukocytosis]] with neutrophilic predominance | |||
*Serum [[Electrolyte|electrolytes]] | |||
:*This is useful too in patients presenting with [[dehydration]] | |||
*[[Gram stain]], culture and sensitivity for sample after abscess drainage. | |||
:*Emperic therapy should be initiated and modified accordingly when results are ready. | |||
*A routine [[throat culture]] for [[group A streptococcus]]. | |||
===Imaging Findings=== | |||
The diagnosis of peritonsillar abscess may be made without the use of imaging however, imaging options may help in differentiating peritonsillar abscess from other simialr conditions example, peritonsillar cellulitis, retropharyngeal abscess and epiglottitis. | |||
====Ultrasound==== | |||
This is helpful in differentiating peritonsillar abscess from peritonsillar cellulitis as well as a guide during abscess drainage. | |||
The approach may be intraoral or submandibular.<ref name="pmid22687177">{{cite journal| author=Costantino TG, Satz WA, Dehnkamp W, Goett H| title=Randomized trial comparing intraoral ultrasound to landmark-based needle aspiration in patients with suspected peritonsillar abscess. | journal=Acad Emerg Med | year= 2012 | volume= 19 | issue= 6 | pages= 626-31 | pmid=22687177 | doi=10.1111/j.1553-2712.2012.01380.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22687177 }} </ref><ref name="pmid26637999">{{cite journal| author=Bandarkar AN, Adeyiga AO, Fordham MT, Preciado D, Reilly BK| title=Tonsil ultrasound: technical approach and spectrum of pediatric peritonsillar infections. | journal=Pediatr Radiol | year= 2016 | volume= 46 | issue= 7 | pages= 1059-67 | pmid=26637999 | doi=10.1007/s00247-015-3505-7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26637999 }} </ref><ref name="pmid8141026">{{cite journal| author=Buckley AR, Moss EH, Blokmanis A| title=Diagnosis of peritonsillar abscess: value of intraoral sonography. | journal=AJR Am J Roentgenol | year= 1994 | volume= 162 | issue= 4 | pages= 961-4 | pmid=8141026 | doi=10.2214/ajr.162.4.8141026 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8141026 }} </ref><ref name="pmid7630286">{{cite journal| author=Strong EB, Woodward PJ, Johnson LP| title=Intraoral ultrasound evaluation of peritonsillar abscess. | journal=Laryngoscope | year= 1995 | volume= 105 | issue= 8 Pt 1 | pages= 779-82 | pmid=7630286 | doi=10.1288/00005537-199508000-00002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7630286 }} </ref><ref name="pmid12671820">{{cite journal| author=Blaivas M, Theodoro D, Duggal S| title=Ultrasound-guided drainage of peritonsillar abscess by the emergency physician. | journal=Am J Emerg Med | year= 2003 | volume= 21 | issue= 2 | pages= 155-8 | pmid=12671820 | doi=10.1053/ajem.2003.50029 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12671820 }} </ref> | |||
On ultrasound the following may be found:<ref name="pmid15635144">{{cite journal| author=Lyon M, Blaivas M| title=Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. | journal=Acad Emerg Med | year= 2005 | volume= 12 | issue= 1 | pages= 85-8 | pmid=15635144 | doi=10.1197/j.aem.2004.08.045 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15635144 }} </ref><ref name="pmid1642863">{{cite journal| author=Boesen T, Jensen F| title=Preoperative ultrasonographic verification of peritonsillar abscesses in patients with severe tonsillitis. | journal=Eur Arch Otorhinolaryngol | year= 1992 | volume= 249 | issue= 3 | pages= 131-3 | pmid=1642863 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1642863 }} </ref><ref name="pmid26637999">{{cite journal| author=Bandarkar AN, Adeyiga AO, Fordham MT, Preciado D, Reilly BK| title=Tonsil ultrasound: technical approach and spectrum of pediatric peritonsillar infections. | journal=Pediatr Radiol | year= 2016 | volume= 46 | issue= 7 | pages= 1059-67 | pmid=26637999 | doi=10.1007/s00247-015-3505-7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26637999 }} </ref><ref name="pmid10435129">{{cite journal| author=Scott PM, Loftus WK, Kew J, Ahuja A, Yue V, van Hasselt CA| title=Diagnosis of peritonsillar infections: a prospective study of ultrasound, computerized tomography and clinical diagnosis. | journal=J Laryngol Otol | year= 1999 | volume= 113 | issue= 3 | pages= 229-32 | pmid=10435129 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10435129 }} </ref><ref name="pmid15635144">{{cite journal| author=Lyon M, Blaivas M| title=Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. | journal=Acad Emerg Med | year= 2005 | volume= 12 | issue= 1 | pages= 85-8 | pmid=15635144 | doi=10.1197/j.aem.2004.08.045 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15635144 }} </ref><ref name="pmid1642863">{{cite journal| author=Boesen T, Jensen F| title=Preoperative ultrasonographic verification of peritonsillar abscesses in patients with severe tonsillitis. | journal=Eur Arch Otorhinolaryngol | year= 1992 | volume= 249 | issue= 3 | pages= 131-3 | pmid=1642863 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1642863 }} </ref> | |||
*Peritonsillar abscess appears as focal irregularly marginated hypoechoic area. | |||
*Irregular hypoechoic areas within the tonsil may represent pockets of developing purulence or necrosis called intratonsillar abscesses. | |||
*Peritonsillar cellulitis appears as enlarged tonsil (arrows) with ill-defined margins and markedly increased echogenicity of surrounding soft tissues that suggests significant inflammatory change/cellulitis. | |||
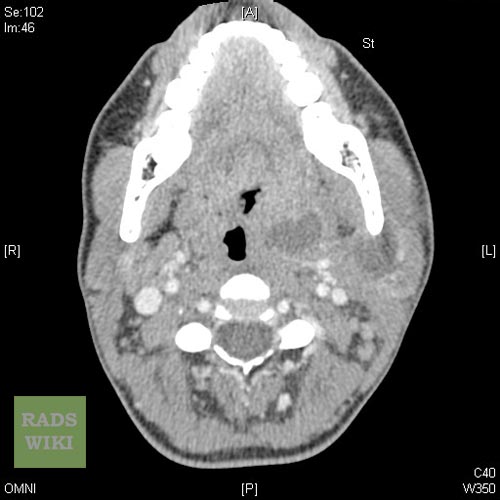
====CT scan==== | |||
Coronal contrast-enhanced CT scan of the neck may identify the peritonsillar abscess.<ref name="pmid26637999">{{cite journal| author=Bandarkar AN, Adeyiga AO, Fordham MT, Preciado D, Reilly BK| title=Tonsil ultrasound: technical approach and spectrum of pediatric peritonsillar infections. | journal=Pediatr Radiol | year= 2016 | volume= 46 | issue= 7 | pages= 1059-67 | pmid=26637999 | doi=10.1007/s00247-015-3505-7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26637999 }} </ref> | |||
==Treatment== | |||
===Medical Therapy=== | |||
Parenteral therapy is the preferred first line route of administration until the temperature of the patient has settled and clinically improved and then switched to oral therapy to complete a 14-day course.<ref name="pmid7782170">{{cite journal| author=Apostolopoulos NJ, Nikolopoulos TP, Bairamis TN| title=Peritonsillar abscess in children. Is incision and drainage an effective management? | journal=Int J Pediatr Otorhinolaryngol | year= 1995 | volume= 31 | issue= 2-3 | pages= 129-35 | pmid=7782170 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7782170 }} </ref> | |||
====Antimicrobial Regimen==== | |||
Below are the antimicrobial regimen available in treating peritonsillar abscess.<ref name=abc>Principles and Practice of Pediatric Infectious Diseases, 4th ed, Long SS, Pickering LK, Prober CG (Eds), Elsevier Saunders, New York 2012. p.205.</ref> | |||
:::* Preferred regimen in adults: [[Ampicillin-sulbactam]] 3 g IV 6h | |||
:::* Preferred regimen in children: [[Ampicillin-sulbactam]] 50 mg/kg per dose [maximum single dose 3 g] IV 6h | |||
:::* Alternative regimen in adults: [[Clindamycin]] 600mg IV 6-8h | |||
:::* Alternative regimen in children: [[Clindamycin]] 13 mg/kg per dose [maximum single dose 900 mg] IV 8h | |||
The above alternative therapy are employed in the following situations: | |||
*Patients not improving on [[Ampicillin-Sulbactam|Ampicillin-sulbactam]] or [[Clindamycin]] | |||
*Severe infection presenting with; | |||
**Toxic appearance, | |||
**Temperature >39°C, | |||
**[[Drooling]], and/or [[respiratory distress]]) | |||
'''Pathogen-directed antimicrobial therapy''' | |||
*'''Resistant Gram-positive cocci''' | |||
For resistant Gram-positive cocci infections IV [[Vancomycin]] or [[Linezolid]] is added to the above emperic therapy. | |||
===Surgery=== | |||
Surgical modalities in the management of peritonsillar abscess involve the use of the following: | |||
*[[Incision and drainage]], or | |||
*[[Tonsillectomy]] | |||
====Indications for [[tonsillectomy]] in peritonsillar abscess==== | |||
*Severe upper respirtaory obstruction | |||
*Previous episodes of severe recurrent [[pharyngitis]] or peritonsillar abscess | |||
*Unresolving peritonsillar abscess after antibiotics [[incision and drainage]] | |||
==Prevention== | |||
There are no definite preventive measures for peritonsillar abscess, however, immunization against certain organisms in chikdhood may decrease the burden of peritonsillar abscess resulting from such infections. | |||
*[[Immunization]] with the [[Hib]] vaccine protects children.<ref name="pmid18931398">{{cite journal| author=Mathoera RB, Wever PC, van Dorsten FR, Balter SG, de Jager CP| title=Epiglottitis in the adult patient. | journal=Neth J Med | year= 2008 | volume= 66 | issue= 9 | pages= 373-7 | pmid=18931398 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18931398 }} </ref> | |||
*In the United states, [[vaccination]] against [[Haemophilus influenzae infection|Hib]] in children was initiated in the 1980s. Immunity against Hib has been adequate with an increasing level of [[immunization]] among children. | |||
* Post-[[splenectomy]] patients are also recommended to be immunized.<ref name="pmid18931398">{{cite journal| author=Mathoera RB, Wever PC, van Dorsten FR, Balter SG, de Jager CP| title=Epiglottitis in the adult patient. | journal=Neth J Med | year= 2008 | volume= 66 | issue= 9 | pages= 373-7 | pmid=18931398 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18931398 }} </ref> | |||
==References== | |||
{{Reflist|2}} | |||
==External links== | |||
*[http://icarus.med.utoronto.ca/carr/manual/pta.html Practical ENT For Primary Care Physicians web site] | |||
*[http://www.drtbalu.com/quinsy.html (Detailed description with video clipping)] | |||
{{Respiratory pathology}} | |||
[[Category:Bacterial diseases]] | |||
[[ka:პერიტონზილური აბსცესი]] | |||
[[nl:Peritonsillair abces]] | |||
[[fi:Kurkkupaise]] | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
Revision as of 20:45, 2 March 2017
| Peritonsillar abscess | |
| ICD-10 | J36 |
|---|---|
| ICD-9 | 475 |
| DiseasesDB | 11141 |
| eMedicine | emerg/417 |
|
WikiDoc Resources for Sandbox:Prince |
|
Articles |
|---|
|
Most recent articles on Sandbox:Prince Most cited articles on Sandbox:Prince |
|
Media |
|
Powerpoint slides on Sandbox:Prince |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sandbox:Prince at Clinical Trials.gov Trial results on Sandbox:Prince Clinical Trials on Sandbox:Prince at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox:Prince NICE Guidance on Sandbox:Prince
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox:Prince Discussion groups on Sandbox:Prince Patient Handouts on Sandbox:Prince Directions to Hospitals Treating Sandbox:Prince Risk calculators and risk factors for Sandbox:Prince
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox:Prince |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Kiran Singh, M.D. [2] Prince Tano Djan, BSc, MBChB [3]
Synonyms and keywords: PTA, tonsillar abscess, intratonsillar abscess
Overview
Peritonsillar abscess (PTA), also commonly referred to as quinsy, is defined as a collection of pus located between the tonsillar capsule and the pharyngeal constrictor muscles. It is the most common deep tissue infection of the neck.[1] Historically, it has been thought of as a complication of acute tonsillitis. However, recent studies have proposed additional hypothesis surrounding its pathogenesis making the understanding of the disease a medical dilemma.[2]
Historical perspective
The outline below shows the historical perspective of peritonsillar abscess.[3]
- In second and third century BC, Celcius was the first to document in literature the treatment and pathogenesis of tonsillar pathology.
- In 1700s peritonsillar abscess was first described.
- In the 1930s and 1940s prior to the advent of antibiotics, surgical management was the most common treatment option for peritonsillar abscess. Interval tonsillectomy was mostly done after symptom resolution.
- By 1947, Chaud tonsillectomy or immediate surgical tonsillectomy became the treatment option.
Classification
On the basis of computed tomographical findings, peritonsillar abscess may be classified into 3 broad categories based on the following:
1. Shape of the abscess
On the basis of shape it may be classified as:[4]
- Oval type or
- Cap type
2. Location of the abscess
On the basis of abscess location it may be differentiated into the following:[4]
- Superior or
- Inferior
3. Shape and location
On the basis of shaped and location it may be classified as:[4]
Pathophysiology
Anatomy
A good understanding of the tonsil and its surrounding space is important in the pathogenesis of peritonsillar abscess. The palatine tonsils are found in an anatomical structure called tonsillar fossa. This fossa is bounded anteriorly by palatoglossal muscle, posteriorly by palatopharyngeal muscle, laterally by a fibrous capsule and tonsillar crypts medially. Contents of the tonsillar crypts are expelled by contraction of the tonsillopharyngeus muscle.[5] The tonsils form during the last months of pregnancy and becomes fully formed by 6 to 7 years of age. It then undergoes involution until small size remains in older population. Located within the soft palate is the supratonsillar space occupied by series of 20 to 25 salivary glands described as Weber's glands. The ducts of these glands form a common duct which opens onto the posterior surface of the tonsil after passing through the tonsillar capsule. It is proposed that the secretions from these glands play a rule in food digestion. Peritonsillar abscesses form in the area between the palatine tonsil and its capsule.
Pathogenesis
The pathogenesis of peritonsillar abscess is still not well-understood.[2] There are two proposed theories believed to be involved in the pathogensis of peritonsillar abscess formation.[5][3][6][7]
- 1. It is proposed to arise from an extension of exudative tonsillitis.
Some authorities believe that blockage of drainage from tonsillar crypt in acute tonsillitis results in spread of infection into the peritonsillar space.
- 2. Involvement of Weber's gland account for the abscess formation. Some believe that peritonsillar abscess arises from infectious process involving group of salivary glands called Weber's glands located in the supratonsillar space.
Antigenic response following any disturbance arising from within the tonsillar crypt mucosa allows for lymphocytic interaction. This disruption in the crypt epithelium may be preceded by infectious process. Invasion and proliferation of the tonsillar crypt by infectious pathogens results in localized edema and influx of neutrophils. This is clinically seen as inflamed tonsil with or without exudation.[5] Pus accumulation within tissue behind the supratonsillar space leads to tonsillar bulging, uvula and palate deviation.
Causes
Peritonsillar abscess (PTA) usually arises as a complication of an untreated or partially treated episode of acute tonsillitis. The infection, in these cases, spreads to the peritonsillar area (peritonsillitis). This region comprises of loose connective tissue and is hence susceptible to formation of abscess. Peritonsilar abscess can also occur de novo. Both aerobic and anaerobic bacteria can be causative.[8][8]
Life-threatening causes
Life-threatening conditions may result in death or permanent disability within 24 hours if left untreated. Peritonsillar abscess may become a life-threatening condition and must be treated as such irrespective of the cause.[9][8]
Most common cause
The most frequent pathogen of peritonsillar abscess is Streptococcus pyogenes.[9][8][10][11]
Common causes
Some common causes of peritonsillar abscess include:[9][8]
- Fusobacterium necrophorum
- Streptococcus milleri
- Staphylococci
- Haemophilus
- Fusobacterium
- Prevotella
- Acinetobacter spp.
- Candida albicans
- Peptostreptococcus spp.
- Pseudomonas spp.
- Enterobacter spp.
- Klebsiella
Less common causes
Less common causes of peritonsillar abscess include:[9][8]
Differentiating Peritonsillar abscess from Other Diseases
| Disease/Variable | Presentation | Causes | Physical exams findings | Age commonly affected | Imaging finding | Treatment |
|---|---|---|---|---|---|---|
| Peritonsillar abscess | Severe sore throat, otalgia fever, a "hot potato" or muffled voice, drooling, and trismus[1] | Aerobic and anaerobic | Contralateral deflection of the uvula,
the tonsil is displaced inferiorly and medially, tender submandibular and anterior cervical lymph nodes, tonsillar hypertrophy with likely peritonsillar edema. |
The highest occurrence is in adults between 20 to 40 years of age.[1] | On ultrasound peritonsillar abscess appears as focal irregularly marginated hypoechoic area.[12][13][14][15][12][13] | Ampicillin-sulbactam, Clindamycin, Vancomycin or Linezolid |
| Croup | Has cough and stridor but no drooling. Others are Hoarseness, Difficulty breathing, symptoms of the common cold, Runny nose, Fever | Parainfluenza virus | Suprasternal and intercostal indrawing,[16] Inspiratory stridor[17], expiratory wheezing,[17] Sternal wall retractions[18] | Mainly 6 months and 3 years old
rarely, adolescents and adults[19] |
Steeple sign on neck X-ray | Dexamethasone and nebulised epinephrine |
| Epiglottitis | Has stridor and drooling but no cough. Other symptoms include difficulty breathing, fever, chills, difficulty swallowing, hoarseness of voice | H. influenza type b, | Cyanosis, Cervical lymphadenopathy, Inflammed epiglottis | Used to be mostly found in
pediatric age group between 3 to 5 years, however, recent trend favors adults as most commonly affected individuals[20] with a mean age of 44.94 years |
Thumbprint sign on neck x-ray | Airway maintenance, parenteral Cefotaxime or Ceftriaxone in combination with Vancomycin. Adjuvant therapy includes corticosteroids and racemic Epinephrine.[21][22] |
| Pharyngitis | Sore throat, pain on swallowing, fever, headache, abdominal pain, nausea and vomiting | Group A beta-hemolytic | Inflammed pharynx with or without exudate | Mostly in children and young adults,
with 50% of cases identified between the ages of 5 to 24 years.[23] |
_ | Antimicrobial therapy mainly penicillin-based and analgesics. |
| Tonsilitis | Sore throat, pain on swallowing, fever, headache, cough | Most common cause is
viral including adenovirus, coronavirus, and Second most common causes are bacterial; |
Fever, especially 100°F or higher.[25][26]Erythema, edema and Exudate of the tonsils.[27] cervical lymphadenopathy, Dysphonia.[28] | Primarily affects children
between 5 and 15 years old.[29] |
Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.[4][30][31] | Antimicrobial therapy mainly penicillin-based and analgesics with tonsilectomy in selected cases. |
| Retropharyngeal abscess | Neck pain, stiff neck, torticollis | Polymicrobial infection.
Mostly; Streptococcus pyogenes, Staphylococcus aureus and respiratory anaerobes (example; Fusobacteria, Prevotella, |
Child may be unable to open the mouth widely. May have enlarged
cervical lymph nodes and neck mass. |
Mostly between 2-4 years, but can occur in other age groups.[37][38] | On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen[39][40] | Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; ampicillin-sulbactam or clindamycin. |
Epidemiology and Demographics
Prevalence and incidence
The incidence of peritonsillar abscess is highest between November to December and April to May in the northern hemisphere. This has been associated with the highest rates of streptococcal pharyngitis and exudative tonsillitis around that these times.[41][42]
Age
Peritonsillar abscess occur in all age groups. The highest occurrence is in adults between 20 to 40 years of age.[1][43][44]
Race
There is no racial predilection to developing peritonsillar abscess.
Gender
Males are more commonly affected with peritonsillar abscess than female with male to female ratio of approximately 1.4:1. However, equal male to female ratios have been reported in some studies as well.[45][46][47][48][49][50][51]
Developed and developing countries
Peritonsillar abscess has not been found to vary significantly among countries.
Risk Factors
Common risk factors in the development of peritonsillar abscess include:[52][53]
- Smoking
- Previous peritonsillar abscess episodes
- History of recurrent pharyngotonsillitis
- Poor oral hygiene
Screening
There are no screening recommendations for peritonsillar abscess.
Natural History, Complications, and Prognosis
Natural history
Peritonsillar abscess if left untreated may result in extraperitonsillar extension.[54][55]
Complications
The following are some complications that may follow peritonsillar abscess:[1][56][57][58][59]
- Extraperitonsillar spread example parapharyngeal extension, deep neck tissues and posterior mediastinum[54][55][4]
Peritonsillar abscess may spread through the deep fascia of the neck with associated rapid progression to a more serious infection.
- Airway obstruction
- Aspiration pneumonitis or lung abscess secondary to peritonsillar abscess rupture
- Hemorrhage from erosion or septic necrosis into carotid sheath
- Mediastinitis
- Poststreptococcal sequelae (e.g., glomerulonephritis, rheumatic fever) when infection is caused by Group A streptococcus
- Necrotizing fasciitis
Prognosis
The prognosis of peritonsillar abscess is good with early and appropriate treatment.[60][61][62][63]
Diagnosis
History and Symptoms
- Unlike tonsillitis, which is more common in the pediatric age group, peritonsillar abscess has a more even age spread — from children to adults.
- Drooling
- Dysphagia
- Foul smelling breath
- Fever
- Headache
- Hoarseness, muffled voice (also called hot potato voice)
- Odynophagia
- Otalgia (on the side of the abscess)
- Sore throat ( may be severe and unilateral)
- Stridor[64]
- Malaise
Physical Examination
Physical examination findings suggestive of peritonsillar abscess include the following:[1][65][3][66]
Appearance of the Patient
- They are usually acutely-ill looking.
Vital Signs
- High temperature
HEENT
- Muffled voice (also called "hot potato voice")
- Contralateral deflection of the uvula (see image below)
- The tonsil is generally displaced inferiorly and medially
- Facial swelling
- Tonsillar hypertrophy with likely Peritonsillar edema (see image below)
- Trismus
- Drooling
- Rancid or fetor breath
Image below shows edematous and inflamed tonsillar with contralacteral uvula deviation:[67]
Neck
- Tenderness of anterior neck
- Tender submandibular and anterior cervical lymph nodes
Lungs
- May be in obvious respiratory distress with flaring of ala nasi, subcostal and intercostal recessions.
- Increased respiratory rate in both children and adults
- Decreased air-entry depending of degree of airway obstruction
Extremities
Laboratory Findings
Although the diagnosis of peritonsillar abscess may be made without the use of laboratory findings, the following nonspecific laboratory findings may be seen:[2][5][3][6][7]
- Complete blood count with differential
- This usually shows leukocytosis with neutrophilic predominance
- Serum electrolytes
- This is useful too in patients presenting with dehydration
- Gram stain, culture and sensitivity for sample after abscess drainage.
- Emperic therapy should be initiated and modified accordingly when results are ready.
- A routine throat culture for group A streptococcus.
Imaging Findings
The diagnosis of peritonsillar abscess may be made without the use of imaging however, imaging options may help in differentiating peritonsillar abscess from other simialr conditions example, peritonsillar cellulitis, retropharyngeal abscess and epiglottitis.
Ultrasound
This is helpful in differentiating peritonsillar abscess from peritonsillar cellulitis as well as a guide during abscess drainage. The approach may be intraoral or submandibular.[68][14][69][70][71]
On ultrasound the following may be found:[12][13][14][15][12][13]
- Peritonsillar abscess appears as focal irregularly marginated hypoechoic area.
- Irregular hypoechoic areas within the tonsil may represent pockets of developing purulence or necrosis called intratonsillar abscesses.
- Peritonsillar cellulitis appears as enlarged tonsil (arrows) with ill-defined margins and markedly increased echogenicity of surrounding soft tissues that suggests significant inflammatory change/cellulitis.
CT scan
Coronal contrast-enhanced CT scan of the neck may identify the peritonsillar abscess.[14]
Treatment
Medical Therapy
Parenteral therapy is the preferred first line route of administration until the temperature of the patient has settled and clinically improved and then switched to oral therapy to complete a 14-day course.[61]
Antimicrobial Regimen
Below are the antimicrobial regimen available in treating peritonsillar abscess.[67]
- Preferred regimen in adults: Ampicillin-sulbactam 3 g IV 6h
- Preferred regimen in children: Ampicillin-sulbactam 50 mg/kg per dose [maximum single dose 3 g] IV 6h
- Alternative regimen in adults: Clindamycin 600mg IV 6-8h
- Alternative regimen in children: Clindamycin 13 mg/kg per dose [maximum single dose 900 mg] IV 8h
The above alternative therapy are employed in the following situations:
- Patients not improving on Ampicillin-sulbactam or Clindamycin
- Severe infection presenting with;
- Toxic appearance,
- Temperature >39°C,
- Drooling, and/or respiratory distress)
Pathogen-directed antimicrobial therapy
- Resistant Gram-positive cocci
For resistant Gram-positive cocci infections IV Vancomycin or Linezolid is added to the above emperic therapy.
Surgery
Surgical modalities in the management of peritonsillar abscess involve the use of the following:
Indications for tonsillectomy in peritonsillar abscess
- Severe upper respirtaory obstruction
- Previous episodes of severe recurrent pharyngitis or peritonsillar abscess
- Unresolving peritonsillar abscess after antibiotics incision and drainage
Prevention
There are no definite preventive measures for peritonsillar abscess, however, immunization against certain organisms in chikdhood may decrease the burden of peritonsillar abscess resulting from such infections.
- Immunization with the Hib vaccine protects children.[72]
- In the United states, vaccination against Hib in children was initiated in the 1980s. Immunity against Hib has been adequate with an increasing level of immunization among children.
- Post-splenectomy patients are also recommended to be immunized.[72]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Galioto NJ (2008). "Peritonsillar abscess". Am Fam Physician. 77 (2): 199–202. PMID 18246890.
- ↑ 2.0 2.1 2.2 Powell EL, Powell J, Samuel JR, Wilson JA (2013). "A review of the pathogenesis of adult peritonsillar abscess: time for a re-evaluation". J Antimicrob Chemother. 68 (9): 1941–50. doi:10.1093/jac/dkt128. PMID 23612569.
- ↑ 3.0 3.1 3.2 3.3 Passy V (1994). "Pathogenesis of peritonsillar abscess". Laryngoscope. 104 (2): 185–90. doi:10.1288/00005537-199402000-00011. PMID 8302122.
- ↑ 4.0 4.1 4.2 4.3 4.4 Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H; et al. (2016). "Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy". Auris Nasus Larynx. 43 (2): 182–6. doi:10.1016/j.anl.2015.09.014. PMID 26527518.
- ↑ 5.0 5.1 5.2 5.3 L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286
- ↑ 6.0 6.1 Blair AB, Booth R, Baugh R (2015). "A unifying theory of tonsillitis, intratonsillar abscess and peritonsillar abscess". Am J Otolaryngol. 36 (4): 517–20. doi:10.1016/j.amjoto.2015.03.002. PMID 25865201.
- ↑ 7.0 7.1 Herzon FS, Martin AD (2006). "Medical and surgical treatment of peritonsillar, retropharyngeal, and parapharyngeal abscesses". Curr Infect Dis Rep. 8 (3): 196–202. PMID 16643771.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Megalamani SB, Suria G, Manickam U, Balasubramanian D, Jothimahalingam S (2008). "Changing trends in bacteriology of peritonsillar abscess". J Laryngol Otol. 122 (9): 928–30. doi:10.1017/S0022215107001144. PMID 18039418.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Brook I (2004). "Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses". J Oral Maxillofac Surg. 62 (12): 1545–50. PMID 15573356.
- ↑ 10.0 10.1 Snow DG, Campbell JB, Morgan DW (1991). "The microbiology of peritonsillar sepsis". J Laryngol Otol. 105 (7): 553–5. PMID 1875138.
- ↑ 11.0 11.1 Matsuda A, Tanaka H, Kanaya T, Kamata K, Hasegawa M (2002). "Peritonsillar abscess: a study of 724 cases in Japan". Ear Nose Throat J. 81 (6): 384–9. PMID 12092281.
- ↑ 12.0 12.1 12.2 12.3 Lyon M, Blaivas M (2005). "Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department". Acad Emerg Med. 12 (1): 85–8. doi:10.1197/j.aem.2004.08.045. PMID 15635144.
- ↑ 13.0 13.1 13.2 13.3 Boesen T, Jensen F (1992). "Preoperative ultrasonographic verification of peritonsillar abscesses in patients with severe tonsillitis". Eur Arch Otorhinolaryngol. 249 (3): 131–3. PMID 1642863.
- ↑ 14.0 14.1 14.2 14.3 Bandarkar AN, Adeyiga AO, Fordham MT, Preciado D, Reilly BK (2016). "Tonsil ultrasound: technical approach and spectrum of pediatric peritonsillar infections". Pediatr Radiol. 46 (7): 1059–67. doi:10.1007/s00247-015-3505-7. PMID 26637999.
- ↑ 15.0 15.1 Scott PM, Loftus WK, Kew J, Ahuja A, Yue V, van Hasselt CA (1999). "Diagnosis of peritonsillar infections: a prospective study of ultrasound, computerized tomography and clinical diagnosis". J Laryngol Otol. 113 (3): 229–32. PMID 10435129.
- ↑
- ↑ 17.0 17.1
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑
- ↑ Belleza WG, Kalman S (2006). "Otolaryngologic emergencies in the outpatient setting". Med Clin North Am. 90 (2): 329–53. doi:10.1016/j.mcna.2005.12.001. PMID 16448878.
- ↑ Bisno AL, Gerber MA, Gwaltney JM, Kaplan EL, Schwartz RH, Infectious Diseases Society of America (2002). "Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America". Clin Infect Dis. 35 (2): 113–25. doi:10.1086/340949. PMID 12087516.
- ↑ Steyer TE (2002). "Peritonsillar abscess: diagnosis and treatment". Am Fam Physician. 65 (1): 93–6. PMID 11804446.
- ↑ Khayr W, Taepke J (2005). "Management of peritonsillar abscess: needle aspiration versus incision and drainage versus tonsillectomy". Am J Ther. 12 (4): 344–50. PMID 16041198.
- ↑ Ong YK, Goh YH, Lee YL (2004). "Peritonsillar infections: local experience". Singapore Med J. 45 (3): 105–9. PMID 15029410.
- ↑ Marom T, Cinamon U, Itskoviz D, Roth Y (2010). "Changing trends of peritonsillar abscess". Am J Otolaryngol. 31 (3): 162–7. doi:10.1016/j.amjoto.2008.12.003. PMID 20015734.
- ↑ Klug TE (2014). "Incidence and microbiology of peritonsillar abscess: the influence of season, age, and gender". Eur J Clin Microbiol Infect Dis. 33 (7): 1163–7. doi:10.1007/s10096-014-2052-8. PMID 24474247.
- ↑ Gavriel H, Lazarovitch T, Pomortsev A, Eviatar E (2009). "Variations in the microbiology of peritonsillar abscess". Eur J Clin Microbiol Infect Dis. 28 (1): 27–31. doi:10.1007/s10096-008-0583-6. PMID 18612664.
- ↑ Sunnergren O, Swanberg J, Mölstad S (2008). "Incidence, microbiology and clinical history of peritonsillar abscesses". Scand J Infect Dis. 40 (9): 752–5. doi:10.1080/00365540802040562. PMID 19086341.
- ↑ Hidaka H, Kuriyama S, Yano H, Tsuji I, Kobayashi T (2011). "Precipitating factors in the pathogenesis of peritonsillar abscess and bacteriological significance of the Streptococcus milleri group". Eur J Clin Microbiol Infect Dis. 30 (4): 527–32. doi:10.1007/s10096-010-1114-9. PMID 21086007.
- ↑ Costales-Marcos M, López-Álvarez F, Núñez-Batalla F, Moreno-Galindo C, Alvarez Marcos C, Llorente-Pendás JL (2012). "[Peritonsillar infections: prospective study of 100 consecutive cases]". Acta Otorrinolaringol Esp. 63 (3): 212–7. doi:10.1016/j.otorri.2012.01.001. PMID 22425204.
- ↑ Lehnerdt G, Senska K, Fischer M, Jahnke K (2005). "[Smoking promotes the formation of peritonsillar abscesses]". Laryngorhinootologie. 84 (9): 676–9. doi:10.1055/s-2005-870289. PMID 16142623.
- ↑ Dilkes MG, Dilkes JE, Ghufoor K (1992). "Smoking and quinsy". Lancet. 339 (8808): 1552. PMID 1351238.
- ↑ 54.0 54.1 Coughlin AM, Baugh RF, Pine HS (2014). "Lingual tonsil abscess with parapharyngeal extension: a case report". Ear Nose Throat J. 93 (9): E7–8. PMID 25255362.
- ↑ 55.0 55.1 Deeva YV (2015). "[SURGICAL TREATMENT OF TONSILLAR NECK PHLEGMON]". Klin Khir (7): 47–8. PMID 26591220.
- ↑ Goldenberg D, Golz A, Joachims HZ (1997). "Retropharyngeal abscess: a clinical review". J Laryngol Otol. 111 (6): 546–50. PMID 9231089.
- ↑ Stevens HE (1990). "Vascular complication of neck space infection: case report and literature review". J Otolaryngol. 19 (3): 206–10. PMID 2355414.
- ↑ Greinwald JH, Wilson JF, Haggerty PG (1995). "Peritonsillar abscess: an unlikely cause of necrotizing fasciitis". Ann Otol Rhinol Laryngol. 104 (2): 133–7. doi:10.1177/000348949510400209. PMID 7857015.
- ↑ Wenig BL, Shikowitz MJ, Abramson AL (1984). "Necrotizing fasciitis as a lethal complication of peritonsillar abscess". Laryngoscope. 94 (12 Pt 1): 1576–9. PMID 6594557.
- ↑ Powell J, Wilson JA (2012). "An evidence-based review of peritonsillar abscess". Clin Otolaryngol. 37 (2): 136–45. doi:10.1111/j.1749-4486.2012.02452.x. PMID 22321140.
- ↑ 61.0 61.1 Apostolopoulos NJ, Nikolopoulos TP, Bairamis TN (1995). "Peritonsillar abscess in children. Is incision and drainage an effective management?". Int J Pediatr Otorhinolaryngol. 31 (2–3): 129–35. PMID 7782170.
- ↑ Johnson RF, Stewart MG, Wright CC (2003). "An evidence-based review of the treatment of peritonsillar abscess". Otolaryngol Head Neck Surg. 128 (3): 332–43. doi:10.1067/mhn.2003.93. PMID 12646835.
- ↑ Herzon FS (1995). "Harris P. Mosher Award thesis. Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines". Laryngoscope. 105 (8 Pt 3 Suppl 74): 1–17. PMID 7630308.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Nwe TT, Singh B (2000). "Management of pain in peritonsillar abscess". J Laryngol Otol. 114 (10): 765–7. PMID 11127146.
- ↑ 67.0 67.1 DescriptionEnglish: A right sided peritonsilar abscess Date 13 May 2011 Source Own work Author James Heilman,MD wikimedia commons https://commons.wikimedia.org/wiki/File:PeritonsilarAbsess.jpg
- ↑ Costantino TG, Satz WA, Dehnkamp W, Goett H (2012). "Randomized trial comparing intraoral ultrasound to landmark-based needle aspiration in patients with suspected peritonsillar abscess". Acad Emerg Med. 19 (6): 626–31. doi:10.1111/j.1553-2712.2012.01380.x. PMID 22687177.
- ↑ Buckley AR, Moss EH, Blokmanis A (1994). "Diagnosis of peritonsillar abscess: value of intraoral sonography". AJR Am J Roentgenol. 162 (4): 961–4. doi:10.2214/ajr.162.4.8141026. PMID 8141026.
- ↑ Strong EB, Woodward PJ, Johnson LP (1995). "Intraoral ultrasound evaluation of peritonsillar abscess". Laryngoscope. 105 (8 Pt 1): 779–82. doi:10.1288/00005537-199508000-00002. PMID 7630286.
- ↑ Blaivas M, Theodoro D, Duggal S (2003). "Ultrasound-guided drainage of peritonsillar abscess by the emergency physician". Am J Emerg Med. 21 (2): 155–8. doi:10.1053/ajem.2003.50029. PMID 12671820.
- ↑ 72.0 72.1 Mathoera RB, Wever PC, van Dorsten FR, Balter SG, de Jager CP (2008). "Epiglottitis in the adult patient". Neth J Med. 66 (9): 373–7. PMID 18931398.
External links
Template:Respiratory pathology
ka:პერიტონზილური აბსცესი nl:Peritonsillair abces fi:Kurkkupaise
Physical Examination
Physical examination findings suggestive of peritonsillar abscess include the following:[1][2][3][4]
Appearance of the Patient
- They are usually acutely-ill looking.
Vital Signs
- High temperature
HEENT
- Muffled voice (also called "hot potato voice")
- Contralateral deflection of the uvula
- The tonsil is generally displaced inferiorly and medially
- Facial swelling
- Tonsillar hypertrophy with likely peritonsillar edema.
- Trismus
- Drooling
- Rancid or fetor breath
Neck
- Tenderness of anterior neck
- Tender submandibular and anterior cervical lymph nodes
Lungs
- May be in obvious respiratory distress with flaring of ala nasi, subcostal and intercostal recessions.
- Increased respiratory rate in both children and adults
- Decreased air-entry depending of degree of airway obstruction
Extremities
- Cyanosis
| Variable | Croup | Epiglottitis | Pharyngitis | Tonsilitis | Retropharyngeal abscess | |
|---|---|---|---|---|---|---|
| Presentation | Cough | ✔ | — | Sore throat, pain on swallowing, fever, headache, abdominal pain, nausea and vomiting | Sore throat, pain on swallowing, fever, headache, cough | Neck pain, stiff neck, torticollis |
| Stridor | ✔ | ✔ | ||||
| Drooling | — | ✔ | ||||
| Others are Hoarseness, Difficulty breathing, symptoms of the common cold, Runny nose, Fever | Other symptoms include difficulty breathing, fever, chills, difficulty swallowing, hoarseness of voice | |||||
| Causes | Parainfluenza virus | H. influenza type b, beta-hemolytic streptococci, Staphylococcus aureus, fungi and viruses. | Group A beta-hemolytic streptococcus. | Most common cause is viral including adenovirus, rhinovirus, influenza, coronavirus, and respiratory syncytial virus. Second most common causes are bacterial; Group A streptococcal bacteria,[5] | Polymicrobial infection. Mostly; Streptococcus pyogenes, Staphylococcus aureus and respiratory anaerobes (example; Fusobacteria, Prevotella, and Veillonella species)[6][7][8][9][10][11] | |
| Physical exams findings | Suprasternal and intercostal indrawing,[12] Inspiratory stridor[13], expiratory wheezing,[13] Sternal wall retractions[14] | Cyanosis, Cervical lymphadenopathy, Inflammed epiglottis | Inflammed pharynx with or without exudate | Fever, especially 100°F or higher.[15][16]Erythema, edema and Exudate of the tonsils.[17] cervical lymphadenopathy, Dysphonia.[18] | Child may be unable to open the mouth widely. May have enlarged
cervical lymph nodes and neck mass. | |
| Age commonly affected | Mainly 6 months and 3 years old
rarely, adolescents and adults[19] |
Used to be mostly found in
pediatric age group between 3 to 5 years, however, recent trend favors adults as most commonly affected individuals[20] with a mean age of 44.94 years. |
Mostly in children and young adults,
with 50% of cases identified between the ages of 5 to 24 years.[21] |
Primarily affects children
between 5 and 15 years old.[22] |
Mostly between 2-4 years, but can occur in other age groups.[23][24] | |
| Imaging finding | Steeple sign on neck X-ray | Thumbprint sign on neck x-ray | — | Intraoral or transcutaneous USG may show an abscess making CT scan unnecessary.[25][26][27] | On CT scan, a mass impinging on the posterior pharyngeal wall with rim enhancement is seen[28][29] | |
| Treatment | Dexamethasone and nebulised epinephrine | Airway maintenance, parenteral Cefotaxime or Ceftriaxone in combination with Vancomycin. Adjuvant therapy includes corticosteroids and racemic Epinephrine.[30][31] | Antimicrobial therapy mainly penicillin-based and analgesics. | Antimicrobial therapy mainly penicillin-based and analgesics with tonsilectomy in selected cases. | Immediate surgical drainage and antimicrobial therapy. emperic therapy involves; ampicillin-sulbactam or clindamycin. | |
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
Treatment
Treatment is, as for all abscesses, through surgical incision and drainage of the pus, thereby relieving the pain of the stretched tissues. The drainage can often be achieved in the Outpatient Department using a guarded No. 11 blade in an awake and co-operative patient. Sometimes, a needle aspiration can suffice. Antibiotics are also given to treat the infection.
Peritonsillar abscesses are widely considered one of the most painful complications, primarily the surgical draining of the abscess itself. The patient is operated on awake, surgically slicing open the tonsil and draining the abscess.
Complications
- Parapharyngeal abscess
- Extension of abscess in other deep neck spaces leading to airway compromise
- Septicaemia
Alternaria spp[32]
Rhodotorula spp [33]
Acremonium spp.[34]
Dreschlera spp[35]
Malassezia spp[36]
Scedosporium spp[37]
Arthrographis spp[38]
Blastoschizomyces (11, 12),
Paecilomyces (13, 14),
Aureobasidium (15),
Clavispora (16), Ustilago (17),
Exophiala (Wangiella) (18),
and Exserohilum (19, 20).
On the other hand, most cases of fungal CNS infections are caused by only a few important species,
The common causes of fungal meningistis may be classified into two subgroups. This inlcudes:
Primary fungal pathogens of humans
All of these may cause CNS infections. This group includes: C. neoformans (22, 23),
Coccidioides immitis (24, 25, 26),
Blastomyces dermatitidis (27, 28),
Paracoccidioides brasiliensis (29, 30),
Sporothrix schenckii (31, 32),
H. capsulatum (33, 34),
Pseudallescheria boydii (Scedosporium apiospermum) (35, 36),
dematiaceous fungi (37, 38, 39).
The second group is considered opportunists, which take advantage of significant immune defects in the host. This group includes
Candida species (40, 41, 42),
Aspergillus species (43, 44, 45),
mucormycosis (46, 47), and
Trichosporon species (48, 49).
Title:Fungal Meningitis
Author / Creator:Horan ; Perfect, Jennifer, John L. R.
Language: English
Is Part Of: Infections of the Central Nervous System
Identifier: ISBN: 978-1-4698-8366-3
Source: Gale Virtual Reference Library (GVRL)
| According to severity of the disease | |||
| Mild |
| ||
| Moderate |
| ||
| Severe |
| ||
| According to the duration of disease[39] | |||
| Acute |
| ||
| Subacute |
| ||
| Chronic |
| ||
| Recurrent |
| ||
| Variable | Empyema Thoracis | Lung abscess | Pleural effusion | Pneumonia | Lung cancer | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Presentation | Variable presentation
but may follow long standing pneumonia |
Usually has history of aspiration pneumonia, alcoholics, drug abusers, seizure disorder, have undergone recent general anesthesia, or have a nasogastric or endotracheal tube. | Usually follows pneumonia as a complication | presents with fever, pleuritc chest pain, cough | mostly asymptomatic but may
have cough productive with hemoptysis and chronic history of smoking | ||||||||||||||||
| Causes | In general any bacteria
can cause an empyema, however different bacteria are associated with different rates of empyema formation.[1] Common causes include bacteroides, fusobacterium, |
Lung abscess is commonly caused by bacterial infections and these include bacteroides, peptostreptococcus and prevotella mostly after aspiration | Common causes of transudative pleural effusion include;[1][2][3][4][5] left ventricular failure, Nephrotic syndrome, and cirrhosis, while common causes of exudative pleural effusions[6] are bacterial pneumonia and malignancy | Pneumonia can result from a variety of causes, including infection with bacteria, viruses, fungi, parasites, and chemical injury to the lungs | Direct cause of lung cancers
is DNA mutations that often result in either activation of proto-oncogenes (e.g. K-RAS) or the inactivation of tumors suppressor genes (e.g. TP53) or both. The risk of these genetic mutations may be increased following exposure to environmental components example smoking | ||||||||||||||||
| Laboratory findings | The pleural fluid typically has a low pH (<7.20),
low glucose (<60 mg/dL), and contains infectious organisms. Therefore, the diagnosis relies on the presence of pus or organisms on gram stain. A positive bacteria culture from pleural fluid is not needed to make diagnosis of empyema.[40][41] |
Raised inflammatory markers ( eg high ESR, CRP) are usual but not specific | The most widely used criteria is to differentiate between exudate and transudate using the light's criteria. Fluid is exudate when:
|
Laboratory findings are non specific example leukocytosis, sputum samples for gram staining and culture. Other tests include urine antigen test, PCR, C-reactive protein and procalcitonin | The laboratory findings are
non specific including: hypercarbia, hypoxia, and tumor cells in sputum and pleural effusion cytology. | ||||||||||||||||
| Physical examination | On examination, the following
findings may be seen:[42][43][44] Lateral chest wall swelling and tenderness, clubbing of the fingernails, dull percussion note, r educed breath sounds on the affected side of the chest, egophony, coarse crackles, increased tactile fremitus, mediastinal shift to opposite side with large empyema |
Chest examination shows features of consolidation such as localised dullness on percussion, bronchial breath sound etc.
Dental decay is common especially in alcoholics and children. Clubbing is present in one third of patients. |
Bulging of the intercostal spaces,
decreased chest expansion bronchovesicular breath sounds of decreased intensity, egophony, dullness to percussion, decreased or absent fremitus. |
Physical examination increased respiratory rate, low oxygen saturation, difficulty breathing, bronchial breathe sounds, increased tactile fremitus crackling sounds, or increased whispered pectoriloquy. | Physical examination findings are non specific and may include decreased/absent breath sounds, pallor, low-grade fever, tachypnea and cachezia. | ||||||||||||||||
| CXR | Chest X ray of empyema shows air-fluid level continuos homogenous pattern from the mediastinum to the chest wall forming obtuse angle with the lung parenchyma.[45] |
Chest xray shows often unilateral cavity containing an air-fluid level and consolidation of lung parenchyema. |
A homogenous opacification is noted at the affected side. The costophrenic angle is obliterated with a meniscus. | CXR shows areas of diffused opacities. | CXR may show lung mass, widening of the mediastinum, atelectasis, or pleural effusion. | ||||||||||||||||
| Chest ultrasound | Ultrasound in empyema is positive
for suspended microbubble sign, air fluid level, curtains sign and loss of gliding sign.[46] |
Ultrasound in lung abscess is negative for suspended microbubble sign, curtains sign and loss of gliding sign but air fluid level may be seen,.[47] | Ultrasonography is helpful in making diagnosis of pleural effusion particularly in differentiating effusion from masses.[48] The extended thoracic spine sign on sonography has high sensitivity and specificity for diagnosing pleural effusion.[49] Chest or upper abdominal ultrasound may show subpulmonic effusion as shown below.[50][51][52] | Not reqiured unless complicated with empyema | USG is helpful in guiding biopsy, staging and estimating prognosis. It may show hypo- and hyperechogenic masses.[53][54][55] | ||||||||||||||||
| CT scan | Seen as a lung mass whose cavity
is regular with smooth and regular lumen, well-defined boundary and shape changes with change in patient's position.[56] Mass may resolve on antibiotics The split pleura sign is present[57] (most reliable sign to differentiate empyema from lung abscess)[58] |
Lung mass whose cavity is rregular with undulated lumen, irregular-poorly defined boundary and shape does not change with change in patient's position.[59] Mass may resolve on antibiotics | In most cases CT imaging may not provide additional information that would influence the clinical decision-making process.[60][61] [62] CT scan shows heterogeneous opacification of the affected side and cardiomediastinal shift to the opposite site in unilateral effusion.[63] |
|
Seen as a spiculated irregular solid mass that does not resolve on antibiotics | ||||||||||||||||
|
|
|||||||||||||||||||||
- ↑ Galioto NJ (2008). "Peritonsillar abscess". Am Fam Physician. 77 (2): 199–202. PMID 18246890.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Passy V (1994). "Pathogenesis of peritonsillar abscess". Laryngoscope. 104 (2): 185–90. doi:10.1288/00005537-199402000-00011. PMID 8302122.
- ↑ Nwe TT, Singh B (2000). "Management of pain in peritonsillar abscess". J Laryngol Otol. 114 (10): 765–7. PMID 11127146.
- ↑ Putto A (1987). "Febrile exudative tonsillitis: viral or streptococcal?". Pediatrics. 80 (1): 6–12. PMID 3601520.
- ↑ Cheng J, Elden L (2013). "Children with deep space neck infections: our experience with 178 children". Otolaryngol Head Neck Surg. 148 (6): 1037–42. doi:10.1177/0194599813482292. PMID 23520072.
- ↑ Abdel-Haq N, Quezada M, Asmar BI (2012). "Retropharyngeal abscess in children: the rising incidence of methicillin-resistant Staphylococcus aureus". Pediatr Infect Dis J. 31 (7): 696–9. doi:10.1097/INF.0b013e318256fff0. PMID 22481424.
- ↑ Inman JC, Rowe M, Ghostine M, Fleck T (2008). "Pediatric neck abscesses: changing organisms and empiric therapies". Laryngoscope. 118 (12): 2111–4. doi:10.1097/MLG.0b013e318182a4fb. PMID 18948832.
- ↑ Brook I (2004). "Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses". J Oral Maxillofac Surg. 62 (12): 1545–50. PMID 15573356.
- ↑ Wright CT, Stocks RM, Armstrong DL, Arnold SR, Gould HJ (2008). "Pediatric mediastinitis as a complication of methicillin-resistant Staphylococcus aureus retropharyngeal abscess". Arch Otolaryngol Head Neck Surg. 134 (4): 408–13. doi:10.1001/archotol.134.4.408. PMID 18427007.
- ↑ Asmar BI (1990). "Bacteriology of retropharyngeal abscess in children". Pediatr Infect Dis J. 9 (8): 595–7. PMID 2235179.
- ↑ Johnson D (2009). "Croup". BMJ Clin Evid. 2009. PMC 2907784. PMID 19445760.
- ↑ 13.0 13.1 Cherry, James D. (2008). "Croup". New England Journal of Medicine. 358 (4): 384–391. doi:10.1056/NEJMcp072022. ISSN 0028-4793.
- ↑ Johnson D (2009). "Croup". BMJ Clin Evid. 2009. PMC 2907784. PMID 19445760.
- ↑ Tonsillitis. Medline Plus. https://www.nlm.nih.gov/medlineplus/ency/article/001043.htm. Accessed May 2nd, 2016.
- ↑ "Tonsillitis - NHS Choices".
- ↑ Stelter K (2014). "Tonsillitis and sore throat in children". GMS Curr Top Otorhinolaryngol Head Neck Surg. 13: Doc07. doi:10.3205/cto000110. PMC 4273168. PMID 25587367.
- ↑ "Tonsillitis - Symptoms - NHS Choices".
- ↑ Tong MC, Chu MC, Leighton SE, van Hasselt CA (1996). "Adult croup". Chest. 109 (6): 1659–62. PMID 8769531.
- ↑ Lichtor JL, Roche Rodriguez M, Aaronson NL, Spock T, Goodman TR, Baum ED (2016). "Epiglottitis: It Hasn't Gone Away". Anesthesiology. 124 (6): 1404–7. doi:10.1097/ALN.0000000000001125. PMID 27031010.
- ↑ Bennett, John (2015). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1455748013.
- ↑ Sharav, Yair; Benoliel, Rafael (2008). Orofacial Pain and Headache. Elsevier. ISBN 0723434123.
- ↑ Craig FW, Schunk JE (2003). "Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management". Pediatrics. 111 (6 Pt 1): 1394–8. PMID 12777558.
- ↑ Coulthard M, Isaacs D (1991). "Neonatal retropharyngeal abscess". Pediatr Infect Dis J. 10 (7): 547–9. PMID 1876473.
- ↑ Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H; et al. (2016). "Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy". Auris Nasus Larynx. 43 (2): 182–6. doi:10.1016/j.anl.2015.09.014. PMID 26527518.
- ↑ Nogan S, Jandali D, Cipolla M, DeSilva B (2015). "The use of ultrasound imaging in evaluation of peritonsillar infections". Laryngoscope. 125 (11): 2604–7. doi:10.1002/lary.25313. PMID 25946659.
- ↑ Fordham MT, Rock AN, Bandarkar A, Preciado D, Levy M, Cohen J; et al. (2015). "Transcervical ultrasonography in the diagnosis of pediatric peritonsillar abscess". Laryngoscope. 125 (12): 2799–804. doi:10.1002/lary.25354. PMID 25945805.
- ↑ Philpott CM, Selvadurai D, Banerjee AR (2004). "Paediatric retropharyngeal abscess". J Laryngol Otol. 118 (12): 919–26. PMID 15667676.
- ↑ Vural C, Gungor A, Comerci S (2003). "Accuracy of computerized tomography in deep neck infections in the pediatric population". Am J Otolaryngol. 24 (3): 143–8. PMID 12761699.
- ↑ Nickas BJ (2005). "A 60-year-old man with stridor, drooling, and "tripoding" following a nasal polypectomy". J Emerg Nurs. 31 (3): 234–5, quiz 321. doi:10.1016/j.jen.2004.10.015. PMID 15983574.
- ↑ Wick F, Ballmer PE, Haller A (2002). "Acute epiglottis in adults". Swiss Med Wkly. 132 (37–38): 541–7. PMID 12557859.
- ↑ OHASHI Y (1960). "On a rare disease due to Alternaria tenuis Nees (alternariasis)". Tohoku J Exp Med. 72: 78–82. PMID 13730495.
- ↑ Shinde RS, Mantur BG, Patil G, Parande MV, Parande AM (2008). "Meningitis due to Rhodotorula glutinis in an HIV infected patient". Indian J Med Microbiol. 26 (4): 375–7. PMID 18974495.
- ↑ Fincher RM, Fisher JF, Lovell RD, Newman CL, Espinel-Ingroff A, Shadomy HJ (1991). "Infection due to the fungus Acremonium (cephalosporium)". Medicine (Baltimore). 70 (6): 398–409. PMID 1956281.
- ↑ Fuste FJ, Ajello L, Threlkeld R, Henry JE (1973). "Drechslera hawaiiensis: causative agent of a fatal fungal meningo-encephalitis". Sabouraudia. 11 (1): 59–63. PMID 4739938.
- ↑ Rosales CM, Jackson MA, Zwick D (2004). "Malassezia furfur meningitis associated with total parenteral nutrition subdural effusion". Pediatr Dev Pathol. 7 (1): 86–90. doi:10.1007/s10024-003-4030-5. PMID 15255040.
- ↑ Symoens F, Knoop C, Schrooyen M, Denis O, Estenne M, Nolard N; et al. (2006). "Disseminated Scedosporium apiospermum infection in a cystic fibrosis patient after double-lung transplantation". J Heart Lung Transplant. 25 (5): 603–7. doi:10.1016/j.healun.2005.12.011. PMID 16678041.
- ↑ Chin-Hong PV, Sutton DA, Roemer M, Jacobson MA, Aberg JA (2001). "Invasive fungal sinusitis and meningitis due to Arthrographis kalrae in a patient with AIDS". J Clin Microbiol. 39 (2): 804–7. doi:10.1128/JCM.39.2.804-807.2001. PMC 87827. PMID 11158158.
- ↑ Zheng H, Chen Q, Xie Z, Wang D, Li M, Zhang X; et al. (2016). "A retrospective research of HIV-negative cryptococcal meningoencephalitis patients with acute/subacute onset". Eur J Clin Microbiol Infect Dis. 35 (2): 299–303. doi:10.1007/s10096-015-2545-0. PMID 26792138.
- ↑ Mavroudis C, Ganzel BL, Cox SK, Polk HC (1987). "Experimental aerobic-anaerobic thoracic empyema in the guinea pig". Ann Thorac Surg. 43 (3): 298–302. PMID 3548615.
- ↑ Perez VP, Caierão J, Fischer GB, Dias CA, d'Azevedo PA (2016). "Pleural effusion with negative culture: a challenge for pneumococcal diagnosis in children". Diagn Microbiol Infect Dis. 86 (2): 200–4. doi:10.1016/j.diagmicrobio.2016.07.022. PMID 27527890.
- ↑ Atay S, Banki F, Floyd C (2016). "Empyema necessitans caused by actinomycosis: A case report". Int J Surg Case Rep. 23: 182–5. doi:10.1016/j.ijscr.2016.04.005. PMC 5022073. PMID 27180228.
- ↑ Gomes MM, Alves M, Correia JB, Santos L (2013). "Empyema necessitans: very late complication of pulmonary tuberculosis". BMJ Case Rep. 2013. doi:10.1136/bcr-2013-202072. PMC 3863066. PMID 24326441.
- ↑ Kuan YC, How SH, Yeen WC, Ng TH, Fauzi AR (2011). "Empyema thoracis complicated by pneumothorax necessitans manifesting as lobulated, localized subcutaneous emphysematous swellings". Ann Thorac Surg. 91 (6): 1969–71. doi:10.1016/j.athoracsur.2010.11.075. PMID 21619994.
- ↑ Moffett BK, Panchabhai TS, Nakamatsu R, Arnold FW, Peyrani P, Wiemken T; et al. (2016). "Comparing posteroanterior with lateral and anteroposterior chest radiography in the initial detection of parapneumonic effusions". Am J Emerg Med. 34 (12): 2402–2407. doi:10.1016/j.ajem.2016.09.021. PMID 27793503.
- ↑ Lin FC, Chou CW, Chang SC (2004). "Differentiating pyopneumothorax and peripheral lung abscess: chest ultrasonography". Am J Med Sci. 327 (6): 330–5. PMID 15201646.
- ↑ Lin FC, Chou CW, Chang SC (2004). "Differentiating pyopneumothorax and peripheral lung abscess: chest ultrasonography". Am J Med Sci. 327 (6): 330–5. PMID 15201646.
- ↑
- ↑ Dickman E, Terentiev V, Likourezos A, Derman A, Haines L (2015). "Extension of the Thoracic Spine Sign: A New Sonographic Marker of Pleural Effusion". J Ultrasound Med. 34 (9): 1555–61. doi:10.7863/ultra.15.14.06013. PMID 26269297.
- ↑ Almeida FA, Eiger G (2008). "Subpulmonic effusion". Intern Med J. 38 (3): 216–7. doi:10.1111/j.1445-5994.2007.01619.x. PMID 18290818.
- ↑ Connell DG, Crothers G, Cooperberg PL (1982). "The subpulmonic pleural effusion: sonographic aspects". J Can Assoc Radiol. 33 (2): 101–3. PMID 7107669.
- ↑ Halvorsen RA, Thompson WM (1986). "Ascites or pleural effusion? CT and ultrasound differentiation". Crit Rev Diagn Imaging. 26 (3): 201–40. PMID 3536306.
- ↑ Mroz RM, Korniluk M, Swidzinska E, Dzieciol J, Czaban J, Panek B; et al. (2010). "Lung mass in a 28-year-old male: a case report of a rare tumor". Eur J Med Res. 15 Suppl 2: 95–7. PMC 4360372. PMID 21147631.
- ↑ Torun E, Fidan A, Cağlayan B, Salepçi T, Mayadağli A, Salepçi B (2008). "[Prognostic factors in small cell lung cancer]". Tuberk Toraks. 56 (1): 22–9. PMID 18330751.
- ↑ Filon E, Kodur E, Cygan M (1989). "[Ultrasonographic examination of the adrenal glands for detection of lung cancer metastasis]". Nowotwory. 39 (3–4): 157–61. PMID 2700089.
- ↑ Baber CE, Hedlund LW, Oddson TA, Putman CE (1980). "Differentiating empyemas and peripheral pulmonary abscesses: the value of computed tomography". Radiology. 135 (3): 755–8. doi:10.1148/radiology.135.3.7384467. PMID 7384467.
- ↑ Stark DD, Federle MP, Goodman PC, Podrasky AE, Webb WR (1983). "Differentiating lung abscess and empyema: radiography and computed tomography". AJR Am J Roentgenol. 141 (1): 163–7. doi:10.2214/ajr.141.1.163. PMID 6602513.
- ↑ Kraus GJ (2007). "The split pleura sign". Radiology. 243 (1): 297–8. doi:10.1148/radiol.2431041658. PMID 17392263.
- ↑ Baber CE, Hedlund LW, Oddson TA, Putman CE (1980). "Differentiating empyemas and peripheral pulmonary abscesses: the value of computed tomography". Radiology. 135 (3): 755–8. doi:10.1148/radiology.135.3.7384467. PMID 7384467.
- ↑ Corcoran JP, Acton L, Ahmed A, Hallifax RJ, Psallidas I, Wrightson JM; et al. (2016). "Diagnostic value of radiological imaging pre- and post-drainage of pleural effusions". Respirology. 21 (2): 392–5. doi:10.1111/resp.12675. PMID 26545413.
- ↑ Federle MP, Mark AS, Guillaumin ES (1986). "CT of subpulmonic pleural effusions and atelectasis: criteria for differentiation from subphrenic fluid". AJR Am J Roentgenol. 146 (4): 685–9. doi:10.2214/ajr.146.4.685. PMID 3485341.
- ↑ Halvorsen RA, Thompson WM (1986). "Ascites or pleural effusion? CT and ultrasound differentiation". Crit Rev Diagn Imaging. 26 (3): 201–40. PMID 3536306.
- ↑ Wolverson MK, Crepps LF, Sundaram M, Heiberg E, Vas WG, Shields JB (1983). "Hyperdensity of recent hemorrhage at body computed tomography: incidence and morphologic variation". Radiology. 148 (3): 779–84. doi:10.1148/radiology.148.3.6878700. PMID 6878700.