Sandbox/01: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Infobox Disease | |||
| Name = Rickets | |||
| ICD10 = {{ICD10|E|55| |e|50}} | |||
| ICD9 = {{ICD9|268}} | |||
| Image = Rickets USNLM.gif | |||
| Caption = A family with rickets. Paris, 1900. | |||
| DiseasesDB = 9351 | |||
| MedlinePlus = 000344 | |||
| MeshName = Rickets | |||
| MeshNumber = D012279 | |||
}} | |||
{{SI}} | |||
{{CMG}} | {{CMG}} | ||
==Overview== | |||
'''Rickets''' is a softening of the bones in children potentially leading to fractures and deformity. Rickets is among the most frequent childhood diseases in many developing countries. The predominant cause is a [[vitamin D]] deficiency, but lack of adequate [[calcium]] in the diet may also lead to rickets. Although it can occur in adults, the majority of cases occur in children suffering from severe [[malnutrition]], usually resulting from [[famine]] or [[starvation]] during the early stages of childhood. | |||
[[Osteomalacia]] is the term used to describe a similar condition occurring in adults, generally due to a deficiency of vitamin D. | |||
The origin of the word "rickets" is unknown. The Greek derived word "rachitis" (meaning "inflammation of the spine") was later adopted as the scientific term for rickets, due chiefly to the words' similarity in sound. | |||
==Epidemiology== | |||
[[Image:Rickets wrist.jpg|thumb|left|"rachitis" The "wrist widening" of rickets]] | |||
Those at higher risk for developing rickets include: | |||
*Breast-fed infants whose mothers are not exposed to sunlight | |||
*Breast-fed infants who are not exposed to sunlight | |||
*Individuals not consuming fortified milk, such as those who are [[lactose intolerant]] | |||
Individuals with red hair have a decreased risk for rickets due to their greater production of vitamin D in sunlight.<ref>[http://www.derm.med.ed.ac.uk/06_teaching/redhairgen.htm Red hair and genetics]</ref> | |||
==Etiology== | |||
Vitamin D is required for proper calcium absorption from the gut. In the absence of vitamin D, dietary calcium is not properly absorbed, resulting in [[hypocalcemia]], leading to skeletal and dental deformities and [[neuromuscular]] symptoms, e.g. hyperexcitability. | |||
A rare [[X-linked dominant]] form exists called [[X-linked hypophosphatemia|Vitamin D resistant rickets]]. | |||
==Presentation== | |||
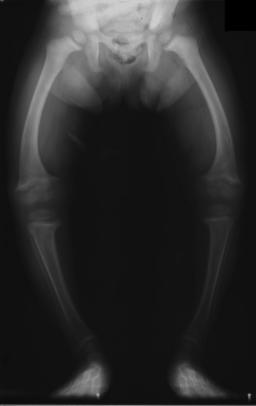
[[Image:XrayRicketsLegssmall.jpg|thumb|left|[[Radiograph]] of a two-year old rickets sufferer, with a marked [[genu varum]] (bowing of the [[femur]]s) and decreased bone [[opacity]], suggesting poor [[bone mineralization]].|right]] | |||
Signs and symptoms of rickets include: | |||
*Bone pain or tenderness | |||
*[[tooth|dental]] problems | |||
*[[muscle]] weakness (rickety myopathy or "floppy baby syndrome") | |||
*increased tendency for [[fracture]]s (easily broken bones), especially [[greenstick fracture]]s | |||
*Skeletal deformity | |||
**Toddlers: Bowed legs ([[genu varum]]) | |||
**Older children: Knock-knees ([[genu valgum]]) or "windswept knees" | |||
**Cranial, spinal, and pelvic deformities | |||
*Growth disturbance | |||
*[[Hypocalcemia]] (low level of calcium in the blood), and | |||
*[[Tetany (medical sign)|Tetany]] (uncontrolled muscle spasms all over the body). | |||
*[[Craniotabes]] (soft skull) | |||
*[[Costochondral]] swelling (aka "[[rickety rosary]]" or "[[rachitic rosary]]") | |||
*[[Harrison's groove]] | |||
*Double malleoli sign due to metaphyseal hyperplasia [http://medicalpics.blogspot.com/2007/04/double-malleoli-sign-of-rickets.html] | |||
An [[X-ray]] or [[radiography|radiograph]] of an advanced sufferer from rickets tends to present in a classic way: bow legs (outward curve of long bone of the legs) and a deformed chest. Changes in the skull also occur causing a distinctive "square headed" appearance. These deformities persist into adult life if not treated. | |||
Long-term consequences include permanent bends or disfiguration of the long bones, and a [[Scoliosis|curved back]]. | |||
==Diagnosis== | |||
A doctor may diagnose rickets by: | |||
*Blood tests: | |||
**Serum [[calcium]] may show low levels of calcium, serum [[phosphorus]] may be low, and serum [[alkaline phosphatase]] may be high. | |||
*[[Arterial blood gas]]es may reveal [[metabolic acidosis]] | |||
*[[X-ray]]s of affected bones may show loss of calcium from bones or changes in the shape or structure of the bones. | |||
*Bone biopsy is rarely performed but will confirm rickets. | |||
'''Patient #1: Radiographs of the knee in a patient with rickets''' | |||
<gallery> | |||
Image:Rickets-001.jpg | |||
Image:Rickets-002.jpg | |||
</gallery> | |||
'''Patient #2: Radiographs of the knee in a patient with rickets''' | |||
<gallery> | |||
Image: | |||
Rickets-201.jpg | |||
Image: | |||
Rickets-202.jpg | |||
</gallery> | |||
'''Patient #3: Radiograph of the chest in a patient with rickets''' | |||
<gallery> | |||
Image: | |||
Rickets-301.jpg | |||
</gallery> | |||
==Ricketts: Microscopical Findings== | |||
{{#ev:youtube|y7iA0_jkOTI}} | |||
==Treatment and prevention== | |||
===Diet and sunlight=== | |||
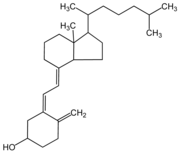
[[Image:Cholecalciferol.png|thumb|left|[[Cholecalciferol]] (D3)]] | |||
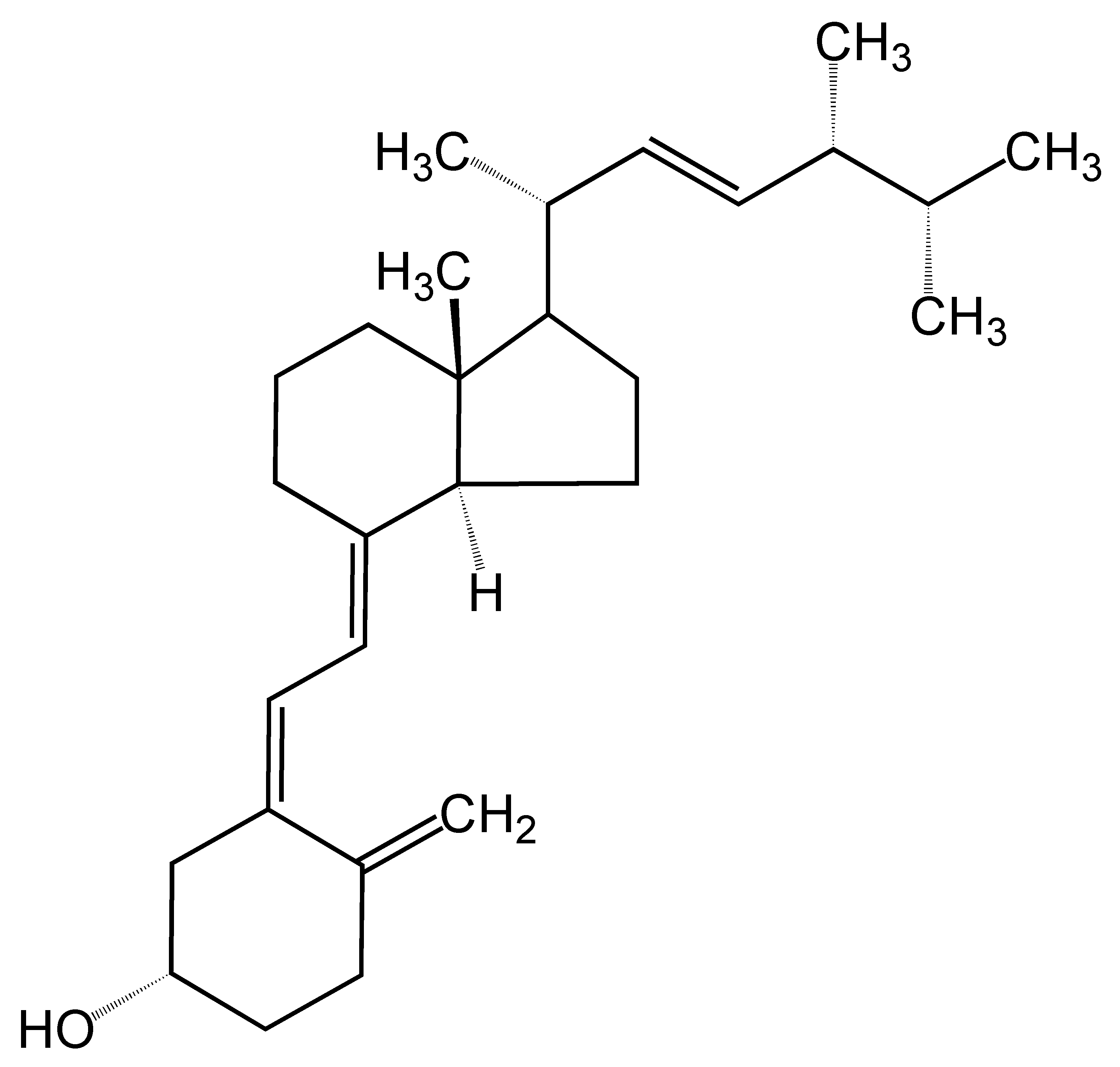
[[Image:Ergocalciferol.png|thumb|left|[[Ergocalciferol]] (D2)]] | |||
Treatment involves increasing dietary intake of calcium, phosphates and vitamin D. Exposure to ultraviolet light (sunshine), [[cod liver oil]], halibut-liver oil, and [[Ergosterol|viosterol]] are all sources of vitamin D. | |||
A sufficient amount of ultraviolet in sunlight each day and adequate supplies of calcium and phosphorus in the diet can prevent rickets. Darker-skinned babies need to be exposed longer to the [[ultraviolet|ultraviolet rays]]. The replacement of vitamin D has been proven to correct rickets using these methods of [http://pediatrics.aappublications.org/cgi/content/full/112/2/e132 ultraviolet light therapy]and medicine. | |||
Recommendations are for 200 [[international unit]]s (IU) of vitamin D a day for infants and children. Children who do not get adequate amounts of vitamin D are at increased risk of rickets. Vitamin D is essential for allowing the body to uptake calcium for use in proper bone calcification and maintenance. | |||
=== | ===Supplementation=== | ||
Sufficient vitamin D levels can also be achieved through dietary supplementation. Vitamin D3 ([[cholecalciferol]]) is the preferred form since it is more readily absorbed than vitamin D2. Most [[dermatology|dermatologists]] recommend vitamin D supplementation as an alternative to unprotected ultraviolet exposure due to the increased risk of skin cancer associated with sun exposure. | |||
According to the [[American Academy of Pediatrics]] (AAP), infants who are breast-fed may not get enough vitamin D from breast milk alone. For this reason, the AAP recommends that infants who are exclusively breast-fed receive daily supplements of vitamin D from age 2 months until they start drinking at least 17 ounces of vitamin D-fortified milk or formula a day [http://aappolicy.aappublications.org/cgi/content/full/pediatrics;111/4/908]. This requirement for supplemental vitamin D is not a defect in the evolution of human breastmilk but is instead a result of the modern-day infant's decreased exposure to sunlight. | |||
==References== | == References == | ||
{{reflist|2}} | {{reflist|2}} | ||
<references/> | |||
== External links == | |||
*[http://aappolicy.aappublications.org/cgi/content/full/pediatrics;111/4/908 AAP Recommendations on Vitamin D Supplementation] | |||
*[http://courses.washington.edu/bonephys/hypercalU/opmal2.html Dr. Susan Ott's website on osteomalacia] | |||
*[http://www.healthvitaminsguide.com/deficiencies/rickets.htm Rickets - Symptoms, Causes, Treatment] | |||
*[http://dictionary.reference.com/search?q=osteomalacia Dictionary.com - Osteomalacia] | |||
*[http://www.fluoridealert.org/health/bone/fluorosis/osteomalacia.html Fluoride & Osteomalacia] | |||
*[http://www.beyonddiscovery.org/content/view.txt.asp?a=414 History of Vitamin D and the battle against Rickets] | |||
* {{Chorus|00906}} | |||
{{Nutritional pathology}} | {{Nutritional pathology}} | ||
[[Category:Malnutrition]] | |||
[[Category:Pediatrics]] | |||
[[Category:Skeletal disorders]] | |||
[[Category:Gastroenterology]] | [[Category:Gastroenterology]] | ||
[[de:Rachitis]] | |||
[[es:Raquitismo]] | |||
[[fi:Riisitauti]] | |||
[[fr:Rachitisme]] | |||
[[ko:구루병]] | |||
[[it:Rachitismo]] | |||
[[ja:くる病]] | |||
[[nl:Rachitis]] | |||
[[no:Rakitt]] | |||
[[pl:Krzywica]] | |||
[[pt:Raquitismo]] | |||
[[ru:Рахит]] | |||
[[simple:Rickets]] | |||
[[sv:Rakitis]] | |||
[[tr:Raşitizm]] | |||
[[zh:佝僂病]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Revision as of 14:29, 3 June 2016
| Rickets | ||
 | ||
|---|---|---|
| A family with rickets. Paris, 1900. | ||
| ICD-10 | E55 | |
| ICD-9 | 268 | |
| DiseasesDB | 9351 | |
| MedlinePlus | 000344 | |
| MeSH | D012279 | |
|
WikiDoc Resources for Sandbox/01 |
|
Articles |
|---|
|
Most recent articles on Sandbox/01 |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sandbox/01 at Clinical Trials.gov Clinical Trials on Sandbox/01 at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox/01
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox/01 Discussion groups on Sandbox/01 Patient Handouts on Sandbox/01 Directions to Hospitals Treating Sandbox/01 Risk calculators and risk factors for Sandbox/01
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox/01 |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Rickets is a softening of the bones in children potentially leading to fractures and deformity. Rickets is among the most frequent childhood diseases in many developing countries. The predominant cause is a vitamin D deficiency, but lack of adequate calcium in the diet may also lead to rickets. Although it can occur in adults, the majority of cases occur in children suffering from severe malnutrition, usually resulting from famine or starvation during the early stages of childhood. Osteomalacia is the term used to describe a similar condition occurring in adults, generally due to a deficiency of vitamin D. The origin of the word "rickets" is unknown. The Greek derived word "rachitis" (meaning "inflammation of the spine") was later adopted as the scientific term for rickets, due chiefly to the words' similarity in sound.
Epidemiology

Those at higher risk for developing rickets include:
- Breast-fed infants whose mothers are not exposed to sunlight
- Breast-fed infants who are not exposed to sunlight
- Individuals not consuming fortified milk, such as those who are lactose intolerant
Individuals with red hair have a decreased risk for rickets due to their greater production of vitamin D in sunlight.[1]
Etiology
Vitamin D is required for proper calcium absorption from the gut. In the absence of vitamin D, dietary calcium is not properly absorbed, resulting in hypocalcemia, leading to skeletal and dental deformities and neuromuscular symptoms, e.g. hyperexcitability.
A rare X-linked dominant form exists called Vitamin D resistant rickets.
Presentation
Signs and symptoms of rickets include:
- Bone pain or tenderness
- dental problems
- muscle weakness (rickety myopathy or "floppy baby syndrome")
- increased tendency for fractures (easily broken bones), especially greenstick fractures
- Skeletal deformity
- Toddlers: Bowed legs (genu varum)
- Older children: Knock-knees (genu valgum) or "windswept knees"
- Cranial, spinal, and pelvic deformities
- Growth disturbance
- Hypocalcemia (low level of calcium in the blood), and
- Tetany (uncontrolled muscle spasms all over the body).
- Craniotabes (soft skull)
- Costochondral swelling (aka "rickety rosary" or "rachitic rosary")
- Harrison's groove
- Double malleoli sign due to metaphyseal hyperplasia [2]
An X-ray or radiograph of an advanced sufferer from rickets tends to present in a classic way: bow legs (outward curve of long bone of the legs) and a deformed chest. Changes in the skull also occur causing a distinctive "square headed" appearance. These deformities persist into adult life if not treated.
Long-term consequences include permanent bends or disfiguration of the long bones, and a curved back.
Diagnosis
A doctor may diagnose rickets by:
- Blood tests:
- Serum calcium may show low levels of calcium, serum phosphorus may be low, and serum alkaline phosphatase may be high.
- Arterial blood gases may reveal metabolic acidosis
- X-rays of affected bones may show loss of calcium from bones or changes in the shape or structure of the bones.
- Bone biopsy is rarely performed but will confirm rickets.
Patient #1: Radiographs of the knee in a patient with rickets
Patient #2: Radiographs of the knee in a patient with rickets
Patient #3: Radiograph of the chest in a patient with rickets
Ricketts: Microscopical Findings
{{#ev:youtube|y7iA0_jkOTI}}
Treatment and prevention
Diet and sunlight
Treatment involves increasing dietary intake of calcium, phosphates and vitamin D. Exposure to ultraviolet light (sunshine), cod liver oil, halibut-liver oil, and viosterol are all sources of vitamin D.
A sufficient amount of ultraviolet in sunlight each day and adequate supplies of calcium and phosphorus in the diet can prevent rickets. Darker-skinned babies need to be exposed longer to the ultraviolet rays. The replacement of vitamin D has been proven to correct rickets using these methods of ultraviolet light therapyand medicine.
Recommendations are for 200 international units (IU) of vitamin D a day for infants and children. Children who do not get adequate amounts of vitamin D are at increased risk of rickets. Vitamin D is essential for allowing the body to uptake calcium for use in proper bone calcification and maintenance.
Supplementation
Sufficient vitamin D levels can also be achieved through dietary supplementation. Vitamin D3 (cholecalciferol) is the preferred form since it is more readily absorbed than vitamin D2. Most dermatologists recommend vitamin D supplementation as an alternative to unprotected ultraviolet exposure due to the increased risk of skin cancer associated with sun exposure.
According to the American Academy of Pediatrics (AAP), infants who are breast-fed may not get enough vitamin D from breast milk alone. For this reason, the AAP recommends that infants who are exclusively breast-fed receive daily supplements of vitamin D from age 2 months until they start drinking at least 17 ounces of vitamin D-fortified milk or formula a day [3]. This requirement for supplemental vitamin D is not a defect in the evolution of human breastmilk but is instead a result of the modern-day infant's decreased exposure to sunlight.
References
External links
- AAP Recommendations on Vitamin D Supplementation
- Dr. Susan Ott's website on osteomalacia
- Rickets - Symptoms, Causes, Treatment
- Dictionary.com - Osteomalacia
- Fluoride & Osteomalacia
- History of Vitamin D and the battle against Rickets
- Template:Chorus
Template:Nutritional pathology
de:Rachitis fi:Riisitauti ko:구루병 it:Rachitismo nl:Rachitis no:Rakitt simple:Rickets sv:Rakitis




