ST elevation myocardial infarction primary percutaneous coronary intervention
| Myocardial infarction | |
 | |
|---|---|
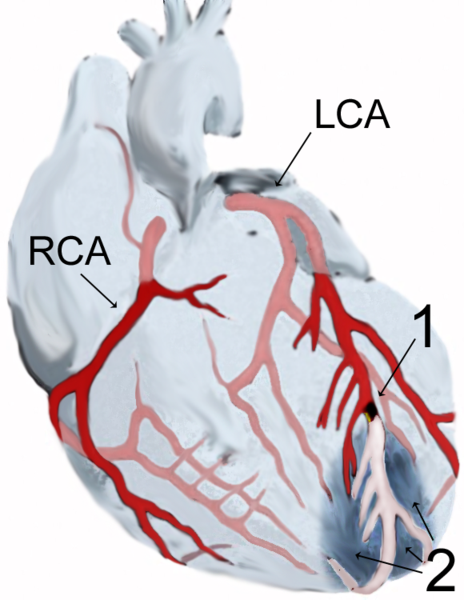
| Diagram of a myocardial infarction (2) of the tip of the anterior wall of the heart (an apical infarct) after occlusion (1) of a branch of the left coronary artery (LCA, right coronary artery = RCA). | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
| Cardiology Network |
 Discuss ST elevation myocardial infarction primary percutaneous coronary intervention further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Vijayalakshmi Kunadian MBBS MD MRCP [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Definitions
Primary PCI
Primary PCI is defined as the performance of percutaneous coronary intervention (PCI) (either conventional balloon angioplasty or coronary stent placement) in the setting of ST elevation MI (STEMI) without antecedent treatment with a fibrinolytic agent. The chapter on Primary PCI can be found here. Primary PCI is the subject of this chapter.
Facilitated PCI
Facilitated PCI is defined as the intent to perform a PCI (either conventional balloon angioplasty or coronary stent placement) in the setting of STEMI following treatment with either a full dose or half dose of a fibrinolytic agent. This approach is also termed a pharmaco-invasive strategy. This strategy differs from rescue or adjunctive PCI in that the intent of facilitated PCI is to perform PCI, and the administration of a fibrinolytic agent is intended to improve the PCI results. The chapter on Facilitated PCI can be found here.
Rescue PCI
Rescue PCI is defined as the intent to administer a fibrinolytic agent in the setting of STEMI, and the performance of PCI for failure of the fibrinolytic agents is unintended. If there are clinical signs and symptoms of failure of the fibrinolytic agent to achieve reperfusion, then rescue PCI is performed to open the totally occluded artery. The strategy differs from facilitated PCI in that the intent is to administer a fibrinolytic agent, and the performance of PCI is intended to improve the fibrinolytic results. The chapter on Rescue PCI can be found here.
Adjunctive PCI
Adjunctive PCI is defined as the intent to administer fibrinolytic agent in the setting of STEMI, and the performance of PCI for partial success of the fibrinolytic agent is unintended. If there are clinical signs and symptoms of incomplete reperfusion, then adjunctive PCI is performed to further open a patent artery (one with TIMI grade 2 or 3 flow). The strategy differs from facilitated PCI in that the intent is to administer a fibrinolytic agent, and the performance of PCI is intended to improve the fibrinolytic results.
Normal 0 false false false EN-US X-NONE X-NONE MicrosoftInternetExplorer4
Primary Percutaneous coronary intervention
Abbreviations and acronyms
ADMIRAL Abciximab before Direct Angioplasty and Stenting in Myocardial Infarction Regarding Acute and Long-term follow-up
ASPV Average systolic peak velocity
C-PORT Cardiovascular Patients Outcomes Research Team
DANAMI Danish Multicenter Randomized study on fibrinolytic therapy versus Acute Coronary Angioplasty in Acute Myocardial Infarction
DSE Dobutamine stress echocardiography
EMERALD Enhanced Myocardial Efficacy and Recovery by Aspiration of Liberated Debris
FTT Fibrinolysis Therapy Trialists
GUSTO Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes
IC Intracoronary
ICH Intracranial hemorrhage
LVEF Left ventricular ejection fraction
MBG Myocardial blush grade
MCE Myocardial contrast echocardiography
NRMI National Registry of Myocardial Infarction
OAT Occluded artery trial
PAMI Primary angioplasty in Acute Myocardial Infarction
PASSION Paclitaxel-Eluting Stent versus Conventional Stent in Myocardial Infarction with ST-Segment Elevation
PRAGUE PRimary Angioplasty in patients transferred from General community hospitals to specialized PTCA Units with or without Emergency fibrinolysis
PTCA Percutaneous transluminal coronary angioplasty
PCI Percutaneous coronary intervention
PPCI Primary percutaneous coronary intervention
RAPPORT Reopro And Primary PTCA Organization and Randomized Trial
RIKS-HIA Register of Information and Knowledge about Swedish Heart Intensive care Admissions
SESAMI Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction
SK Streptokinase
STRATEGY Single High Dose Bolus Tirofiban and Sirolimus Eluting Stent vs. Abciximab and Bare Metal Stent in Myocardial Infarction study
STEMI ST elevation myocardial infarction
STOP-AMI Stent versus Fibrinolysis for Occluded coronary arteries in patients with Acute Myocardial Infarction
TAPAS Thrombus Aspiration in Percutaneous coronary intervention following Acute myocardial infarction Study.
TFG TIMI flow grade
TIMI Thrombolysis in Myocardial Infarction
TMPG TIMI myocardial perfusion grade
TPA Tissue plasminogen activator
TVR Target vessel revascularization
TYPHOON Trial to assess the use of the cYPHer stent in acute myocardial infarction treated with ballOON angioplasty
Introduction
In 1976, Davies and co-workers in a series of 500 autopsy specimens identified plaque rupture and coronary thrombosis which led to coronary artery occlusion as the cause of acute myocardial infarction ADDIN REFMGR.CITE <Refman><Author>Davies</Author><Year>1976</Year><RecNum>1776</RecNum><IDText>Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1776</Ref_ID><Title_Primary>Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi</Title_Primary><Authors_Primary>Davies,M.J.</Authors_Primary><Authors_Primary>Woolf,N.</Authors_Primary><Authors_Primary>Robertson,W.B.</Authors_Primary><Date_Primary>1976/7</Date_Primary><Keywords>Acute Disease</Keywords><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Arteries</Keywords><Keywords>Autopsy</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>Female</Keywords><Keywords>Heart Ventricles</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Necrosis</Keywords><Keywords>pathology</Keywords><Keywords>Perfusion</Keywords><Keywords>Thrombosis</Keywords><Reprint>Not in File</Reprint><Start_Page>659</Start_Page><End_Page>664</End_Page><Periodical>Br.Heart J.</Periodical><Volume>38</Volume><Issue>7</Issue><Web_URL>PM:973888</Web_URL><ZZ_JournalStdAbbrev><f name="System">Br.Heart J.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[1]. Briefly, coronary artery occlusion results in chest pain and electrocardiographic changes in the leads corresponding to the infarcted segments. Necrosis of the myocardium ensues starting from the endocardium to the epicardium eventually resulting in transmural infarct depending on the duration of occlusion ADDIN REFMGR.CITE <Refman><Author>Reimer</Author><Year>1977</Year><RecNum>1777</RecNum><IDText>The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1777</Ref_ID><Title_Primary>The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs</Title_Primary><Authors_Primary>Reimer,K.A.</Authors_Primary><Authors_Primary>Lowe,J.E.</Authors_Primary><Authors_Primary>Rasmussen,M.M.</Authors_Primary><Authors_Primary>Jennings,R.B.</Authors_Primary><Date_Primary>1977/11</Date_Primary><Keywords>Animals</Keywords><Keywords>Cell Survival</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>Disease Models,Animal</Keywords><Keywords>Dogs</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Endocardium</Keywords><Keywords>Hemodynamics</Keywords><Keywords>Hemorrhage</Keywords><Keywords>injuries</Keywords><Keywords>Ischemia</Keywords><Keywords>Ligation</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Necrosis</Keywords><Keywords>Papillary Muscles</Keywords><Keywords>pathology</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Time Factors</Keywords><Reprint>Not in File</Reprint><Start_Page>786</Start_Page><End_Page>794</End_Page><Periodical>Circulation</Periodical><Volume>56</Volume><Issue>5</Issue><Web_URL>PM:912839</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[2].
Since the introduction of pharmacologic reperfusion therapies in the seventies, the main goal of reperfusion treatment has been to restore early, full and sustained patency of the infarct related arteries. In the seventies and in the eighties, fibrinolytic therapy has been the primary reperfusion therapy that was available for the management of patients with acute ST elevation myocardial infarction (STEMI). An initial analysis consisting of 9 clinical trials by the Fibrinolysis Therapy Trialists (FTT) group demonstrated that there was a significant reduction in the mortality with the use of fibrinolytic therapy compared to control subjects who did not receive fibrinolysis (9.6% vs. 11.5%, p<0.00001) ADDIN REFMGR.CITE <Refman><Year>1994</Year><RecNum>1778</RecNum><IDText>Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1778</Ref_ID><Title_Primary>Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group</Title_Primary><Date_Primary>1994/2/5</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Anistreplase</Keywords><Keywords>blood</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Bundle-Branch Block</Keywords><Keywords>contraindications</Keywords><Keywords>drug therapy</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Heart Rate</Keywords><Keywords>history</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Morbidity</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies as Topic</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Odds Ratio</Keywords><Keywords>Plasminogen</Keywords><Keywords>Pressure</Keywords><Keywords>Randomized Controlled Trials as Topic</Keywords><Keywords>Research</Keywords><Keywords>Shock</Keywords><Keywords>statistics & numerical data</Keywords><Keywords>Streptokinase</Keywords><Keywords>Stroke</Keywords><Keywords>Survival</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Urinary Plasminogen Activator</Keywords><Reprint>Not in File</Reprint><Start_Page>311</Start_Page><End_Page>322</End_Page><Periodical>Lancet</Periodical><Volume>343</Volume><Issue>8893</Issue><Web_URL>PM:7905143</Web_URL><ZZ_JournalStdAbbrev><f name="System">Lancet</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[3].
Subsequently with the introduction of percutaneous transluminal coronary angioplasty (PTCA), patients who were treated with fibrinolytic therapy underwent coronary angiography and PTCA was performed for persistent occlusion of the coronary arteries. As a result, initial studies compared the outcome of patients who were treated with fibrinolytic therapy with those who had fibrinolytic therapy and subsequently underwent PTCA. Theses initial studies did not demonstrate significant benefit between the two groups ADDIN REFMGR.CITE <Refman><Author>Topol</Author><Year>1987</Year><RecNum>373</RecNum><IDText>A randomized trial of immediate versus delayed elective angioplasty after intravenous tissue plasminogen activator in acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>373</Ref_ID><Title_Primary>A randomized trial of immediate versus delayed elective angioplasty after intravenous tissue plasminogen activator in acute myocardial infarction</Title_Primary><Authors_Primary>Topol,E.J.</Authors_Primary><Authors_Primary>Califf,R.M.</Authors_Primary><Authors_Primary>George,B.S.</Authors_Primary><Authors_Primary>Kereiakes,D.J.</Authors_Primary><Authors_Primary>Abbottsmith,C.W.</Authors_Primary><Authors_Primary>Candela,R.J.</Authors_Primary><Authors_Primary>Lee,K.L.</Authors_Primary><Authors_Primary>Pitt,B.</Authors_Primary><Authors_Primary>Stack,R.S.</Authors_Primary><Authors_Primary>O'Neill,W.W.</Authors_Primary><Date_Primary>1987/9/3</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Balloon</Keywords><Keywords>Arteries</Keywords><Keywords>Clinical Trials</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Emergencies</Keywords><Keywords>Female</Keywords><Keywords>Heart Catheterization</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Injections,Intravenous</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Random Allocation</Keywords><Keywords>Research Support,Non-U.S.Gov't</Keywords><Keywords>Stroke Volume</Keywords><Keywords>surgery</Keywords><Keywords>therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Ventricular Function</Keywords><Reprint>Not in File</Reprint><Start_Page>581</Start_Page><End_Page>588</End_Page><Periodical>N Engl J Med</Periodical><Volume>317</Volume><Issue>10</Issue><Web_URL>PM:2956516</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Simoons</Author><Year>1988</Year><RecNum>1910</RecNum><IDText>Thrombolysis with tissue plasminogen activator in acute myocardial infarction: no additional benefit from immediate percutaneous coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1910</Ref_ID><Title_Primary>Thrombolysis with tissue plasminogen activator in acute myocardial infarction: no additional benefit from immediate percutaneous coronary angioplasty</Title_Primary><Authors_Primary>Simoons,M.L.</Authors_Primary><Authors_Primary>Arnold,A.E.</Authors_Primary><Authors_Primary>Betriu,A.</Authors_Primary><Authors_Primary>de Bono,D.P.</Authors_Primary><Authors_Primary>Col,J.</Authors_Primary><Authors_Primary>Dougherty,F.C.</Authors_Primary><Authors_Primary>von,Essen R.</Authors_Primary><Authors_Primary>Lambertz,H.</Authors_Primary><Authors_Primary>Lubsen,J.</Authors_Primary><Authors_Primary>Meier,B.</Authors_Primary><Authors_Primary>.</Authors_Primary><Date_Primary>1988/1/30</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Balloon</Keywords><Keywords>Aspirin</Keywords><Keywords>Clinical Trials as Topic</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Comparative Study</Keywords><Keywords>complications</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Drug Therapy,Combination</Keywords><Keywords>Europe</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Heparin</Keywords><Keywords>Humans</Keywords><Keywords>Hypotension</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Infusions,Intravenous</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Plasminogen</Keywords><Keywords>Proteins</Keywords><Keywords>Random Allocation</Keywords><Keywords>Recombinant Proteins</Keywords><Keywords>Recurrence</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Ventricular Fibrillation</Keywords><Reprint>Not in File</Reprint><Start_Page>197</Start_Page><End_Page>203</End_Page><Periodical>Lancet</Periodical><Volume>1</Volume><Issue>8579</Issue><Web_URL>PM:2893037</Web_URL><ZZ_JournalStdAbbrev><f name="System">Lancet</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[4;5]. Hence a strategy of primary PTCA alone for patients with acute STEMI was adopted and this strategy offered significant advantage in terms of reduction in mortality, non-fatal reinfarction and intracranial hemorrhage compared to patients who received fibrinolytic therapy.
Since the introduction of primary PTCA, significant advances have been made in the field of interventional cardiology with the availability of intra-coronary stents, advanced pharmacotherapy including potent antiplatelet and antithrombin agents. Studies using intra-coronary stents and potent antiplatelet agents such as glycoprotein IIb/IIIa inhibitors have demonstrated significant mortality reduction, reduction in non-fatal reinfarction and stroke. Primary PCI indeed is now the favored treatment strategy for the management of patients with acute STEMI in places where it is feasible to provide this treatment.
Limitations of fibrinolytic therapy
Contraindications to fibrinolysis
Although the use of fibrinolytic therapy was associated with significant reduction in mortality, it was soon demonstrated to be overcome by a number of limitations. An analysis from the TIMI-9 registry demonstrated that 10.3% of patients have contraindications to fibrinolysis which consisted of prior stroke or transient ischemic attack, recent cardiopulmonary resuscitation, trauma, surgery, recent bleeding, persistent hypertension and significant illness ADDIN REFMGR.CITE <Refman><Author>Cannon</Author><Year>2002</Year><RecNum>1915</RecNum><IDText>Under-utilization of evidence based medications in acute ST elevation myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI 9) registry</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1915</Ref_ID><Title_Primary>Under-utilization of evidence based medications in acute ST elevation myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI 9) registry</Title_Primary><Authors_Primary>Cannon,C.P.</Authors_Primary><Authors_Primary>Bahit,MC</Authors_Primary><Authors_Primary>Haugland,J.M.</Authors_Primary><Authors_Primary>Henry,T.D.</Authors_Primary><Authors_Primary>Schweiger,M.J.</Authors_Primary><Authors_Primary>McKendall,GR</Authors_Primary><Authors_Primary>Shah,P.K.</Authors_Primary><Authors_Primary>Murphy,S.A.</Authors_Primary><Authors_Primary>Gibson,C.Michael</Authors_Primary><Authors_Primary>McCabe,C.H.</Authors_Primary><Authors_Primary>Antman,E.</Authors_Primary><Authors_Primary>Braunwald,E</Authors_Primary><Date_Primary>2002</Date_Primary><Keywords>Myocardial Infarction</Keywords><Keywords>Infarction</Keywords><Keywords>Registries</Keywords><Reprint>Not in File</Reprint><Start_Page>44</Start_Page><End_Page>52</End_Page><Periodical>Crit Pathways Cardiol</Periodical><Volume>1</Volume><ZZ_JournalFull><f name="System">Crit Pathways Cardiol</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[6]. Its efficacy in the management of patients with cardiogenic shock complicating acute STEMI is not proven. In addition, not all patients who are treated with fibrinolysis undergo coronary angiography. This results in patients with significant coronary stenosis or three vessel disease not receiving the appropriate revascularization therapy.
Timing of fibrinolytic treatment
The benefit of fibrinolytic therapy decreases as time progresses after the onset of symptoms. Pre-hospital administration of fibrinolysis was beneficial if administered within 70 minutes in terms reduction in the composite score of death, stroke, serious bleed and infarct size (p=0.009) ADDIN REFMGR.CITE <Refman><Author>Weaver</Author><Year>1993</Year><RecNum>1912</RecNum><IDText>Prehospital-initiated vs hospital-initiated thrombolytic therapy. The Myocardial Infarction Triage and Intervention Trial</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1912</Ref_ID><Title_Primary>Prehospital-initiated vs hospital-initiated thrombolytic therapy. The Myocardial Infarction Triage and Intervention Trial</Title_Primary><Authors_Primary>Weaver,W.D.</Authors_Primary><Authors_Primary>Cerqueira,M.</Authors_Primary><Authors_Primary>Hallstrom,A.P.</Authors_Primary><Authors_Primary>Litwin,P.E.</Authors_Primary><Authors_Primary>Martin,J.S.</Authors_Primary><Authors_Primary>Kudenchuk,P.J.</Authors_Primary><Authors_Primary>Eisenberg,M.</Authors_Primary><Date_Primary>1993/9/8</Date_Primary><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Aspirin</Keywords><Keywords>Chest Pain</Keywords><Keywords>Comparative Study</Keywords><Keywords>complications</Keywords><Keywords>diagnosis</Keywords><Keywords>drug therapy</Keywords><Keywords>Emergency Medical Services</Keywords><Keywords>Emergency Service,Hospital</Keywords><Keywords>Female</Keywords><Keywords>Gated Blood-Pool Imaging</Keywords><Keywords>Heparin</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Outcome and Process Assessment (Health Care)</Keywords><Keywords>Pain</Keywords><Keywords>physiopathology</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>standards</Keywords><Keywords>statistics & numerical data</Keywords><Keywords>Stroke</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Time Factors</Keywords><Keywords>Triage</Keywords><Keywords>Washington</Keywords><Reprint>Not in File</Reprint><Start_Page>1211</Start_Page><End_Page>1216</End_Page><Periodical>JAMA</Periodical><Volume>270</Volume><Issue>10</Issue><Address>Department of Medicine, University of Washington School of Medicine, Seattle</Address><Web_URL>PM:8355383</Web_URL><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[7]. Further studies suggest that significant mortality reduction is seen in patients treated with fibrinolytic therapy within the first 2 hours of symptom onset compared to those presenting later ADDIN REFMGR.CITE <Refman><Author>Boersma</Author><Year>1996</Year><RecNum>1911</RecNum><IDText>Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1911</Ref_ID><Title_Primary>Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour</Title_Primary><Authors_Primary>Boersma,E.</Authors_Primary><Authors_Primary>Maas,A.C.</Authors_Primary><Authors_Primary>Deckers,J.W.</Authors_Primary><Authors_Primary>Simoons,M.L.</Authors_Primary><Date_Primary>1996/9/21</Date_Primary><Keywords>Animals</Keywords><Keywords>Clinical Trials</Keywords><Keywords>drug therapy</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>methods</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Netherlands</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Time Factors</Keywords><Reprint>Not in File</Reprint><Start_Page>771</Start_Page><End_Page>775</End_Page><Periodical>Lancet</Periodical><Volume>348</Volume><Issue>9030</Issue><Address>Erasmus University, Rotterdam, Netherlands</Address><Web_URL>PM:8813982</Web_URL><ZZ_JournalStdAbbrev><f name="System">Lancet</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[8].
Cerebrovascular events
Stroke remains a catastrophic complication of fibrinolytic therapy. The FTT collaborators analysis demonstrated that fibrinolysis was associated with an increase in stroke rates compared to control patients (1.2% vs. 0.8%, p<0.00001) ADDIN REFMGR.CITE <Refman><Year>1994</Year><RecNum>1778</RecNum><IDText>Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1778</Ref_ID><Title_Primary>Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group</Title_Primary><Date_Primary>1994/2/5</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Anistreplase</Keywords><Keywords>blood</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Bundle-Branch Block</Keywords><Keywords>contraindications</Keywords><Keywords>drug therapy</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Heart Rate</Keywords><Keywords>history</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Morbidity</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies as Topic</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Odds Ratio</Keywords><Keywords>Plasminogen</Keywords><Keywords>Pressure</Keywords><Keywords>Randomized Controlled Trials as Topic</Keywords><Keywords>Research</Keywords><Keywords>Shock</Keywords><Keywords>statistics & numerical data</Keywords><Keywords>Streptokinase</Keywords><Keywords>Stroke</Keywords><Keywords>Survival</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Urinary Plasminogen Activator</Keywords><Reprint>Not in File</Reprint><Start_Page>311</Start_Page><End_Page>322</End_Page><Periodical>Lancet</Periodical><Volume>343</Volume><Issue>8893</Issue><Web_URL>PM:7905143</Web_URL><ZZ_JournalStdAbbrev><f name="System">Lancet</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[3]. An analysis from the GUSTO I (Global Use of Strategies to Open Occluded arteries in Acute Coronary Syndromes) study demonstrated that the overall incidence of stroke after fibrinolytic therapy was 1.4% (95% of stroke occurred within 5 days). Combination treatment with streptokinase (SK) and tissue plasminogen activator (TPA) was associated with significantly more stroke than SK alone (1.64% vs. 1.19%, p<0.007). Of these in 41% of cases the stroke was fatal. Intracranial hemorrhage (ICH) occurred in 0.46% of cases who received SK and 0.88% of cases who received combination therapy (p<0.001) ADDIN REFMGR.CITE <Refman><Author>Gore</Author><Year>1995</Year><RecNum>1775</RecNum><IDText>Stroke after thrombolysis. Mortality and functional outcomes in the GUSTO-I trial. Global Use of Strategies to Open Occluded Coronary Arteries</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1775</Ref_ID><Title_Primary>Stroke after thrombolysis. Mortality and functional outcomes in the GUSTO-I trial. Global Use of Strategies to Open Occluded Coronary Arteries</Title_Primary><Authors_Primary>Gore,J.M.</Authors_Primary><Authors_Primary>Granger,C.B.</Authors_Primary><Authors_Primary>Simoons,M.L.</Authors_Primary><Authors_Primary>Sloan,M.A.</Authors_Primary><Authors_Primary>Weaver,W.D.</Authors_Primary><Authors_Primary>White,H.D.</Authors_Primary><Authors_Primary>Barbash,G.I.</Authors_Primary><Authors_Primary>Van de,Werf F.</Authors_Primary><Authors_Primary>Aylward,P.E.</Authors_Primary><Authors_Primary>Topol,E.J.</Authors_Primary><Authors_Primary>.</Authors_Primary><Date_Primary>1995/11/15</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>adverse effects</Keywords><Keywords>Aged</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Cerebral Hemorrhage</Keywords><Keywords>Cerebral Infarction</Keywords><Keywords>chemically induced</Keywords><Keywords>Comparative Study</Keywords><Keywords>Disability Evaluation</Keywords><Keywords>drug therapy</Keywords><Keywords>Drug Therapy,Combination</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Hemorrhage</Keywords><Keywords>Heparin</Keywords><Keywords>Humans</Keywords><Keywords>Hypertension</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Logistic Models</Keywords><Keywords>Male</Keywords><Keywords>Massachusetts</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Plasminogen</Keywords><Keywords>Pressure</Keywords><Keywords>Prognosis</Keywords><Keywords>psychology</Keywords><Keywords>Quality of Life</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>Streptokinase</Keywords><Keywords>Stroke</Keywords><Keywords>Survivors</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Reprint>Not in File</Reprint><Start_Page>2811</Start_Page><End_Page>2818</End_Page><Periodical>Circulation</Periodical><Volume>92</Volume><Issue>10</Issue><Address>University of Massachusetts Medical Center, Worcester, USA</Address><Web_URL>PM:7586246</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[9]. Another analysis demonstrated a slight increase in ICH among patients receiving TPA (0.95%) ADDIN REFMGR.CITE <Refman><Author>Gurwitz</Author><Year>1998</Year><RecNum>1913</RecNum><IDText>Risk for intracranial hemorrhage after tissue plasminogen activator treatment for acute myocardial infarction. Participants in the National Registry of Myocardial Infarction 2</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1913</Ref_ID><Title_Primary>Risk for intracranial hemorrhage after tissue plasminogen activator treatment for acute myocardial infarction. Participants in the National Registry of Myocardial Infarction 2</Title_Primary><Authors_Primary>Gurwitz,J.H.</Authors_Primary><Authors_Primary>Gore,J.M.</Authors_Primary><Authors_Primary>Goldberg,R.J.</Authors_Primary><Authors_Primary>Barron,H.V.</Authors_Primary><Authors_Primary>Breen,T.</Authors_Primary><Authors_Primary>Rundle,A.C.</Authors_Primary><Authors_Primary>Sloan,M.A.</Authors_Primary><Authors_Primary>French,W.</Authors_Primary><Authors_Primary>Rogers,W.J.</Authors_Primary><Date_Primary>1998/10/15</Date_Primary><Keywords>adverse effects</Keywords><Keywords>Age Factors</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>blood</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Body Weight</Keywords><Keywords>Cerebral Hemorrhage</Keywords><Keywords>Cerebrovascular Disorders</Keywords><Keywords>chemically induced</Keywords><Keywords>complications</Keywords><Keywords>diagnosis</Keywords><Keywords>Female</Keywords><Keywords>Hemorrhage</Keywords><Keywords>history</Keywords><Keywords>Hospitalization</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Logistic Models</Keywords><Keywords>Magnetic Resonance Imaging</Keywords><Keywords>Male</Keywords><Keywords>Massachusetts</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Plasminogen</Keywords><Keywords>Pressure</Keywords><Keywords>Registries</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>Stroke</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Tomography,X-Ray Computed</Keywords><Reprint>Not in File</Reprint><Start_Page>597</Start_Page><End_Page>604</End_Page><Periodical>Ann.Intern.Med.</Periodical><Volume>129</Volume><Issue>8</Issue><Address>University of Massachusetts Medical School and the Fallon Healthcare System, Worcester 01608, USA</Address><Web_URL>PM:9786806</Web_URL><ZZ_JournalStdAbbrev><f name="System">Ann.Intern.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[10].
Patency of infarct arteries
In addition to the above limitations, early patency of the infarct related arteries is not demonstrated in all patients treated with fibrinolytic therapy. Angiography following fibrinolytic therapy demonstrates that TIMI flow grade 3 is achieved in only ~40-60% of cases. In an analysis from the GUSTO trial, the patency of infarct artery (TIMI flow grade 2/3) at 90 minutes was achieved in 81% of cases in the accelerated TPA group compared to only 54% in the SK group (p<0.001). Normal flow (TFG 3) was achieved in 54% of patients who received TPA compared to 40% among those who received the other treatments (SK + subcutaneous heparin, SK + intravenous heparin, combination SK, TPA and heparin) ADDIN REFMGR.CITE <Refman><Year>1993</Year><RecNum>368</RecNum><IDText>The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>368</Ref_ID><Title_Primary>The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators</Title_Primary><Date_Primary>1993/11/25</Date_Primary><Keywords>Angiography</Keywords><Keywords>Arteries</Keywords><Keywords>Cineangiography</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Drug Therapy,Combination</Keywords><Keywords>Female</Keywords><Keywords>Heparin</Keywords><Keywords>Humans</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Research Support,Non-U.S.Gov't</Keywords><Keywords>Streptokinase</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Vascular Patency</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1615</Start_Page><End_Page>1622</End_Page><Periodical>N Engl J Med</Periodical><Volume>329</Volume><Issue>22</Issue><Web_URL>PM:8232430</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[11]. The mortality at 30 days was significantly increased among those who had reduced flow compared to those who had normal flow (8.9% vs. 4.4%, p=0.009).
Reinfarction and recurrent ischemia
Fibrinolysis is also overcome by frequent occurrence of recurrent ischemia, reocclusion of the infarct artery (reocclusion within 5-7 days occurred in 4.9-6.4% cases in the GUSTO analysis) and reinfarction. Reinfarction occurred in 4.3% of cases following thrombolysis at a median of 3.8 days after fibrinolysis. The 30-day mortality was increased among those who had reinfarction compared to those who did not have reinfarction (11.3% vs. 3.5%, p<0.001). The mortality from 30 days to one year was also significantly increased among those who had reinfarction (4.7% vs. 3.2%, p<0.001) ADDIN REFMGR.CITE <Refman><Author>Hudson</Author><Year>2001</Year><RecNum>1914</RecNum><IDText>Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1914</Ref_ID><Title_Primary>Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials</Title_Primary><Authors_Primary>Hudson,M.P.</Authors_Primary><Authors_Primary>Granger,C.B.</Authors_Primary><Authors_Primary>Topol,E.J.</Authors_Primary><Authors_Primary>Pieper,K.S.</Authors_Primary><Authors_Primary>Armstrong,P.W.</Authors_Primary><Authors_Primary>Barbash,G.I.</Authors_Primary><Authors_Primary>Guerci,A.D.</Authors_Primary><Authors_Primary>Vahanian,A.</Authors_Primary><Authors_Primary>Califf,R.M.</Authors_Primary><Authors_Primary>Ohman,E.M.</Authors_Primary><Date_Primary>2001/9/11</Date_Primary><Keywords>Aged</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Clinical Trials as Topic</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Drug Therapy,Combination</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolysis</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Heart</Keywords><Keywords>Heart Rate</Keywords><Keywords>Hospitalization</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Odds Ratio</Keywords><Keywords>Plasminogen</Keywords><Keywords>Population</Keywords><Keywords>Pressure</Keywords><Keywords>Recurrence</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Smoking</Keywords><Keywords>statistics & numerical data</Keywords><Keywords>Streptokinase</Keywords><Keywords>Survival Rate</Keywords><Keywords>therapeutic use</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Time Factors</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>utilization</Keywords><Reprint>Not in File</Reprint><Start_Page>1229</Start_Page><End_Page>1235</End_Page><Periodical>Circulation</Periodical><Volume>104</Volume><Issue>11</Issue><Address>Duke Clinical Research Institute, Durham, NC, USA. mhudson1@hfhs.org</Address><Web_URL>PM:11551872</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[12].
Fibrinolysis versus PTCA
Due to the limitations associated with the fibrinolytic therapy, it became evident in small non-randomized studies that mechanical reperfusion strategy using percutaneous transluminal coronary angioplasty is associated with increased infarct artery patency and reduced mortality. This encouraged randomized trials to directly compare the benefits of primary PTCA with fibrinolytic therapy.
Clinical trials comparing primary PTCA with fibrinolysis
The initial studies compared the efficacy of intracoronary streptokinase administration with primary PTCA among patients with ST elevation myocardial infarction. O’Neill and colleagues randomized a total of 56 patients to either intracoronary streptokinase (SK) or undergo PTCA. There was no difference in the infarct artery patency rates between the two groups (85% SK vs. 83% PTCA, p=NS). However there was significant reduction in the residual stenosis with PTCA compared to fibrinolytic therapy (p<0.001), improvement in global ejection fraction (p<0.001) and regional wall motion abnormality (p=0.05) ADDIN REFMGR.CITE <Refman><Author>O'Neill</Author><Year>1986</Year><RecNum>1782</RecNum><IDText>A prospective randomized clinical trial of intracoronary streptokinase versus coronary angioplasty for acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1782</Ref_ID><Title_Primary>A prospective randomized clinical trial of intracoronary streptokinase versus coronary angioplasty for acute myocardial infarction</Title_Primary><Authors_Primary>O'Neill,W.</Authors_Primary><Authors_Primary>Timmis,G.C.</Authors_Primary><Authors_Primary>Bourdillon,P.D.</Authors_Primary><Authors_Primary>Lai,P.</Authors_Primary><Authors_Primary>Ganghadarhan,V.</Authors_Primary><Authors_Primary>Walton,J.,Jr.</Authors_Primary><Authors_Primary>Ramos,R.</Authors_Primary><Authors_Primary>Laufer,N.</Authors_Primary><Authors_Primary>Gordon,S.</Authors_Primary><Authors_Primary>Schork,M.A.</Authors_Primary><Authors_Primary>.</Authors_Primary><Date_Primary>1986/3/27</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Balloon</Keywords><Keywords>Arteries</Keywords><Keywords>Clinical Trials as Topic</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug therapy</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Infusions,Parenteral</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Contraction</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>physiopathology</Keywords><Keywords>Prospective Studies</Keywords><Keywords>radiography</Keywords><Keywords>Random Allocation</Keywords><Keywords>Reperfusion</Keywords><Keywords>Streptokinase</Keywords><Keywords>Stroke Volume</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Ventricular Function</Keywords><Reprint>Not in File</Reprint><Start_Page>812</Start_Page><End_Page>818</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>314</Volume><Issue>13</Issue><Web_URL>PM:2936956</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[13].
Clinical studies with short-term follow-up
Over the following ten years, several small and large randomized clinical studies were performed to assess the benefits of primary PTCA compared with fibrinolysis. In 1995, Michels and Yusuf performed a meta-analysis of 7 clinical trials comparing primary PTCA versus fibrinolytic therapy and 16 clinical trials comparing PTCA after fibrinolysis versus fibrinolytic therapy alone consisting of 8496 patients ADDIN REFMGR.CITE <Refman><Author>Michels</Author><Year>1995</Year><RecNum>1783</RecNum><IDText>Does PTCA in acute myocardial infarction affect mortality and reinfarction rates? A quantitative overview (meta-analysis) of the randomized clinical trials</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1783</Ref_ID><Title_Primary>Does PTCA in acute myocardial infarction affect mortality and reinfarction rates? A quantitative overview (meta-analysis) of the randomized clinical trials</Title_Primary><Authors_Primary>Michels,K.B.</Authors_Primary><Authors_Primary>Yusuf,S.</Authors_Primary><Date_Primary>1995/1/15</Date_Primary><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>classification</Keywords><Keywords>Clinical Trials</Keywords><Keywords>Comparative Study</Keywords><Keywords>Cross-Over Studies</Keywords><Keywords>epidemiology</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>methods</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Odds Ratio</Keywords><Keywords>Randomized Controlled Trials as Topic</Keywords><Keywords>Recurrence</Keywords><Keywords>Survivors</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time Factors</Keywords><Reprint>Not in File</Reprint><Start_Page>476</Start_Page><End_Page>485</End_Page><Periodical>Circulation</Periodical><Volume>91</Volume><Issue>2</Issue><Address>Department of Epidemiology, Harvard School of Public Health, Boston, Mass</Address><Web_URL>PM:7805253</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[14]. There was a significant mortality benefit with primary PTCA compared to fibrinolytic therapy at 6 weeks in addition to benefits in terms of reduction in combined short-term mortality and reinfarction. These benefits were not demonstrated among patients who underwent PTCA after fibrinolysis compared to those who had fibrinolysis alone. This latter finding discouraged PTCA following the administration of fibrinolysis.
In 1997, Weaver and colleagues performed another meta-analysis consisting of 10 single center and multi-center randomized trials consisting of 2606 patients who had primary PTCA and fibrinolytic therapy from January 1985 to March 1996. Streptokinase was used in four of these trials, tissue plasminogen activator (TPA) was used in three trials and the accelerated dose TPA was used in the remaining three trials. There was significant 30-day mortality reduction with primary PTCA (n=1290) compared to fibrinolytic therapy (n=1316) [4.4% vs. 6.5%, p=0.02]. There was also significant reduction in the combined death and reinfarction rates (7.2% vs. 11.9%, p<0.001), total stroke (0.7% vs. 2%, p=0.007) and hemorrhagic stroke rates (0.1% vs. 1.1%, p<0.001) ADDIN REFMGR.CITE <Refman><Author>Weaver</Author><Year>1997</Year><RecNum>1784</RecNum><IDText>Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1784</Ref_ID><Title_Primary>Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review</Title_Primary><Authors_Primary>Weaver,W.D.</Authors_Primary><Authors_Primary>Simes,R.J.</Authors_Primary><Authors_Primary>Betriu,A.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Authors_Primary>Zijlstra,F.</Authors_Primary><Authors_Primary>Garcia,E.</Authors_Primary><Authors_Primary>Grinfeld,L.</Authors_Primary><Authors_Primary>Gibbons,R.J.</Authors_Primary><Authors_Primary>Ribeiro,E.E.</Authors_Primary><Authors_Primary>DeWood,M.A.</Authors_Primary><Authors_Primary>Ribichini,F.</Authors_Primary><Date_Primary>1997/12/17</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cerebrovascular Disorders</Keywords><Keywords>Comparative Study</Keywords><Keywords>Confidence Intervals</Keywords><Keywords>epidemiology</Keywords><Keywords>Health Services Research</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Infusions,Intravenous</Keywords><Keywords>Logistic Models</Keywords><Keywords>methods</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Odds Ratio</Keywords><Keywords>Outcome and Process Assessment (Health Care)</Keywords><Keywords>Plasminogen</Keywords><Keywords>Plasminogen Activators</Keywords><Keywords>Randomized Controlled Trials as Topic</Keywords><Keywords>Recurrence</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Streptokinase</Keywords><Keywords>Stroke</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>United States</Keywords><Reprint>Not in File</Reprint><Start_Page>2093</Start_Page><End_Page>2098</End_Page><Periodical>JAMA</Periodical><Volume>278</Volume><Issue>23</Issue><Address>Heart and Vascular Institute, Henry Ford Health System, Detroit, MI 48202, USA. wweaver1@hfhs.org</Address><Web_URL>PM:9403425</Web_URL><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[15].
Clinical trials with long-term follow-up
Although significant benefits have been proven in the short term (4-6 weeks) using the primary PTCA strategy, one of the main limitations of these initials trials is that long term outcome results were not available. Hence subsequent studies including the GUSTO IIb, Zwolle group studies and the PAMI (Primary angioplasty in Acute Myocardial Infarction) trials provided outcome results extending up to 5 years.
GUSTO IIb study
The GUSTO IIb study (Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes) demonstrated that benefit in terms of reduction in the composite outcome of death, non fatal reinfarction and non fatal disabling stroke seen at 30 days (9.6% vs. 13.7%, p=0.033) was no longer significant at 6 months (13.3% vs. 15.7 % p=NS) with primary PTCA compared to fibrinolytic therapy using recombinant tissue plasminogen activator among 1138 patients from 57 hospitals ADDIN REFMGR.CITE <Refman><Year>1997</Year><RecNum>1785</RecNum><IDText>A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTO IIb) Angioplasty Substudy Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1785</Ref_ID><Title_Primary>A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTO IIb) Angioplasty Substudy Investigators</Title_Primary><Date_Primary>1997/6/5</Date_Primary><Keywords>Acute Coronary Syndrome</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Cerebrovascular Disorders</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Comparative Study</Keywords><Keywords>drug therapy</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Heparin</Keywords><Keywords>Hirudin Therapy</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Odds Ratio</Keywords><Keywords>Physicians</Keywords><Keywords>Plasminogen</Keywords><Keywords>Plasminogen Activators</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Recurrence</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Stroke</Keywords><Keywords>Syndrome</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>1621</Start_Page><End_Page>1628</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>336</Volume><Issue>23</Issue><Web_URL>PM:9173270</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[16]. At 30 days there was no difference in the occurrence of death (5.7% vs. 7%, p=0.37), reinfarction (4.5% vs. 6.5%, p=0.13) and stroke (0.2% vs. 0.9%, p=0.11) when analyzed independently.
PAMI trial
In the PAMI trial (Primary angioplasty in Acute Myocardial Infarction), 395 patients were randomized to undergo PTCA (n=195) and fibrinolysis using TPA (n=200) within 12 hours of acute STEMI ADDIN REFMGR.CITE <Refman><Author>Grines</Author><Year>1993</Year><RecNum>388</RecNum><IDText>A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>388</Ref_ID><Title_Primary>A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group</Title_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Authors_Primary>Browne,K.F.</Authors_Primary><Authors_Primary>Marco,J.</Authors_Primary><Authors_Primary>Rothbaum,D.</Authors_Primary><Authors_Primary>Stone,G.W.</Authors_Primary><Authors_Primary>O'Keefe,J.</Authors_Primary><Authors_Primary>Overlie,P.</Authors_Primary><Authors_Primary>Donohue,B.</Authors_Primary><Authors_Primary>Chelliah,N.</Authors_Primary><Authors_Primary>Timmis,G.C.</Authors_Primary><Authors_Primary>.</Authors_Primary><Date_Primary>1993/3/11</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Aged,80 and over</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Aspirin</Keywords><Keywords>Cerebral Hemorrhage</Keywords><Keywords>Comparative Study</Keywords><Keywords>complications</Keywords><Keywords>Coronary Artery Bypass</Keywords><Keywords>Emergencies</Keywords><Keywords>etiology</Keywords><Keywords>Exercise Test</Keywords><Keywords>Female</Keywords><Keywords>Heart Catheterization</Keywords><Keywords>Hemorrhage</Keywords><Keywords>Heparin</Keywords><Keywords>Humans</Keywords><Keywords>Injections,Intravenous</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Ischemia</Keywords><Keywords>radionuclide imaging</Keywords><Keywords>Radionuclide Ventriculography</Keywords><Keywords>Recurrence</Keywords><Keywords>Rest</Keywords><Keywords>surgery</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function</Keywords><Reprint>Not in File</Reprint><Start_Page>673</Start_Page><End_Page>679</End_Page><Periodical>N Engl J Med</Periodical><Volume>328</Volume><Issue>10</Issue><Address>William Beaumont Hospital, Royal Oak, MI 48073-6769</Address><Web_URL>PM:8433725</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[17]. In contrast to the GUSTO IIb trial results, the combined death and reinfarction rates at 6 months were significantly reduced in the PTCA group compared to the fibrinolysis group (8.5% vs. 16.8%, p=0.02) with an increase in intracranial hemorrhage with fibrinolysis compared to PTCA (2% vs. 0%, p=0.05).
Zwolle group study
The long term benefit of primary PTCA was assessed by Zijlstra and colleagues ADDIN REFMGR.CITE <Refman><Author>Zijlstra</Author><Year>1999</Year><RecNum>415</RecNum><IDText>Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>415</Ref_ID><Title_Primary>Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction</Title_Primary><Authors_Primary>Zijlstra,F.</Authors_Primary><Authors_Primary>Hoorntje,J.C.</Authors_Primary><Authors_Primary>de Boer,M.J.</Authors_Primary><Authors_Primary>Reiffers,S.</Authors_Primary><Authors_Primary>Miedema,K.</Authors_Primary><Authors_Primary>Ottervanger,J.P.</Authors_Primary><Authors_Primary>van't Hof,A.W.</Authors_Primary><Authors_Primary>Suryapranata,H.</Authors_Primary><Date_Primary>1999/11/4</Date_Primary><Keywords>Analysis of Variance</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Cause of Death</Keywords><Keywords>Comparative Study</Keywords><Keywords>drug therapy</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart</Keywords><Keywords>Hospital Charges</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Recurrence</Keywords><Keywords>Research Support,Non-U.S.Gov't</Keywords><Keywords>Risk</Keywords><Keywords>Streptokinase</Keywords><Keywords>Survival Analysis</Keywords><Keywords>Survival Rate</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Reprint>Not in File</Reprint><Start_Page>1413</Start_Page><End_Page>1419</End_Page><Periodical>N Engl J Med</Periodical><Volume>341</Volume><Issue>19</Issue><Address>Department of Cardiology, Hospital De Weezenlanden, Zwolle, The Netherlands. v.derks@diagram-zwolle.nl</Address><Web_URL>PM:10547403</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[18]. There were 395 STEMI patients who underwent primary PTCA and 201 patients who underwent fibrinolysis. Follow-up results were obtained for 5±2 years in this study. There was once again mortality benefit at 30 days using the primary PTCA strategy compared to fibrinolysis alone (1% vs. 7%, p=0.01) which extended to 5±2 years (13.4% vs. 23.9%, p=0.01). There was also significant difference in the occurrence of combined death and non-fatal reinfarction at 30 days (relative risk 0.13, 95% confidence interval 0.05-0.37) and beyond 30 days (relative risk 0.62, 95% confidence interval 0.43-0.91) with primary PTCA. This study also demonstrated that the estimated cost including initial hospital stay charges, readmission charges, procedural charges, physician charges and medications charges were significantly lower with primary PTCA compared to fibrinolytic therapy ($16090 vs. $16813, p=0.05). Although performed at a later time period than the GUSTO and the PAMI trials, one of the limitations with this study is that intracoronary stents and glycoprotein IIb/IIIa inhibitors were not used.
Meta-analysis of primary angioplasty vs. fibrinolysis
In a meta-analysis in 2003, Keeley and colleagues studied 23 trials of acute myocardial infarction consisting of a total of 7739 patients. Of these, 3867 patients were assigned to fibrinolysis and 3872 were assigned to primary PTCA. Most patients who received fibrinolytic therapy received a fibrin-specific agent (76%). Stents were used in 12 trials and platelet glycoprotein IIb/IIIa inhibitors were used in eight trials. Similar to the previous studies on fibrinolysis versus primary PTCA, this study demonstrated that primary PTCA was better than fibrinolytic therapy in terms of reduction in the overall short-term (4-6 weeks) death (7% vs. 9%; p=0.0002), death excluding the SHOCK trial data (5% vs. 7%; p=0.0003), non-fatal reinfarction (3% vs. 7%; p<0.0001), and stroke (1% vs. 2%; p=0.0004). The combined endpoint of death, non-fatal reinfarction and stroke was significantly reduced in the primary PTCA group (8% vs. 14%; p<0.0001). The benefit of primary PTCA over fibrinolytic therapy was not only seen in the short term but also in the long term (6-18 months) regardless of the type of fibrinolytic agents used and whether or not patients were transferred to another center for primary PTCA ADDIN REFMGR.CITE <Refman><Author>Keeley</Author><Year>2003</Year><RecNum>1755</RecNum><IDText>Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1755</Ref_ID><Title_Primary>Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials</Title_Primary><Authors_Primary>Keeley,E.C.</Authors_Primary><Authors_Primary>Boura,J.A.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Date_Primary>2003/1/4</Date_Primary><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>drug therapy</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>methods</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Randomized Controlled Trials as Topic</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Shock</Keywords><Keywords>Stents</Keywords><Keywords>Streptokinase</Keywords><Keywords>Stroke</Keywords><Keywords>Texas</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Work</Keywords><Reprint>Not in File</Reprint><Start_Page>13</Start_Page><End_Page>20</End_Page><Periodical>Lancet</Periodical><Volume>361</Volume><Issue>9351</Issue><Address>Department of Internal Medicine, Division of Cardiology, University of Texas Southwestern Medical Center, Dallas, TX, USA. Ellen.Keeley@UTSoutherwestern.edu</Address><Web_URL>PM:12517460</Web_URL><ZZ_JournalStdAbbrev><f name="System">Lancet</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[19].
The issue of reinfarction following primary PTCA was specifically addressed by Kernis and colleagues in an analysis from the PAMI trials ADDIN REFMGR.CITE <Refman><Author>Kernis</Author><Year>2003</Year><RecNum>2542</RecNum><IDText>The incidence, predictors, and outcomes of early reinfarction after primary angioplasty for acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2542</Ref_ID><Title_Primary>The incidence, predictors, and outcomes of early reinfarction after primary angioplasty for acute myocardial infarction</Title_Primary><Authors_Primary>Kernis,S.J.</Authors_Primary><Authors_Primary>Harjai,K.J.</Authors_Primary><Authors_Primary>Stone,G.W.</Authors_Primary><Authors_Primary>Grines,L.L.</Authors_Primary><Authors_Primary>Boura,J.A.</Authors_Primary><Authors_Primary>Yerkey,M.W.</Authors_Primary><Authors_Primary>O'Neill,W.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Date_Primary>2003/10/1</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Stenosis</Keywords><Keywords>Death</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Hospitalization</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Michigan</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>New York City</Keywords><Keywords>Odds Ratio</Keywords><Keywords>pathology</Keywords><Keywords>Prognosis</Keywords><Keywords>radiography</Keywords><Keywords>Recurrence</Keywords><Keywords>Risk Factors</Keywords><Keywords>Severity of Illness Index</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Dysfunction,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1173</Start_Page><End_Page>1177</End_Page><Periodical>J.Am.Coll.Cardiol</Periodical><Volume>42</Volume><Issue>7</Issue><Address>Cardiology Division, William Beaumont Hospital, Royal Oak, Michigan, USA</Address><Web_URL>PM:14522475</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[20]. In this study, reinfarction occurred in 2.1% of cases at one month, lower than that observed in the Keeley analysis. In addition this study demonstrated that the admission Killip class >1, left ventricular ejection fraction <50%, final % coronary stenosis >30%, coronary artery dissection and presence of thrombus were associated with reinfarction. One month reinfarction was associated with an occurrence of death (OR 7.14, 95% CI 3.28 to 15.5) and ischemic target vessel revascularization (OR 15.0, 95% CI 8.68 to 26.0) at 6 months. This study however, may not accurately reflect current practice due to the reduced use of glycoprotein IIb/IIIa inhibitors and stents in the PAMI trials.
Primary PTCA versus pre-hospital thrombolysis
Primary PCI is not only superior to in-hospital thrombolysis but also superior compared with pre-hospital thrombolysis. This was indeed demonstrated in the Register of Information and Knowledge about Swedish Heart Intensive care Admissions (RIKS-HIA) study ADDIN REFMGR.CITE <Refman><Author>Stenestrand</Author><Year>2006</Year><RecNum>495</RecNum><IDText>Long-term outcome of primary percutaneous coronary intervention vs prehospital and in-hospital thrombolysis for patients with ST-elevation myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>495</Ref_ID><Title_Primary>Long-term outcome of primary percutaneous coronary intervention vs prehospital and in-hospital thrombolysis for patients with ST-elevation myocardial infarction</Title_Primary><Authors_Primary>Stenestrand,U.</Authors_Primary><Authors_Primary>Lindback,J.</Authors_Primary><Authors_Primary>Wallentin,L.</Authors_Primary><Date_Primary>2006/10/11</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Clinical Trials</Keywords><Keywords>Cohort Studies</Keywords><Keywords>Comorbidity</Keywords><Keywords>Emergency Medical Services</Keywords><Keywords>Emergency Service,Hospital</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Intensive Care</Keywords><Keywords>Length of Stay</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Proportional Hazards Models</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Registries</Keywords><Keywords>Survival Analysis</Keywords><Keywords>Sweden</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>1749</Start_Page><End_Page>1756</End_Page><Periodical>JAMA</Periodical><Volume>296</Volume><Issue>14</Issue><Address>Department of Cardiology, University Hospital, Linkoping, Sweden. stenestrand@riks-hia.se</Address><Web_URL>PM:17032988</Web_URL><ZZ_JournalStdAbbrev><f name="System">JAMA</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[21] which consisted of 26 205 patients with ST elevation myocardial infarction. Patients who underwent primary PCI demonstrated clear benefits in terms of reduction in mortality at 30 days (4.9% vs. 7.6% vs. 11.4%) and at one year (7.6% vs. 10.3% vs. 15.9%) compared to those who had pre-hospital thrombolysis and in-hospital thrombolysis. Primary PCI patients had shorter hospital stay and less reinfarction compared to the other two groups.
Advances in PCI
Over the last 15 years there has been significant development in the stent technology and adjunctive pharmacotherapy which further enhances the outcomes of primary angioplasty now commonly referred to as primary percutaneous coronary intervention (PCI).
Intracoronary stenting
Stent-PAMI study
The safety and efficacy of primary stenting using the Palmaz-Schatz stents for patients with acute ST elevation myocardial infarction was examined in the stent PAMI trials ADDIN REFMGR.CITE <Refman><Author>Stone</Author><Year>1998</Year><RecNum>1786</RecNum><IDText>Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1786</Ref_ID><Title_Primary>Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators</Title_Primary><Authors_Primary>Stone,G.W.</Authors_Primary><Authors_Primary>Brodie,B.R.</Authors_Primary><Authors_Primary>Griffin,J.J.</Authors_Primary><Authors_Primary>Morice,M.C.</Authors_Primary><Authors_Primary>Costantini,C.</Authors_Primary><Authors_Primary>St Goar,F.G.</Authors_Primary><Authors_Primary>Overlie,P.A.</Authors_Primary><Authors_Primary>Popma,J.J.</Authors_Primary><Authors_Primary>McDonnell,J.</Authors_Primary><Authors_Primary>Jones,D.</Authors_Primary><Authors_Primary>O'Neill,W.W.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Date_Primary>1998/1</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Arteries</Keywords><Keywords>Aspirin</Keywords><Keywords>California</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Feasibility Studies</Keywords><Keywords>Female</Keywords><Keywords>Heparin</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Ischemia</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Pilot Projects</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Regional Blood Flow</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Safety</Keywords><Keywords>Stents</Keywords><Keywords>therapy</Keywords><Keywords>Ticlopidine</Keywords><Reprint>Not in File</Reprint><Start_Page>23</Start_Page><End_Page>30</End_Page><Periodical>J.Am.Coll.Cardiol.</Periodical><Volume>31</Volume><Issue>1</Issue><Address>Cardiovascular Institute, El Camino Hospital, Mountain View, California 94040, USA. gstone1418@aol.com</Address><Web_URL>PM:9426013</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Stone</Author><Year>1999</Year><RecNum>1787</RecNum><IDText>Clinical and angiographic follow-Up after primary stenting in acute myocardial infarction: the Primary Angioplasty in Myocardial Infarction (PAMI) stent pilot trial</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1787</Ref_ID><Title_Primary>Clinical and angiographic follow-Up after primary stenting in acute myocardial infarction: the Primary Angioplasty in Myocardial Infarction (PAMI) stent pilot trial</Title_Primary><Authors_Primary>Stone,G.W.</Authors_Primary><Authors_Primary>Brodie,B.R.</Authors_Primary><Authors_Primary>Griffin,J.J.</Authors_Primary><Authors_Primary>Costantini,C.</Authors_Primary><Authors_Primary>Morice,M.C.</Authors_Primary><Authors_Primary>St Goar,F.G.</Authors_Primary><Authors_Primary>Overlie,P.A.</Authors_Primary><Authors_Primary>Popma,J.J.</Authors_Primary><Authors_Primary>McDonnell,J.</Authors_Primary><Authors_Primary>Jones,D.</Authors_Primary><Authors_Primary>O'Neill,W.W.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Date_Primary>1999/3/30</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>contraindications</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Pilot Projects</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Recurrence</Keywords><Keywords>Regression Analysis</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Stents</Keywords><Keywords>Survival</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Washington</Keywords><Reprint>Not in File</Reprint><Start_Page>1548</Start_Page><End_Page>1554</End_Page><Periodical>Circulation</Periodical><Volume>99</Volume><Issue>12</Issue><Address>Washington Hospital Center, Washington, DC20010, USA</Address><Web_URL>PM:10096929</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[22;23]. In the pilot trial, 312 patients from 9 centers were included. Of these, 240 (77%) patients underwent stenting which was successful in 98% of the cases. TIMI flow grade 3 was achieved in 96% of cases. Low rates of in-hospital death (0.8%), reinfarction (1.7%), recurrent ischemia (3.8%) and pre discharge target vessel revascularization (1.3%) were demonstrated with the stenting strategy ADDIN REFMGR.CITE <Refman><Author>Stone</Author><Year>1998</Year><RecNum>1786</RecNum><IDText>Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1786</Ref_ID><Title_Primary>Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators</Title_Primary><Authors_Primary>Stone,G.W.</Authors_Primary><Authors_Primary>Brodie,B.R.</Authors_Primary><Authors_Primary>Griffin,J.J.</Authors_Primary><Authors_Primary>Morice,M.C.</Authors_Primary><Authors_Primary>Costantini,C.</Authors_Primary><Authors_Primary>St Goar,F.G.</Authors_Primary><Authors_Primary>Overlie,P.A.</Authors_Primary><Authors_Primary>Popma,J.J.</Authors_Primary><Authors_Primary>McDonnell,J.</Authors_Primary><Authors_Primary>Jones,D.</Authors_Primary><Authors_Primary>O'Neill,W.W.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Date_Primary>1998/1</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Arteries</Keywords><Keywords>Aspirin</Keywords><Keywords>California</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Feasibility Studies</Keywords><Keywords>Female</Keywords><Keywords>Heparin</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Ischemia</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Pilot Projects</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Regional Blood Flow</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Safety</Keywords><Keywords>Stents</Keywords><Keywords>therapy</Keywords><Keywords>Ticlopidine</Keywords><Reprint>Not in File</Reprint><Start_Page>23</Start_Page><End_Page>30</End_Page><Periodical>J.Am.Coll.Cardiol.</Periodical><Volume>31</Volume><Issue>1</Issue><Address>Cardiovascular Institute, El Camino Hospital, Mountain View, California 94040, USA. gstone1418@aol.com</Address><Web_URL>PM:9426013</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[22]. There were no additional events at 30 days except the occurrence of target vessel revascularization (TVR) in one patient. A subsequent study from the same group demonstrated that at 7.4±2.6 month follow-up, the incidence of death, reinfarction and TVR continued to be low among patients who underwent primary angioplasty using stents. This was also associated with a low rate of restenosis at follow-up (27.5%) ADDIN REFMGR.CITE <Refman><Author>Stone</Author><Year>1999</Year><RecNum>1787</RecNum><IDText>Clinical and angiographic follow-Up after primary stenting in acute myocardial infarction: the Primary Angioplasty in Myocardial Infarction (PAMI) stent pilot trial</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1787</Ref_ID><Title_Primary>Clinical and angiographic follow-Up after primary stenting in acute myocardial infarction: the Primary Angioplasty in Myocardial Infarction (PAMI) stent pilot trial</Title_Primary><Authors_Primary>Stone,G.W.</Authors_Primary><Authors_Primary>Brodie,B.R.</Authors_Primary><Authors_Primary>Griffin,J.J.</Authors_Primary><Authors_Primary>Costantini,C.</Authors_Primary><Authors_Primary>Morice,M.C.</Authors_Primary><Authors_Primary>St Goar,F.G.</Authors_Primary><Authors_Primary>Overlie,P.A.</Authors_Primary><Authors_Primary>Popma,J.J.</Authors_Primary><Authors_Primary>McDonnell,J.</Authors_Primary><Authors_Primary>Jones,D.</Authors_Primary><Authors_Primary>O'Neill,W.W.</Authors_Primary><Authors_Primary>Grines,C.L.</Authors_Primary><Date_Primary>1999/3/30</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>contraindications</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Pilot Projects</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Recurrence</Keywords><Keywords>Regression Analysis</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Stents</Keywords><Keywords>Survival</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Washington</Keywords><Reprint>Not in File</Reprint><Start_Page>1548</Start_Page><End_Page>1554</End_Page><Periodical>Circulation</Periodical><Volume>99</Volume><Issue>12</Issue><Address>Washington Hospital Center, Washington, DC20010, USA</Address><Web_URL>PM:10096929</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[23].
STOP-AMI study
Stenting in combination with glycoprotein IIb/IIIa inhibitor was examined in the STOP-AMI trial (Stent versus Fibrinolysis for Occluded coronary arteries in patients with Acute Myocardial Infarction) ADDIN REFMGR.CITE <Refman><Author>Schomig</Author><Year>2000</Year><RecNum>441</RecNum><IDText>Coronary stenting plus platelet glycoprotein IIb/IIIa blockade compared with tissue plasminogen activator in acute myocardial infarction. Stent versus Thrombolysis for Occluded Coronary Arteries in Patients with Acute Myocardial Infarction Study Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>441</Ref_ID><Title_Primary>Coronary stenting plus platelet glycoprotein IIb/IIIa blockade compared with tissue plasminogen activator in acute myocardial infarction. Stent versus Thrombolysis for Occluded Coronary Arteries in Patients with Acute Myocardial Infarction Study Investigators</Title_Primary><Authors_Primary>Schomig,A.</Authors_Primary><Authors_Primary>Kastrati,A.</Authors_Primary><Authors_Primary>Dirschinger,J.</Authors_Primary><Authors_Primary>Mehilli,J.</Authors_Primary><Authors_Primary>Schricke,U.</Authors_Primary><Authors_Primary>Pache,J.</Authors_Primary><Authors_Primary>Martinoff,S.</Authors_Primary><Authors_Primary>Neumann,F.J.</Authors_Primary><Authors_Primary>Schwaiger,M.</Authors_Primary><Date_Primary>2000/8/10</Date_Primary><Keywords>Aged</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Arteries</Keywords><Keywords>Cerebrovascular Accident</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Comparative Study</Keywords><Keywords>drug therapy</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Germany</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Incidence</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>pathology</Keywords><Keywords>Platelet Aggregation Inhibitors</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>radionuclide imaging</Keywords><Keywords>Recurrence</Keywords><Keywords>Research Support,Non-U.S.Gov't</Keywords><Keywords>Risk</Keywords><Keywords>Stents</Keywords><Keywords>Technetium Tc 99m Sestamibi</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>385</Start_Page><End_Page>391</End_Page><Periodical>N Engl J Med</Periodical><Volume>343</Volume><Issue>6</Issue><Address>Deutsches Herzzentrum, 1. Medizinische Klinik rechts der Isar, Munich, Germany. aschoemig@dhm.mhn.de</Address><Web_URL>PM:10933737</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[24]. One hundred and forty patients were randomized to undergo PCI using stents (n=71) and abciximab or to receive alteplase (n=69). The primary endpoint of this study consisted of the degree of myocardial salvage assessed using Tc 99m sestamibi scans. The median infarct size in the PCI group was significantly reduced compared to the fibrinolytic group (14.3% vs. 19.4%, p=0.02). The salvage index which is calculated by dividing the % of left ventricle salvaged by % of left ventricle compromised by the initial reperfusion defect was also favorable with primary PCI (PPCI) compared to fibrinolysis (0.57 vs. 0.26, p<0.001). The cumulative incidence of death, reinfarction and stroke at 6 months was significantly reduced in the PPCI group (8.5% vs. 23.2%, p=0.02).
Drug eluting stents in PPCI
Sirolimus-eluting stent studies
Over the last five years, drug eluting stents have played a major role in reducing the incidence of restenosis. The advantages of using drug eluting stents have been examined in the setting of an acute myocardial infarction. In the Trial to assess the use of the cYPHer stent in acute myocardial infarction treated with ballOON angioplasty (TYPHOON), ADDIN REFMGR.CITE <Refman><Author>Spaulding</Author><Year>2006</Year><RecNum>3657</RecNum><IDText>Sirolimus-eluting versus uncoated stents in acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>3657</Ref_ID><Title_Primary>Sirolimus-eluting versus uncoated stents in acute myocardial infarction</Title_Primary><Authors_Primary>Spaulding,C.</Authors_Primary><Authors_Primary>Henry,P.</Authors_Primary><Authors_Primary>Teiger,E.</Authors_Primary><Authors_Primary>Beatt,K.</Authors_Primary><Authors_Primary>Bramucci,E.</Authors_Primary><Authors_Primary>Carrie,D.</Authors_Primary><Authors_Primary>Slama,M.S.</Authors_Primary><Authors_Primary>Merkely,B.</Authors_Primary><Authors_Primary>Erglis,A.</Authors_Primary><Authors_Primary>Margheri,M.</Authors_Primary><Authors_Primary>Varenne,O.</Authors_Primary><Authors_Primary>Cebrian,A.</Authors_Primary><Authors_Primary>Stoll,H.P.</Authors_Primary><Authors_Primary>Snead,D.B.</Authors_Primary><Authors_Primary>Bode,C.</Authors_Primary><Date_Primary>2006/9/14</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Artery Bypass</Keywords><Keywords>Death</Keywords><Keywords>Disease-Free Survival</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>France</Keywords><Keywords>Humans</Keywords><Keywords>Immunosuppressive Agents</Keywords><Keywords>Infarction</Keywords><Keywords>Logistic Models</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Paris</Keywords><Keywords>Patients</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>prevention & control</Keywords><Keywords>Recurrence</Keywords><Keywords>Research</Keywords><Keywords>Safety</Keywords><Keywords>Single-Blind Method</Keywords><Keywords>Sirolimus</Keywords><Keywords>Stents</Keywords><Keywords>therapy</Keywords><Keywords>Thrombosis</Keywords><Keywords>Vascular Patency</Keywords><Reprint>Not in File</Reprint><Start_Page>1093</Start_Page><End_Page>1104</End_Page><Periodical>N Engl J Med</Periodical><Volume>355</Volume><Issue>11</Issue><Address>Assistance Publique-Hopitaux de Paris (AP-HP) Cochin Hospital, Paris 5 Medical School Rene Descartes University and INSERM U780, Paris, France. christian.spaulding@cch.ap-hop-paris.fr</Address><Web_URL>PM:16971716</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[25] the use of sirolimus eluting stents was associated with a significant reduction in the primary endpoint of target vessel failure at one year which consisted of target vessel failure related death, repeat myocardial infarction and target vessel revascularization (7.3% vs. 14.3%, p=0.004) which was mainly driven by a reduction in the occurrence of target vessel revascularization (5.6% vs. 13.4 %, p<0.001) without a significant reduction in death and repeat myocardial infarction (MI) .
Likewise, the SESAMI study (Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction) demonstrated that primary PCI using sirolimus eluting stent compared to bare metal stent was associated with reduction in binary restenosis by 56%, target lesion revascularization by 61%, target vessel revascularization by 62%, adverse events by 59% and target vessel failure by 53% at one year ADDIN REFMGR.CITE <Refman><Author>Menichelli</Author><Year>2007</Year><RecNum>1908</RecNum><IDText>Randomized trial of Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction (SESAMI)</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1908</Ref_ID><Title_Primary>Randomized trial of Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction (SESAMI)</Title_Primary><Authors_Primary>Menichelli,M.</Authors_Primary><Authors_Primary>Parma,A.</Authors_Primary><Authors_Primary>Pucci,E.</Authors_Primary><Authors_Primary>Fiorilli,R.</Authors_Primary><Authors_Primary>De,Felice F.</Authors_Primary><Authors_Primary>Nazzaro,M.</Authors_Primary><Authors_Primary>Giulivi,A.</Authors_Primary><Authors_Primary>Alborino,D.</Authors_Primary><Authors_Primary>Azzellino,A.</Authors_Primary><Authors_Primary>Violini,R.</Authors_Primary><Date_Primary>2007/5/15</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Drug-Eluting Stents</Keywords><Keywords>epidemiology</Keywords><Keywords>Equipment Design</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Graft Occlusion,Vascular</Keywords><Keywords>Humans</Keywords><Keywords>Immunosuppressive Agents</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>radiography</Keywords><Keywords>Sirolimus</Keywords><Keywords>Stents</Keywords><Keywords>therapy</Keywords><Keywords>Thrombosis</Keywords><Reprint>Not in File</Reprint><Start_Page>1924</Start_Page><End_Page>1930</End_Page><Periodical>J.Am.Coll.Cardiol.</Periodical><Volume>49</Volume><Issue>19</Issue><Address>Division of Interventional Cardiology, San Camillo Hospital, Rome, Italy. menichelli747@yahoo.com</Address><Web_URL>PM:17498576</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[26]. The Single High Dose Bolus Tirofiban and Sirolimus Eluting Stent vs. Abciximab and Bare Metal Stent in Myocardial Infarction study (STRATEGY) demonstrated that PPCI using high dose tirofiban and sirolimus eluting stents (n=87) was associated with a significant reduction in the primary endpoint of combined death, non fatal reinfarction, stroke and binary restenosis at 8 months (19% vs. 50%, p<0.001) compared to a strategy of abciximab and bare metal stent implantation (n=88). The binary restenosis was also significantly reduced in the sirolimus group (9% vs. 36%, p=0.002) ADDIN REFMGR.CITE <Refman><Author>Valgimigli</Author><Year>2005</Year><RecNum>1909</RecNum><IDText>Tirofiban and sirolimus-eluting stent vs abciximab and bare-metal stent for acute myocardial infarction: a randomized trial</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1909</Ref_ID><Title_Primary>Tirofiban and sirolimus-eluting stent vs abciximab and bare-metal stent for acute myocardial infarction: a randomized trial</Title_Primary><Authors_Primary>Valgimigli,M.</Authors_Primary><Authors_Primary>Percoco,G.</Authors_Primary><Authors_Primary>Malagutti,P.</Authors_Primary><Authors_Primary>Campo,G.</Authors_Primary><Authors_Primary>Ferrari,F.</Authors_Primary><Authors_Primary>Barbieri,D.</Authors_Primary><Authors_Primary>Cicchitelli,G.</Authors_Primary><Authors_Primary>McFadden,E.P.</Authors_Primary><Authors_Primary>Merlini,F.</Authors_Primary><Authors_Primary>Ansani,L.</Authors_Primary><Authors_Primary>Guardigli,G.</Authors_Primary><Authors_Primary>Bettini,A.</Authors_Primary><Authors_Primary>Parrinello,G.</Authors_Primary><Authors_Primary>Boersma,E.</Authors_Primary><Authors_Primary>Ferrari,R.</Authors_Primary><Date_Primary>2005/5/4</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Aged</Keywords><Keywords>analogs & derivatives</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Arteries</Keywords><Keywords>Bundle-Branch Block</Keywords><Keywords>Cardiology</Keywords><Keywords>Comparative Study</Keywords><Keywords>Drug Delivery Systems</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Immunosuppressive Agents</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Platelet Aggregation</Keywords><Keywords>Platelet Aggregation Inhibitors</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Single-Blind Method</Keywords><Keywords>Sirolimus</Keywords><Keywords>Stents</Keywords><Keywords>Stroke</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Tyrosine</Keywords><Reprint>Not in File</Reprint><Start_Page>2109</Start_Page><End_Page>2117</End_Page><Periodical>JAMA</Periodical><Volume>293</Volume><Issue>17</Issue><Address>Chair of Cardiology, University of Ferrara, Cardiovascular Institute, Arcispedale S. Anna, Italy. vlgmrc@unife.it</Address><Web_URL>PM:15870414</Web_URL><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[27].
Paclitaxel-eluting stent study
On the other hand, in the PASSION trial (Paclitaxel-Eluting Stent versus Conventional Stent in Myocardial Infarction with ST-Segment Elevation) using paclitaxel eluting stents, the benefits of using paclitaxel eluting stents following an acute myocardial infarction were not striking. There was a trend towards reduction in death, recurrent myocardial infarction and target vessel revascularization (8.8% vs. 12.8%, p=0.09) with no difference in death, recurrent MI and TVR when assessed independently compared to the bare metal stents ADDIN REFMGR.CITE <Refman><Author>Laarman</Author><Year>2006</Year><RecNum>3382</RecNum><IDText>Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>3382</Ref_ID><Title_Primary>Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention</Title_Primary><Authors_Primary>Laarman,G.J.</Authors_Primary><Authors_Primary>Suttorp,M.J.</Authors_Primary><Authors_Primary>Dirksen,M.T.</Authors_Primary><Authors_Primary>van,Heerebeek L.</Authors_Primary><Authors_Primary>Kiemeneij,F.</Authors_Primary><Authors_Primary>Slagboom,T.</Authors_Primary><Authors_Primary>van der Wieken,L.R.</Authors_Primary><Authors_Primary>Tijssen,J.G.</Authors_Primary><Authors_Primary>Rensing,B.J.</Authors_Primary><Authors_Primary>Patterson,M.</Authors_Primary><Date_Primary>2006/9/14</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Cardiology</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Artery Bypass</Keywords><Keywords>Death</Keywords><Keywords>Disease-Free Survival</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Immunosuppressive Agents</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Netherlands</Keywords><Keywords>Paclitaxel</Keywords><Keywords>Patients</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>prevention & control</Keywords><Keywords>Proportional Hazards Models</Keywords><Keywords>Recurrence</Keywords><Keywords>Risk</Keywords><Keywords>Single-Blind Method</Keywords><Keywords>Stents</Keywords><Keywords>therapy</Keywords><Keywords>Thrombosis</Keywords><Reprint>Not in File</Reprint><Start_Page>1105</Start_Page><End_Page>1113</End_Page><Periodical>N Engl J Med</Periodical><Volume>355</Volume><Issue>11</Issue><Address>Department of Interventional Cardiology, Onze Lieve Vrouwe Gasthuis, Amsterdam, The Netherlands. g.j.laarman@olvg.nl</Address><Web_URL>PM:16971717</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[28].
Adjunctive pharmacotherapy
Glycoprotein IIb/IIIa inhibitor therapy
RAPPORT trial
The use of adjunctive pharmacotherapy using glycoprotein IIb/IIIa inhibitor was assessed in the RAPPORT trial (Reopro And Primary PTCA Organization and Randomized Trial) ADDIN REFMGR.CITE <Refman><Author>Brener</Author><Year>1998</Year><RecNum>437</RecNum><IDText>Randomized, placebo-controlled trial of platelet glycoprotein IIb/IIIa blockade with primary angioplasty for acute myocardial infarction. ReoPro and Primary PTCA Organization and Randomized Trial (RAPPORT) Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>437</Ref_ID><Title_Primary>Randomized, placebo-controlled trial of platelet glycoprotein IIb/IIIa blockade with primary angioplasty for acute myocardial infarction. ReoPro and Primary PTCA Organization and Randomized Trial (RAPPORT) Investigators</Title_Primary><Authors_Primary>Brener,S.J.</Authors_Primary><Authors_Primary>Barr,L.A.</Authors_Primary><Authors_Primary>Burchenal,J.E.</Authors_Primary><Authors_Primary>Katz,S.</Authors_Primary><Authors_Primary>George,B.S.</Authors_Primary><Authors_Primary>Jones,A.A.</Authors_Primary><Authors_Primary>Cohen,E.D.</Authors_Primary><Authors_Primary>Gainey,P.C.</Authors_Primary><Authors_Primary>White,H.J.</Authors_Primary><Authors_Primary>Cheek,H.B.</Authors_Primary><Authors_Primary>Moses,J.W.</Authors_Primary><Authors_Primary>Moliterno,D.J.</Authors_Primary><Authors_Primary>Effron,M.B.</Authors_Primary><Authors_Primary>Topol,E.J.</Authors_Primary><Date_Primary>1998/8/25</Date_Primary><Keywords>adverse effects</Keywords><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Arteries</Keywords><Keywords>chemically induced</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Double-Blind Method</Keywords><Keywords>Female</Keywords><Keywords>Hemorrhage</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Incidence</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Platelet Aggregation Inhibitors</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>Postoperative Hemorrhage</Keywords><Keywords>Research Support,Non-U.S.Gov't</Keywords><Keywords>Stents</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>734</Start_Page><End_Page>741</End_Page><Periodical>Circulation</Periodical><Volume>98</Volume><Issue>8</Issue><Address>Cleveland Clinic Foundation, Ohio 44195, USA</Address><Web_URL>PM:9727542</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[29]. Patients underwent primary PTCA with (n=241) and without abciximab (n=242). Abciximab significantly reduced the incidence of death, reinfarction and target vessel revascularization at 7 days (3.3% vs. 9.9%, p=0.03), 30 days (5.8% vs. 11.2%, p=0.003) and at 6 months (11.6% vs. 17.8%, p=0.05). The need for bail-out glycoprotein IIb/IIIa inhibitor therapy was reduced in the abciximab group by 42%, p=0.008. However, there was an increased risk of major bleed in the abciximab group (16.6% vs. 9.5%, p=0.02) compared to the placebo group.
ADMIRAL study
The ADMIRAL study (Abciximab before Direct Angioplasty and Stenting in Myocardial Infarction Regarding Acute and Long-term follow-up) determined the benefit of administration of abciximab in patients undergoing primary angioplasty with stenting (149 patients received stents and abciximab, 151 patients received stents and placebo) ADDIN REFMGR.CITE <Refman><Author>Montalescot</Author><Year>2001</Year><RecNum>1789</RecNum><IDText>Platelet glycoprotein IIb/IIIa inhibition with coronary stenting for acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1789</Ref_ID><Title_Primary>Platelet glycoprotein IIb/IIIa inhibition with coronary stenting for acute myocardial infarction</Title_Primary><Authors_Primary>Montalescot,G.</Authors_Primary><Authors_Primary>Barragan,P.</Authors_Primary><Authors_Primary>Wittenberg,O.</Authors_Primary><Authors_Primary>Ecollan,P.</Authors_Primary><Authors_Primary>Elhadad,S.</Authors_Primary><Authors_Primary>Villain,P.</Authors_Primary><Authors_Primary>Boulenc,J.M.</Authors_Primary><Authors_Primary>Morice,M.C.</Authors_Primary><Authors_Primary>Maillard,L.</Authors_Primary><Authors_Primary>Pansieri,M.</Authors_Primary><Authors_Primary>Choussat,R.</Authors_Primary><Authors_Primary>Pinton,P.</Authors_Primary><Date_Primary>2001/6/21</Date_Primary><Keywords>adverse effects</Keywords><Keywords>Aged</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Cardiology</Keywords><Keywords>classification</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Double-Blind Method</Keywords><Keywords>drug therapy</Keywords><Keywords>Drug Therapy,Combination</Keywords><Keywords>Female</Keywords><Keywords>France</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Platelet Aggregation</Keywords><Keywords>Platelet Aggregation Inhibitors</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>prevention & control</Keywords><Keywords>Recurrence</Keywords><Keywords>Research</Keywords><Keywords>Stents</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1895</Start_Page><End_Page>1903</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>344</Volume><Issue>25</Issue><Address>Division of Cardiology, Pitie-Salpetriere Hospital, Paris, France. gilles.montalescot@psl.ap-hop-paris.fr</Address><Web_URL>PM:11419426</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[30]. Abciximab administration was associated with an increase in pre-PCI (16.8% vs. 5.4%, p=0.01) and post-PCI (95.1% vs. 86.7%, p=0.04) TIMI flow grade 3. There was a significant reduction in the incidence of combined death, reinfarction and target vessel revascularization in the abciximab group compared to the placebo group at 30 days (6% vs. 14.6%, p=0.01) and at 6 months (7.4% vs. 15.9%, p=0.02) without an increase in major bleed (0.7% vs. 0%). The six-moth left ventricular ejection fraction was also significantly better in the abciximab group compared to the placebo group (61.1±10.6 vs. 57±11.1, p=0.05).
Intracoronary pharmacotherapy during primary angioplasty
One of the problems encountered during PPCI is the occurrence of no-reflow phenomenon despite the lack of obvious epicardial obstruction which is as a result of microvascular dysfunction. Piana et al demonstrated that no-reflow occurred in 11.5% of cases undergoing PTCA following an acute myocardial infarction compared to those who had PTCA in the non-infarct setting (1.5%, p<0.001) ADDIN REFMGR.CITE <Refman><Author>Piana</Author><Year>1994</Year><RecNum>1916</RecNum><IDText>Incidence and treatment of 'no-reflow' after percutaneous coronary intervention</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1916</Ref_ID><Title_Primary>Incidence and treatment of 'no-reflow' after percutaneous coronary intervention</Title_Primary><Authors_Primary>Piana,R.N.</Authors_Primary><Authors_Primary>Paik,G.Y.</Authors_Primary><Authors_Primary>Moscucci,M.</Authors_Primary><Authors_Primary>Cohen,D.J.</Authors_Primary><Authors_Primary>Gibson,C.M.</Authors_Primary><Authors_Primary>Kugelmass,A.D.</Authors_Primary><Authors_Primary>Carrozza,J.P.,Jr.</Authors_Primary><Authors_Primary>Kuntz,R.E.</Authors_Primary><Authors_Primary>Baim,D.S.</Authors_Primary><Date_Primary>1994/6</Date_Primary><Keywords>adverse effects</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Ischemia</Keywords><Keywords>methods</Keywords><Keywords>Myocardial Ischemia</Keywords><Keywords>Nitroglycerin</Keywords><Keywords>Prevalence</Keywords><Keywords>Research</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>Stents</Keywords><Keywords>surgery</Keywords><Keywords>Syndrome</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Verapamil</Keywords><Reprint>Not in File</Reprint><Start_Page>2514</Start_Page><End_Page>2518</End_Page><Periodical>Circulation</Periodical><Volume>89</Volume><Issue>6</Issue><Address>Charles A. Dana Research Institute, Boston, MA</Address><Web_URL>PM:8205658</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[31].
Mechanisms of no-flow phenomenon
Several mechanisms have been postulated for the development of microvascular dysfunction and no-reflow phenomenon including α-adrenergic mediated macro and microvascular constriction ADDIN REFMGR.CITE <Refman><Author>Gregorini</Author><Year>1999</Year><RecNum>328</RecNum><IDText>Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>328</Ref_ID><Title_Primary>Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction</Title_Primary><Authors_Primary>Gregorini,L.</Authors_Primary><Authors_Primary>Marco,J.</Authors_Primary><Authors_Primary>Kozakova,M.</Authors_Primary><Authors_Primary>Palombo,C.</Authors_Primary><Authors_Primary>Anguissola,G.B.</Authors_Primary><Authors_Primary>Marco,I.</Authors_Primary><Authors_Primary>Bernies,M.</Authors_Primary><Authors_Primary>Cassagneau,B.</Authors_Primary><Authors_Primary>Distante,A.</Authors_Primary><Authors_Primary>Bossi,I.M.</Authors_Primary><Authors_Primary>Fajadet,J.</Authors_Primary><Authors_Primary>Heusch,G.</Authors_Primary><Date_Primary>1999/2/2</Date_Primary><Keywords>Adrenergic alpha-Antagonists</Keywords><Keywords>Adrenergic beta-Antagonists</Keywords><Keywords>Aged</Keywords><Keywords>Angiography</Keywords><Keywords>Arteries</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Echocardiography</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Perfusion</Keywords><Keywords>Phentolamine</Keywords><Keywords>physiopathology</Keywords><Keywords>Piperazines</Keywords><Keywords>radiography</Keywords><Keywords>Receptors,Adrenergic,alpha</Keywords><Keywords>Stents</Keywords><Keywords>surgery</Keywords><Keywords>therapeutic use</Keywords><Keywords>Vasoconstriction</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>482</Start_Page><End_Page>490</End_Page><Periodical>Circulation</Periodical><Volume>99</Volume><Issue>4</Issue><Address>Clinique Pasteur, Centre de Cardiologie Interventionelle, Toulouse, France. luisa.gregorini@unimi.it</Address><Web_URL>PM:9927393</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Gregorini</Author><Year>2002</Year><RecNum>329</RecNum><IDText>Effects of selective alpha1- and alpha2-adrenergic blockade on coronary flow reserve after coronary stenting</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>329</Ref_ID><Title_Primary>Effects of selective alpha1- and alpha2-adrenergic blockade on coronary flow reserve after coronary stenting</Title_Primary><Authors_Primary>Gregorini,L.</Authors_Primary><Authors_Primary>Marco,J.</Authors_Primary><Authors_Primary>Farah,B.</Authors_Primary><Authors_Primary>Bernies,M.</Authors_Primary><Authors_Primary>Palombo,C.</Authors_Primary><Authors_Primary>Kozakova,M.</Authors_Primary><Authors_Primary>Bossi,I.M.</Authors_Primary><Authors_Primary>Cassagneau,B.</Authors_Primary><Authors_Primary>Fajadet,J.</Authors_Primary><Authors_Primary>Di,Mario C.</Authors_Primary><Authors_Primary>Albiero,R.</Authors_Primary><Authors_Primary>Cugno,M.</Authors_Primary><Authors_Primary>Grossi,A.</Authors_Primary><Authors_Primary>Heusch,G.</Authors_Primary><Date_Primary>2002/12/3</Date_Primary><Keywords>Adenosine</Keywords><Keywords>Adrenergic alpha-Antagonists</Keywords><Keywords>adverse effects</Keywords><Keywords>Angiography</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Disease</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>diagnostic use</Keywords><Keywords>drug effects</Keywords><Keywords>Female</Keywords><Keywords>Heart Rate</Keywords><Keywords>Humans</Keywords><Keywords>Hyperemia</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>pharmacology</Keywords><Keywords>physiopathology</Keywords><Keywords>Piperazines</Keywords><Keywords>radiography</Keywords><Keywords>Receptors,Adrenergic,alpha-1</Keywords><Keywords>Receptors,Adrenergic,alpha-2</Keywords><Keywords>Stents</Keywords><Keywords>surgery</Keywords><Keywords>transplantation</Keywords><Keywords>Vascular Patency</Keywords><Keywords>Vasoconstriction</Keywords><Keywords>Yohimbine</Keywords><Reprint>Not in File</Reprint><Start_Page>2901</Start_Page><End_Page>2907</End_Page><Periodical>Circulation</Periodical><Volume>106</Volume><Issue>23</Issue><Address>Experimental Surgery and Transplantation Institute, Ospedale Maggiore IRCCS, University of Milano, Italy. Luisa.Gregorini@unimi.it</Address><Web_URL>PM:12460869</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[32;33]. Endothelial dysfunction detected by elevated levels of different factors is noted among patients with coronary slow-flow phenomenon ADDIN REFMGR.CITE <Refman><Author>Sezgin</Author><Year>2003</Year><RecNum>2338</RecNum><IDText>Vascular endothelial function in patients with slow coronary flow</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2338</Ref_ID><Title_Primary>Vascular endothelial function in patients with slow coronary flow</Title_Primary><Authors_Primary>Sezgin,A.T.</Authors_Primary><Authors_Primary>Sigirci,A.</Authors_Primary><Authors_Primary>Barutcu,I.</Authors_Primary><Authors_Primary>Topal,E.</Authors_Primary><Authors_Primary>Sezgin,N.</Authors_Primary><Authors_Primary>Ozdemir,R.</Authors_Primary><Authors_Primary>Yetkin,E.</Authors_Primary><Authors_Primary>Tandogan,I.</Authors_Primary><Authors_Primary>Kosar,F.</Authors_Primary><Authors_Primary>Ermis,N.</Authors_Primary><Authors_Primary>Yologlu,S.</Authors_Primary><Authors_Primary>Bariskaner,E.</Authors_Primary><Authors_Primary>Cehreli,S.</Authors_Primary><Date_Primary>2003/4</Date_Primary><Keywords>Adult</Keywords><Keywords>analysis</Keywords><Keywords>Arteries</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Brachial Artery</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Arteriosclerosis</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Endothelium,Vascular</Keywords><Keywords>Evaluation Studies</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Hyperemia</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Nitroglycerin</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Regression Analysis</Keywords><Keywords>Statistics</Keywords><Keywords>therapeutic use</Keywords><Keywords>Thrombosis</Keywords><Keywords>Turkey</Keywords><Keywords>Vasodilation</Keywords><Keywords>Vasodilator Agents</Keywords><Reprint>Not in File</Reprint><Start_Page>155</Start_Page><End_Page>161</End_Page><Periodical>Coron.Artery Dis.</Periodical><Volume>14</Volume><Issue>2</Issue><Address>Department of Cardiology, Inonu University, Malatya, Turkey. alpayt.sezgin@superonline.com</Address><Web_URL>PM:12655279</Web_URL><ZZ_JournalStdAbbrev><f name="System">Coron.Artery Dis.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[34]. A number of previous studies have demonstrated elevated levels of plasma endothelin-1, asymmetric dimethylarginine (ADMA), plasma adhesion molecules [intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1) and E-selectin)], homocysteine, C-reactive protein (CRP), interleukin-6, noradrenaline and decreased levels of plasma nitric oxide in the setting of coronary slow-flow phenomenon ADDIN REFMGR.CITE <Refman><Author>Pekdemir</Author><Year>2004</Year><RecNum>2324</RecNum><IDText>The relationship between plasma endothelin-1, nitric oxide levels, and heart rate variability in patients with coronary slow flow</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2324</Ref_ID><Title_Primary>The relationship between plasma endothelin-1, nitric oxide levels, and heart rate variability in patients with coronary slow flow</Title_Primary><Authors_Primary>Pekdemir,H.</Authors_Primary><Authors_Primary>Cicek,D.</Authors_Primary><Authors_Primary>Camsari,A.</Authors_Primary><Authors_Primary>Akkus,M.N.</Authors_Primary><Authors_Primary>Cin,V.G.</Authors_Primary><Authors_Primary>Doven,O.</Authors_Primary><Authors_Primary>Parmaksiz,H.T.</Authors_Primary><Authors_Primary>Katircibasi,M.T.</Authors_Primary><Authors_Primary>Ozcan,I.T.</Authors_Primary><Date_Primary>2004/1</Date_Primary><Keywords>Analysis of Variance</Keywords><Keywords>Angiography</Keywords><Keywords>Arteries</Keywords><Keywords>Atherosclerosis</Keywords><Keywords>blood</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Cardiology</Keywords><Keywords>Case-Control Studies</Keywords><Keywords>Chi-Square Distribution</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Disease</Keywords><Keywords>diagnosis</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Endothelin-1</Keywords><Keywords>Exercise</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Heart Rate</Keywords><Keywords>Humans</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Nitric Oxide</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Plasma</Keywords><Keywords>Regional Blood Flow</Keywords><Keywords>Time</Keywords><Keywords>Turkey</Keywords><Keywords>ultrasonography</Keywords><Reprint>Not in File</Reprint><Start_Page>24</Start_Page><End_Page>33</End_Page><Periodical>Ann.Noninvasive.Electrocardiol.</Periodical><Volume>9</Volume><Issue>1</Issue><Address>Department of Cardiology, Medical Faculty, Mersin University, Mersin, Turkey. hpekdemir@hotmail.com</Address><Web_URL>PM:14731213</Web_URL><ZZ_JournalStdAbbrev><f name="System">Ann.Noninvasive.Electrocardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Turhan</Author><Year>2006</Year><RecNum>2276</RecNum><IDText>Increased plasma soluble adhesion molecules; ICAM-1, VCAM-1, and E-selectin levels in patients with slow coronary flow</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2276</Ref_ID><Title_Primary>Increased plasma soluble adhesion molecules; ICAM-1, VCAM-1, and E-selectin levels in patients with slow coronary flow</Title_Primary><Authors_Primary>Turhan,H.</Authors_Primary><Authors_Primary>Saydam,G.S.</Authors_Primary><Authors_Primary>Erbay,A.R.</Authors_Primary><Authors_Primary>Ayaz,S.</Authors_Primary><Authors_Primary>Yasar,A.S.</Authors_Primary><Authors_Primary>Aksoy,Y.</Authors_Primary><Authors_Primary>Basar,N.</Authors_Primary><Authors_Primary>Yetkin,E.</Authors_Primary><Date_Primary>2006/4/4</Date_Primary><Keywords>Adult</Keywords><Keywords>Angina Pectoris</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Blood Circulation Time</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>E-Selectin</Keywords><Keywords>Endothelium,Vascular</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Inflammation</Keywords><Keywords>Intercellular Adhesion Molecule-1</Keywords><Keywords>Leukocytes</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Plasma</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Regional Blood Flow</Keywords><Keywords>Turkey</Keywords><Keywords>Vascular Cell Adhesion Molecule-1</Keywords><Reprint>Not in File</Reprint><Start_Page>224</Start_Page><End_Page>230</End_Page><Periodical>Int.J.Cardiol.</Periodical><Volume>108</Volume><Issue>2</Issue><Address>Inonu University Medical Faculty, Department of Cardiology, Malatya, Turkey. drhturhan@yahoo.com</Address><Web_URL>PM:16002164</Web_URL><ZZ_JournalStdAbbrev><f name="System">Int.J.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Barutcu</Author><Year>2005</Year><RecNum>1377</RecNum><IDText>Elevated plasma homocysteine level in slow coronary flow</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1377</Ref_ID><Title_Primary>Elevated plasma homocysteine level in slow coronary flow</Title_Primary><Authors_Primary>Barutcu,I.</Authors_Primary><Authors_Primary>Sezgin,A.T.</Authors_Primary><Authors_Primary>Sezgin,N.</Authors_Primary><Authors_Primary>Gullu,H.</Authors_Primary><Authors_Primary>Esen,A.M.</Authors_Primary><Authors_Primary>Topal,E.</Authors_Primary><Authors_Primary>Ozdemir,R.</Authors_Primary><Date_Primary>2005/5/11</Date_Primary><Keywords>Angiography</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>blood supply</Keywords><Keywords>Case-Control Studies</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>Endothelium</Keywords><Keywords>Female</Keywords><Keywords>Homocysteine</Keywords><Keywords>Humans</Keywords><Keywords>Hyperhomocysteinemia</Keywords><Keywords>Male</Keywords><Keywords>metabolism</Keywords><Keywords>Middle Aged</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Vasodilation</Keywords><Reprint>Not in File</Reprint><Start_Page>143</Start_Page><End_Page>145</End_Page><Periodical>Int.J.Cardiol.</Periodical><Volume>101</Volume><Issue>1</Issue><Web_URL>PM:15860399</Web_URL><ZZ_JournalStdAbbrev><f name="System">Int.J.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Selcuk</Author><Year>2007</Year><RecNum>1376</RecNum><IDText>Asymmetric dimethylarginine plasma concentrations and L-arginine/asymmetric dimethylarginine ratio in patients with slow coronary flow</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1376</Ref_ID><Title_Primary>Asymmetric dimethylarginine plasma concentrations and L-arginine/asymmetric dimethylarginine ratio in patients with slow coronary flow</Title_Primary><Authors_Primary>Selcuk,M.T.</Authors_Primary><Authors_Primary>Selcuk,H.</Authors_Primary><Authors_Primary>Temizhan,A.</Authors_Primary><Authors_Primary>Maden,O.</Authors_Primary><Authors_Primary>Ulupinar,H.</Authors_Primary><Authors_Primary>Baysal,E.</Authors_Primary><Authors_Primary>Ozeke,O.</Authors_Primary><Authors_Primary>Sasmaz,A.</Authors_Primary><Date_Primary>2007/11</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>analogs & derivatives</Keywords><Keywords>analysis</Keywords><Keywords>Arginine</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Cardiology</Keywords><Keywords>Cardiovascular Diseases</Keywords><Keywords>Case-Control Studies</Keywords><Keywords>Chromatography,High Pressure Liquid</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Exercise Test</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>metabolism</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Nitric Oxide</Keywords><Keywords>Nitric Oxide Synthase</Keywords><Keywords>pathology</Keywords><Keywords>Regression Analysis</Keywords><Keywords>Risk</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Turkey</Keywords><Reprint>Not in File</Reprint><Start_Page>545</Start_Page><End_Page>551</End_Page><Periodical>Coron.Artery Dis.</Periodical><Volume>18</Volume><Issue>7</Issue><Address>Department of Cardiology, Turkiye Yuksek Ihtisas Hospital, Ankara, Turkey. timurselcuk@hotmail.com</Address><Web_URL>PM:17925608</Web_URL><ZZ_JournalStdAbbrev><f name="System">Coron.Artery Dis.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Li</Author><Year>2007</Year><RecNum>2200</RecNum><IDText>Increased plasma C-reactive protein and interleukin-6 concentrations in patients with slow coronary flow</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2200</Ref_ID><Title_Primary>Increased plasma C-reactive protein and interleukin-6 concentrations in patients with slow coronary flow</Title_Primary><Authors_Primary>Li,J.J.</Authors_Primary><Authors_Primary>Qin,X.W.</Authors_Primary><Authors_Primary>Li,Z.C.</Authors_Primary><Authors_Primary>Zeng,H.S.</Authors_Primary><Authors_Primary>Gao,Z.</Authors_Primary><Authors_Primary>Xu,B.</Authors_Primary><Authors_Primary>Zhang,C.Y.</Authors_Primary><Authors_Primary>Li,J.</Authors_Primary><Date_Primary>2007/10</Date_Primary><Keywords>Angiography</Keywords><Keywords>Arteries</Keywords><Keywords>C-Reactive Protein</Keywords><Keywords>Cardiology</Keywords><Keywords>China</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Inflammation</Keywords><Keywords>Interleukin-6</Keywords><Keywords>methods</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Plasma</Keywords><Keywords>Thrombosis</Keywords><Reprint>Not in File</Reprint><Start_Page>43</Start_Page><End_Page>47</End_Page><Periodical>Clin.Chim.Acta</Periodical><Volume>385</Volume><Issue>1-2</Issue><Address>Department of Cardiology, Fu Wai Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing 100037, People's Republic of China</Address><Web_URL>PM:17706955</Web_URL><ZZ_JournalStdAbbrev><f name="System">Clin.Chim.Acta</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[35-39]. Several pharmacological and mechanical therapies have been suggested for the management of no-reflow ADDIN REFMGR.CITE <Refman><Author>Eeckhout</Author><Year>2001</Year><RecNum>148</RecNum><IDText>The coronary no-reflow: a review of mechanisms and therapies.</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>148</Ref_ID><Title_Primary>The coronary no-reflow: a review of mechanisms and therapies.</Title_Primary><Authors_Primary>Eeckhout,E</Authors_Primary><Authors_Primary>Kern,Morton J.M.</Authors_Primary><Date_Primary>2001</Date_Primary><Reprint>In File</Reprint><Start_Page>729</Start_Page><End_Page>739</End_Page><Periodical>European Heart Journal</Periodical><Volume>22</Volume><ZZ_JournalFull><f name="System">European Heart Journal</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[40]. Intracoronary (IC) pharmacotherapy used to treat no-reflow during PCI following an acute myocardial infarction is discussed in this section.
Intracoronary verapamil
Taniyama and colleagues determined the benefit of intracoronary administration of verapamil among forty patients with acute ST elevation myocardial infarction during primary PTCA ADDIN REFMGR.CITE <Refman><Author>Taniyama</Author><Year>1997</Year><RecNum>207</RecNum><IDText>Beneficial effect of intracoronary verapamil on microvascular and myocardial salvage in patients with acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>207</Ref_ID><Title_Primary>Beneficial effect of intracoronary verapamil on microvascular and myocardial salvage in patients with acute myocardial infarction</Title_Primary><Authors_Primary>Taniyama,Y.</Authors_Primary><Authors_Primary>Ito,H.</Authors_Primary><Authors_Primary>Iwakura,K.</Authors_Primary><Authors_Primary>Masuyama,T.</Authors_Primary><Authors_Primary>Hori,M.</Authors_Primary><Authors_Primary>Takiuchi,S.</Authors_Primary><Authors_Primary>Nishikawa,N.</Authors_Primary><Authors_Primary>Higashino,Y.</Authors_Primary><Authors_Primary>Fujii,K.</Authors_Primary><Authors_Primary>Minamino,T.</Authors_Primary><Date_Primary>1997/11/1</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Echocardiography</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Injections,Intra-Arterial</Keywords><Keywords>Japan</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>pharmacology</Keywords><Keywords>physiopathology</Keywords><Keywords>Regional Blood Flow</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Vasodilator Agents</Keywords><Keywords>Ventricular Function,Left</Keywords><Keywords>Verapamil</Keywords><Reprint>Not in File</Reprint><Start_Page>1193</Start_Page><End_Page>1199</End_Page><Periodical>J Am.Coll.Cardiol.</Periodical><Volume>30</Volume><Issue>5</Issue><Address>Division of Cardiology, Sakurabashi Watanabe Hospital, Osaka, Japan</Address><Web_URL>PM:9350914</Web_URL><ZZ_JournalStdAbbrev><f name="System">J Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[41]. Of these 20 patients received intracoronary verapamil and the remaining 20 were control patients. All patients underwent myocardial contrast echocardiography (MCE) with intracoronary injection of sonicated microbubbles. Following the administration of verapamil the low reflow zone reduced from 0.39±0.23 to 0.29±0.17 (p<0.05) and the peak intensity increased from 6±5 to 12±6. The administration of intracoronary verapamil was also associated with greater reduction in the wall motion score from day 1 to day 24 compared to the control group (0.7±0.8 vs. 0.2±1.3 (p<0.05).
Intracoronary nicorandil
A study by Ota et al demonstrated that combined intravenous and intracoronary administration of nicorandil reduces reperfusion injury during PCI and improves the corrected TFC and ST segment resolution in acute myocardial infarction, and appears to be preferable to intracoronary administration alone. In their study, 0.5 mg per dose (1–2 mg in total) of nicorandil was administered into the coronary artery 1–2 times before and after percutaneous coronary intervention (PCI) balloon inflation. For intravenous administration, 4mg of nicorandil was injected, followed by a continuous drip infusion of 6ml/h (≈6mg/h) ADDIN REFMGR.CITE <Refman><Author>Ota</Author><Year>2006</Year><RecNum>1880</RecNum><IDText>Impact of nicorandil to prevent reperfusion injury in patients with acute myocardial infarction: Sigmart Multicenter Angioplasty Revascularization Trial (SMART)</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1880</Ref_ID><Title_Primary>Impact of nicorandil to prevent reperfusion injury in patients with acute myocardial infarction: Sigmart Multicenter Angioplasty Revascularization Trial (SMART)</Title_Primary><Authors_Primary>Ota,S.</Authors_Primary><Authors_Primary>Nishikawa,H.</Authors_Primary><Authors_Primary>Takeuchi,M.</Authors_Primary><Authors_Primary>Nakajima,K.</Authors_Primary><Authors_Primary>Nakamura,T.</Authors_Primary><Authors_Primary>Okamoto,S.</Authors_Primary><Authors_Primary>Setsuda,M.</Authors_Primary><Authors_Primary>Makino,K.</Authors_Primary><Authors_Primary>Yamakado,T.</Authors_Primary><Authors_Primary>Nakano,T.</Authors_Primary><Date_Primary>2006/9</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>adverse effects</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arrhythmia</Keywords><Keywords>Chest Pain</Keywords><Keywords>complications</Keywords><Keywords>drug effects</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>injuries</Keywords><Keywords>Japan</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion Injury</Keywords><Keywords>Nicorandil</Keywords><Keywords>Pain</Keywords><Keywords>prevention & control</Keywords><Keywords>Recovery of Function</Keywords><Keywords>Reperfusion</Keywords><Keywords>Reperfusion Injury</Keywords><Keywords>therapy</Keywords><Keywords>Vasodilator Agents</Keywords><Reprint>Not in File</Reprint><Start_Page>1099</Start_Page><End_Page>1104</End_Page><Periodical>Circ.J.</Periodical><Volume>70</Volume><Issue>9</Issue><Address>First Department of Internal Medicine, Mie University School of Medicine, Japan. satoshio@clin.medic.mie-u.ac.jp</Address><Web_URL>PM:16936418</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circ.J.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[42].
Intracoronary adenosine
More recently, Stoel and colleagues have demonstrated that high dose adenosine (60mg) administered into the coronary arteries during PCI (all patients received stents and abciximab) following an acute myocardial infarction resulted in better mean ST segment resolution (35.4% vs. 23% placebo, p<0.05), improved TIMI frame count (15.7 vs. 30.2, p<0.005), improved myocardial blush grades (2.7 vs. 2, p<0.05) and coronary resistance index (0.7 vs. 1.31 mm Hg per ml/min, p<0.005) ADDIN REFMGR.CITE <Refman><Author>Stoel</Author><Year>2008</Year><RecNum>1918</RecNum><IDText>High dose adenosine for suboptimal myocardial reperfusion after primary PCI: A randomized placebo-controlled pilot study</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1918</Ref_ID><Title_Primary>High dose adenosine for suboptimal myocardial reperfusion after primary PCI: A randomized placebo-controlled pilot study</Title_Primary><Authors_Primary>Stoel,M.G.</Authors_Primary><Authors_Primary>Marques,K.M.</Authors_Primary><Authors_Primary>de Cock,C.C.</Authors_Primary><Authors_Primary>Bronzwaer,J.G.</Authors_Primary><Authors_Primary>von,Birgelen C.</Authors_Primary><Authors_Primary>Zijlstra,F.</Authors_Primary><Date_Primary>2008/2/15</Date_Primary><Keywords>Adenosine</Keywords><Keywords>Cardiology</Keywords><Keywords>Infarction</Keywords><Keywords>methods</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Netherlands</Keywords><Keywords>Perfusion</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Reperfusion</Keywords><Keywords>Stents</Keywords><Reprint>Not in File</Reprint><Start_Page>283</Start_Page><End_Page>289</End_Page><Periodical>Catheter.Cardiovasc.Interv.</Periodical><Volume>71</Volume><Issue>3</Issue><Address>Department of Cardiology, Medisch Spectrum Twente, Enschede, the Netherlands. m.stoel@ziekenhuis-mst.nl</Address><Web_URL>PM:17985384</Web_URL><ZZ_JournalStdAbbrev><f name="System">Catheter.Cardiovasc.Interv.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[43].
Intracoronary glycoprotein IIb/IIIa inhibitors
It has been postulated that local administration of abciximab would enhance the diffusion of antibodies to platelets inside the thrombus within the coronary arteries as a result of an increase in the concentration of abciximab during local delivery than during IV administration [280:1 (minimal washout) vs. 1:1 (normal flow)] ADDIN REFMGR.CITE <Refman><Author>Wohrle</Author><Year>2003</Year><RecNum>1919</RecNum><IDText>Reduction of major adverse cardiac events with intracoronary compared with intravenous bolus application of abciximab in patients with acute myocardial infarction or unstable angina undergoing coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1919</Ref_ID><Title_Primary>Reduction of major adverse cardiac events with intracoronary compared with intravenous bolus application of abciximab in patients with acute myocardial infarction or unstable angina undergoing coronary angioplasty</Title_Primary><Authors_Primary>Wohrle,J.</Authors_Primary><Authors_Primary>Grebe,O.C.</Authors_Primary><Authors_Primary>Nusser,T.</Authors_Primary><Authors_Primary>Al-Khayer,E.</Authors_Primary><Authors_Primary>Schaible,S.</Authors_Primary><Authors_Primary>Kochs,M.</Authors_Primary><Authors_Primary>Hombach,V.</Authors_Primary><Authors_Primary>Hoher,M.</Authors_Primary><Date_Primary>2003/4/15</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>adverse effects</Keywords><Keywords>analysis</Keywords><Keywords>Angina,Unstable</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Clinical Trials</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Disease</Keywords><Keywords>Diabetes Mellitus</Keywords><Keywords>drug therapy</Keywords><Keywords>Emergencies</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Germany</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Infusions,Intravenous</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>prevention & control</Keywords><Keywords>Recurrence</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>Shock</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Reprint>Not in File</Reprint><Start_Page>1840</Start_Page><End_Page>1843</End_Page><Periodical>Circulation</Periodical><Volume>107</Volume><Issue>14</Issue><Address>Internal-Medicine-II, University of Ulm, Robert-Koch-Strasse-8, 89081 Ulm, Germany</Address><Web_URL>PM:12682003</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Romagnoli</Author><Year>2007</Year><RecNum>1967</RecNum><IDText>Rationale for intracoronary administration of abciximab</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1967</Ref_ID><Title_Primary>Rationale for intracoronary administration of abciximab</Title_Primary><Authors_Primary>Romagnoli,E.</Authors_Primary><Authors_Primary>Burzotta,F.</Authors_Primary><Authors_Primary>Trani,C.</Authors_Primary><Authors_Primary>Biondi-Zoccai,G.G.</Authors_Primary><Authors_Primary>Giannico,F.</Authors_Primary><Authors_Primary>Crea,F.</Authors_Primary><Date_Primary>2007/2</Date_Primary><Keywords>Acute Coronary Syndrome</Keywords><Keywords>administration & dosage</Keywords><Keywords>adverse effects</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>Drug Administration Routes</Keywords><Keywords>drug therapy</Keywords><Keywords>Endothelium</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Italy</Keywords><Keywords>Leukocytes</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>pharmacology</Keywords><Keywords>Platelet Aggregation</Keywords><Keywords>Platelet Aggregation Inhibitors</Keywords><Keywords>prevention & control</Keywords><Keywords>Randomized Controlled Trials</Keywords><Keywords>Syndrome</Keywords><Keywords>Thrombosis</Keywords><Keywords>Ventricular Function</Keywords><Reprint>Not in File</Reprint><Start_Page>57</Start_Page><End_Page>63</End_Page><Periodical>J.Thromb.Thrombolysis.</Periodical><Volume>23</Volume><Issue>1</Issue><Address>Department of cardiovascular disease, Catholic University, Campobasso, Italy. enromagnolimd@hotmail.com</Address><Web_URL>PM:17160551</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Thromb.Thrombolysis.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[44;45]. High local concentration might also enhance the anti-inflammatory properties of abciximab such as the anti-inflammatory effects from cross-reactivity with the leukocyte αMβ2 integrin and inhibition of the vitronectin receptors in the endothelial cells in the culprit vessel ADDIN REFMGR.CITE <Refman><Author>Simon</Author><Year>1997</Year><RecNum>2523</RecNum><IDText>7E3 monoclonal antibody directed against the platelet glycoprotein IIb/IIIa cross-reacts with the leukocyte integrin Mac-1 and blocks adhesion to fibrinogen and ICAM-1</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2523</Ref_ID><Title_Primary>7E3 monoclonal antibody directed against the platelet glycoprotein IIb/IIIa cross-reacts with the leukocyte integrin Mac-1 and blocks adhesion to fibrinogen and ICAM-1</Title_Primary><Authors_Primary>Simon,D.I.</Authors_Primary><Authors_Primary>Xu,H.</Authors_Primary><Authors_Primary>Ortlepp,S.</Authors_Primary><Authors_Primary>Rogers,C.</Authors_Primary><Authors_Primary>Rao,N.K.</Authors_Primary><Date_Primary>1997/3</Date_Primary><Keywords>Acute Coronary Syndrome</Keywords><Keywords>Angioplasty</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>blood</Keywords><Keywords>Cell Adhesion</Keywords><Keywords>Cell Line</Keywords><Keywords>Clinical Trials</Keywords><Keywords>complications</Keywords><Keywords>Cross Reactions</Keywords><Keywords>cytology</Keywords><Keywords>drug effects</Keywords><Keywords>Fibrinogen</Keywords><Keywords>Flow Cytometry</Keywords><Keywords>Humans</Keywords><Keywords>immunology</Keywords><Keywords>injuries</Keywords><Keywords>Intercellular Adhesion Molecule-1</Keywords><Keywords>Macrophage-1 Antigen</Keywords><Keywords>metabolism</Keywords><Keywords>Monocytes</Keywords><Keywords>Neutrophils</Keywords><Keywords>pharmacology</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>Research</Keywords><Keywords>Syndrome</Keywords><Reprint>Not in File</Reprint><Start_Page>528</Start_Page><End_Page>535</End_Page><Periodical>Arterioscler.Thromb.Vasc.Biol.</Periodical><Volume>17</Volume><Issue>3</Issue><Address>Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. disimon@bics.bwh.harvard.edu</Address><Web_URL>PM:9102172</Web_URL><ZZ_JournalStdAbbrev><f name="System">Arterioscler.Thromb.Vasc.Biol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[46]. These effects on the platelets and on the coronary endothelial cells result in reduced reperfusion injury and a greater degree of myocardial salvage ADDIN REFMGR.CITE <Refman><Author>Kintscher</Author><Year>2000</Year><RecNum>2524</RecNum><IDText>Effects of abciximab and tirofiban on vitronectin receptors in human endothelial and smooth muscle cells</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2524</Ref_ID><Title_Primary>Effects of abciximab and tirofiban on vitronectin receptors in human endothelial and smooth muscle cells</Title_Primary><Authors_Primary>Kintscher,U.</Authors_Primary><Authors_Primary>Kappert,K.</Authors_Primary><Authors_Primary>Schmidt,G.</Authors_Primary><Authors_Primary>Doerr,G.</Authors_Primary><Authors_Primary>Grill,M.</Authors_Primary><Authors_Primary>Wollert-Wulf,B.</Authors_Primary><Authors_Primary>Graefe,M.</Authors_Primary><Authors_Primary>Fleck,E.</Authors_Primary><Authors_Primary>Graf,K.</Authors_Primary><Date_Primary>2000/2/25</Date_Primary><Keywords>analogs & derivatives</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>biosynthesis</Keywords><Keywords>Cell Adhesion</Keywords><Keywords>cytology</Keywords><Keywords>drug effects</Keywords><Keywords>Endothelium</Keywords><Keywords>Endothelium,Vascular</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Flow Cytometry</Keywords><Keywords>genetics</Keywords><Keywords>Germany</Keywords><Keywords>Humans</Keywords><Keywords>Iliac Artery</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Immunohistochemistry</Keywords><Keywords>Integrins</Keywords><Keywords>isolation & purification</Keywords><Keywords>metabolism</Keywords><Keywords>Muscle,Smooth,Vascular</Keywords><Keywords>Oligopeptides</Keywords><Keywords>pharmacology</Keywords><Keywords>Receptors,Vitronectin</Keywords><Keywords>Research</Keywords><Keywords>Reverse Transcriptase Polymerase Chain Reaction</Keywords><Keywords>Tyrosine</Keywords><Keywords>Umbilical Veins</Keywords><Keywords>Vitronectin</Keywords><Reprint>Not in File</Reprint><Start_Page>75</Start_Page><End_Page>87</End_Page><Periodical>Eur.J.Pharmacol.</Periodical><Volume>390</Volume><Issue>1-2</Issue><Address>Department of Medicine/Cardiology, Charite, Campus Virchow Klinikum, Humboldt Universitat Berlin and Deutsches Herzzentrum Berlin, Augustenburger Platz 1, D-13353, Berlin, Germany</Address><Web_URL>PM:10708709</Web_URL><ZZ_JournalStdAbbrev><f name="System">Eur.J.Pharmacol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[47].
The beneficial effect of intracoronary abciximab was studied by Wohrle and colleagues ADDIN REFMGR.CITE <Refman><Author>Wohrle</Author><Year>2003</Year><RecNum>1919</RecNum><IDText>Reduction of major adverse cardiac events with intracoronary compared with intravenous bolus application of abciximab in patients with acute myocardial infarction or unstable angina undergoing coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1919</Ref_ID><Title_Primary>Reduction of major adverse cardiac events with intracoronary compared with intravenous bolus application of abciximab in patients with acute myocardial infarction or unstable angina undergoing coronary angioplasty</Title_Primary><Authors_Primary>Wohrle,J.</Authors_Primary><Authors_Primary>Grebe,O.C.</Authors_Primary><Authors_Primary>Nusser,T.</Authors_Primary><Authors_Primary>Al-Khayer,E.</Authors_Primary><Authors_Primary>Schaible,S.</Authors_Primary><Authors_Primary>Kochs,M.</Authors_Primary><Authors_Primary>Hombach,V.</Authors_Primary><Authors_Primary>Hoher,M.</Authors_Primary><Date_Primary>2003/4/15</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>adverse effects</Keywords><Keywords>analysis</Keywords><Keywords>Angina,Unstable</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Clinical Trials</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Disease</Keywords><Keywords>Diabetes Mellitus</Keywords><Keywords>drug therapy</Keywords><Keywords>Emergencies</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Germany</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Infusions,Intravenous</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>prevention & control</Keywords><Keywords>Recurrence</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>Shock</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Reprint>Not in File</Reprint><Start_Page>1840</Start_Page><End_Page>1843</End_Page><Periodical>Circulation</Periodical><Volume>107</Volume><Issue>14</Issue><Address>Internal-Medicine-II, University of Ulm, Robert-Koch-Strasse-8, 89081 Ulm, Germany</Address><Web_URL>PM:12682003</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[44]. In a study of 403 patients, 294 received intracoronary abciximab and 109 patients received intravenous abciximab (20mg bolus followed by 10mg infusion for 12 hours). The 30 day major adverse cardiac events (death, myocardial infarction and urgent revascularization) were significantly reduced in the IC group compared to the IV group (10.2% vs. 20.2%, p<0.008). The benefit was more evident among those who had TIMI flow grade 0/1 prior to the PCI procedure (11.8% vs. 27.5%, p<0.02).
A retrospective analysis of 59 patients undergoing PPCI demonstrated the feasibility and efficacy of intracoronary and intravenous eptifibatide. There was an increase in the final TIMI myocardial perfusion grade 3 (54%) with the administration of eptifibatide ADDIN REFMGR.CITE <Refman><Author>Pinto</Author><Year>2005</Year><RecNum>186</RecNum><IDText>Administration of intracoronary eptifibatide during ST-elevation myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>186</Ref_ID><Title_Primary>Administration of intracoronary eptifibatide during ST-elevation myocardial infarction</Title_Primary><Authors_Primary>Pinto,D.S.</Authors_Primary><Authors_Primary>Kirtane,A.J.</Authors_Primary><Authors_Primary>Ruocco,N.A.</Authors_Primary><Authors_Primary>Deibele,A.J.</Authors_Primary><Authors_Primary>Shui,A.</Authors_Primary><Authors_Primary>Buros,J.</Authors_Primary><Authors_Primary>Murphy,S.A.</Authors_Primary><Authors_Primary>Gibson,C.M.</Authors_Primary><Date_Primary>2005/12/1</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Aged</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Arrhythmia</Keywords><Keywords>Boston</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug therapy</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Injections,Intra-Arterial</Keywords><Keywords>Male</Keywords><Keywords>Massachusetts</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Peptides</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>radiography</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>Safety</Keywords><Keywords>therapeutic use</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>1494</Start_Page><End_Page>1497</End_Page><Periodical>Am.J.Cardiol.</Periodical><Volume>96</Volume><Issue>11</Issue><Address>Beth Israel Deaconess Medical Center, Division of Cardiology, Boston, Massachusetts, USA</Address><Web_URL>PM:16310428</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.J.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[48]. This study was small and retrospective without a control group and hence further ongoing randomized studies will provide a definitive answer on the role of intracoronary eptifibatide administration in improving microvascular function.
Intracoronary thrombolytic
In addition to the drugs mentioned previously and the beneficial effects of intracoronary glycoprotein IIb/IIIa inhibitors, the beneficial effects of intracoronary administration of fibrinolytic were determined among patients undergoing primary PCI by Sezer and colleagues. A total of 41 patients were randomized to undergo PCI with or without IC streptokinase. Two days following the procedure, patients who had IC SK had significantly better coronary flow reserve (2.01±0.57 vs. 1.39±0.31), index of microvascular resistance (16.29±5.06 U vs. 32.49±11.04 U), collateral flow index, mean coronary wedge pressure, systolic wedge pressure and diastolic deceleration time compared to the control group ADDIN REFMGR.CITE <Refman><Author>Sezer</Author><Year>2007</Year><RecNum>1792</RecNum><IDText>Intracoronary streptokinase after primary percutaneous coronary intervention</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1792</Ref_ID><Title_Primary>Intracoronary streptokinase after primary percutaneous coronary intervention</Title_Primary><Authors_Primary>Sezer,M.</Authors_Primary><Authors_Primary>Oflaz,H.</Authors_Primary><Authors_Primary>Goren,T.</Authors_Primary><Authors_Primary>Okcular,I.</Authors_Primary><Authors_Primary>Umman,B.</Authors_Primary><Authors_Primary>Nisanci,Y.</Authors_Primary><Authors_Primary>Bilge,A.K.</Authors_Primary><Authors_Primary>Sanli,Y.</Authors_Primary><Authors_Primary>Meric,M.</Authors_Primary><Authors_Primary>Umman,S.</Authors_Primary><Date_Primary>2007/5/3</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Blood Pressure</Keywords><Keywords>Capillary Resistance</Keywords><Keywords>Catheterization</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Echocardiography</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Heart Ventricles</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Microcirculation</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>pathology</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Pilot Projects</Keywords><Keywords>Pressure</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Streptokinase</Keywords><Keywords>therapy</Keywords><Keywords>Thrombosis</Keywords><Keywords>Time</Keywords><Keywords>Turkey</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1823</Start_Page><End_Page>1834</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>356</Volume><Issue>18</Issue><Address>Istanbul Faculty of Medicine, Istanbul University, Istanbul, Turkey. sezerm@istanbul.edu.tr</Address><Web_URL>PM:17476008</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[49]. However, there was no difference in the left ventricular size and function at 6 months.
Adjunctive anti-embolic devices
In addition to pharmacotherapy, several thrombus extraction ADDIN REFMGR.CITE <Refman><Author>Beran</Author><Year>2002</Year><RecNum>139</RecNum><IDText>Intracoronary thrombectomy with the X-sizer catheter system improves epicardial flow and accelerates ST-segment resolution in patients with acute coronary syndrome: a prospective, randomized, controlled study</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>139</Ref_ID><Title_Primary>Intracoronary thrombectomy with the X-sizer catheter system improves epicardial flow and accelerates ST-segment resolution in patients with acute coronary syndrome: a prospective, randomized, controlled study</Title_Primary><Authors_Primary>Beran,G.</Authors_Primary><Authors_Primary>Lang,I.</Authors_Primary><Authors_Primary>Schreiber,W.</Authors_Primary><Authors_Primary>Denk,S.</Authors_Primary><Authors_Primary>Stefenelli,T.</Authors_Primary><Authors_Primary>Syeda,B.</Authors_Primary><Authors_Primary>Maurer,G.</Authors_Primary><Authors_Primary>Glogar,D.</Authors_Primary><Authors_Primary>Siostrzonek,P.</Authors_Primary><Date_Primary>2002/5/21</Date_Primary><Keywords>Acute Disease</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Arteriosclerosis</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Embolism</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>instrumentation</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Microcirculation</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Odds Ratio</Keywords><Keywords>physiopathology</Keywords><Keywords>prevention & control</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Rheology</Keywords><Keywords>surgery</Keywords><Keywords>Syndrome</Keywords><Keywords>Thrombectomy</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>2355</Start_Page><End_Page>2360</End_Page><Periodical>Circulation</Periodical><Volume>105</Volume><Issue>20</Issue><Address>Department of Cardiology and Emergency Medicine University of Vienna, Vienna, Austria</Address><Web_URL>PM:12021220</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Dudek</Author><Year>2004</Year><RecNum>319</RecNum><IDText>Percutaneous thrombectomy with the RESCUE system in acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>319</Ref_ID><Title_Primary>Percutaneous thrombectomy with the RESCUE system in acute myocardial infarction</Title_Primary><Authors_Primary>Dudek,D.</Authors_Primary><Authors_Primary>Mielecki,W.</Authors_Primary><Authors_Primary>Legutko,J.</Authors_Primary><Authors_Primary>Chyrchel,M.</Authors_Primary><Authors_Primary>Sorysz,D.</Authors_Primary><Authors_Primary>Bartus,S.</Authors_Primary><Authors_Primary>Rzeszutko,L.</Authors_Primary><Authors_Primary>Dubiel,J.S.</Authors_Primary><Date_Primary>2004/12</Date_Primary><Keywords>Arteries</Keywords><Keywords>Atherectomy,Coronary</Keywords><Keywords>blood</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Artery Bypass</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>instrumentation</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Microcirculation</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>physiopathology</Keywords><Keywords>Poland</Keywords><Keywords>radiography</Keywords><Keywords>Safety</Keywords><Keywords>Stroke Volume</Keywords><Keywords>therapy</Keywords><Keywords>Thrombectomy</Keywords><Keywords>Time</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>523</Start_Page><End_Page>533</End_Page><Periodical>Kardiol.Pol.</Periodical><Volume>61</Volume><Issue>12</Issue><Address>2nd Department of Cardiology, Institute of Cardiology, Collegium Medicum, Jagiellonian University, Cracow, Poland</Address><Web_URL>PM:15815753</Web_URL><ZZ_JournalStdAbbrev><f name="System">Kardiol.Pol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Vijayalakshmi</Author><Year>2006</Year><RecNum>1629</RecNum><IDText>Successful thrombus extraction with the Rescue thrombus management system during acute percutaneous coronary intervention improves flow but does not necessarily restore optimal myocardial tissue perfusion</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1629</Ref_ID><Title_Primary>Successful thrombus extraction with the Rescue thrombus management system during acute percutaneous coronary intervention improves flow but does not necessarily restore optimal myocardial tissue perfusion</Title_Primary><Authors_Primary>Vijayalakshmi,K.</Authors_Primary><Authors_Primary>Kunadian,B.</Authors_Primary><Authors_Primary>Wright,R.A.</Authors_Primary><Authors_Primary>Sutton,A.G.</Authors_Primary><Authors_Primary>Hall,J.A.</Authors_Primary><Authors_Primary>de Belder,M.A.</Authors_Primary><Date_Primary>2006/6</Date_Primary><Keywords>Acute Coronary Syndrome</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Atherectomy,Coronary</Keywords><Keywords>blood</Keywords><Keywords>Cardiology</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>Embolism</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>prevention & control</Keywords><Keywords>radiography</Keywords><Keywords>Stents</Keywords><Keywords>Syndrome</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Vascular Patency</Keywords><Reprint>Not in File</Reprint><Start_Page>879</Start_Page><End_Page>886</End_Page><Periodical>Catheter.Cardiovasc.Interv.</Periodical><Volume>67</Volume><Issue>6</Issue><Address>Department of Cardiology, the James Cook University Hospital, Middlesbrough, United Kingdom</Address><Web_URL>PM:16652368</Web_URL><ZZ_JournalStdAbbrev><f name="System">Catheter.Cardiovasc.Interv.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Silva-Orrego</Author><Year>2006</Year><RecNum>1180</RecNum><IDText>Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction) study</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1180</Ref_ID><Title_Primary>Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction) study</Title_Primary><Authors_Primary>Silva-Orrego,P.</Authors_Primary><Authors_Primary>Colombo,P.</Authors_Primary><Authors_Primary>Bigi,R.</Authors_Primary><Authors_Primary>Gregori,D.</Authors_Primary><Authors_Primary>Delgado,A.</Authors_Primary><Authors_Primary>Salvade,P.</Authors_Primary><Authors_Primary>Oreglia,J.</Authors_Primary><Authors_Primary>Orrico,P.</Authors_Primary><Authors_Primary>de,Biase A.</Authors_Primary><Authors_Primary>Piccalo,G.</Authors_Primary><Authors_Primary>Bossi,I.</Authors_Primary><Authors_Primary>Klugmann,S.</Authors_Primary><Date_Primary>2006/10/17</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Catheterization</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>Creatine Kinase</Keywords><Keywords>diagnosis</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Equipment Design</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>instrumentation</Keywords><Keywords>Italy</Keywords><Keywords>methods</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>radiography</Keywords><Keywords>Risk</Keywords><Keywords>Shock</Keywords><Keywords>Single-Blind Method</Keywords><Keywords>standards</Keywords><Keywords>Suction</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>1552</Start_Page><End_Page>1559</End_Page><Periodical>J.Am.Coll.Cardiol.</Periodical><Volume>48</Volume><Issue>8</Issue><Address>Interventional Cardiology, A. De Gasperis Department, Niguarda Hospital, Milan, Italy. pedrosilva@tiscali.it</Address><Web_URL>PM:17045887</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Lefevre</Author><Year>2005</Year><RecNum>192</RecNum><IDText>X-sizer for thrombectomy in acute myocardial infarction improves ST-segment resolution: results of the X-sizer in AMI for negligible embolization and optimal ST resolution (X AMINE ST) trial</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>192</Ref_ID><Title_Primary>X-sizer for thrombectomy in acute myocardial infarction improves ST-segment resolution: results of the X-sizer in AMI for negligible embolization and optimal ST resolution (X AMINE ST) trial</Title_Primary><Authors_Primary>Lefevre,T.</Authors_Primary><Authors_Primary>Garcia,E.</Authors_Primary><Authors_Primary>Reimers,B.</Authors_Primary><Authors_Primary>Lang,I.</Authors_Primary><Authors_Primary>di,Mario C.</Authors_Primary><Authors_Primary>Colombo,A.</Authors_Primary><Authors_Primary>Neumann,F.J.</Authors_Primary><Authors_Primary>Chavarri,M.V.</Authors_Primary><Authors_Primary>Brunel,P.</Authors_Primary><Authors_Primary>Grube,E.</Authors_Primary><Authors_Primary>Thomas,M.</Authors_Primary><Authors_Primary>Glatt,B.</Authors_Primary><Authors_Primary>Ludwig,J.</Authors_Primary><Date_Primary>2005/7/19</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart Catheterization</Keywords><Keywords>Humans</Keywords><Keywords>instrumentation</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Platelet Glycoprotein GPIIb-IIIa Complex</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Risk</Keywords><Keywords>Stents</Keywords><Keywords>surgery</Keywords><Keywords>Thrombectomy</Keywords><Keywords>Time Factors</Keywords><Reprint>Not in File</Reprint><Start_Page>246</Start_Page><End_Page>252</End_Page><Periodical>J Am.Coll.Cardiol.</Periodical><Volume>46</Volume><Issue>2</Issue><Address>Institut Cardiovasculaire Paris Sud, Massy, France. t.lefevre@icps.com.fr</Address><Web_URL>PM:16022950</Web_URL><ZZ_JournalStdAbbrev><f name="System">J Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[50-54], proximal ADDIN REFMGR.CITE <Refman><Author>Koch</Author><Year>2007</Year><RecNum>2529</RecNum><IDText>Proximal Embolic Protection With Aspiration in Percutaneous Corononary Intervention Using the Proxistrade mark Device</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2529</Ref_ID><Title_Primary>Proximal Embolic Protection With Aspiration in Percutaneous Corononary Intervention Using the Proxistrade mark Device</Title_Primary><Authors_Primary>Koch,K.T.</Authors_Primary><Authors_Primary>Haeck,J.D.</Authors_Primary><Authors_Primary>Van Der Schaaf,R.J.</Authors_Primary><Authors_Primary>Alidjan,F.M.</Authors_Primary><Authors_Primary>Henriques,J.P.</Authors_Primary><Authors_Primary>Baan,J.,Jr.</Authors_Primary><Authors_Primary>Piek,J.J.</Authors_Primary><Authors_Primary>Van Der Wal,A.C.</Authors_Primary><Authors_Primary>Tijssen,J.G.</Authors_Primary><Authors_Primary>Sutsch,G.</Authors_Primary><Authors_Primary>de Winter,R.J.</Authors_Primary><Date_Primary>2007</Date_Primary><Keywords>Cardiology</Keywords><Keywords>Infarction</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Netherlands</Keywords><Keywords>Prognosis</Keywords><Keywords>Registries</Keywords><Reprint>Not in File</Reprint><Start_Page>160</Start_Page><End_Page>166</End_Page><Periodical>Rev.Cardiovasc.Med.</Periodical><Volume>8</Volume><Issue>3</Issue><Address>Department of Cardiology, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands</Address><Web_URL>PM:17938616</Web_URL><ZZ_JournalStdAbbrev><f name="System">Rev.Cardiovasc.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[55] and distal protection devices ADDIN REFMGR.CITE <Refman><Author>Bartorelli</Author><Year>1999</Year><RecNum>2286</RecNum><IDText>Successful dissolution of occlusive coronary thrombus with local administration of abciximab during PTCA</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2286</Ref_ID><Title_Primary>Successful dissolution of occlusive coronary thrombus with local administration of abciximab during PTCA</Title_Primary><Authors_Primary>Bartorelli,A.L.</Authors_Primary><Authors_Primary>Trabattoni,D.</Authors_Primary><Authors_Primary>Galli,S.</Authors_Primary><Authors_Primary>Grancini,L.</Authors_Primary><Authors_Primary>Cozzi,S.</Authors_Primary><Authors_Primary>Ravagnani,P.</Authors_Primary><Date_Primary>1999/10</Date_Primary><Keywords>administration & dosage</Keywords><Keywords>Administration,Topical</Keywords><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Anticoagulants</Keywords><Keywords>Cardiology</Keywords><Keywords>complications</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>drug therapy</Keywords><Keywords>Female</Keywords><Keywords>Heart Catheterization</Keywords><Keywords>Humans</Keywords><Keywords>Immunoglobulin Fab Fragments</Keywords><Keywords>instrumentation</Keywords><Keywords>Italy</Keywords><Keywords>radiography</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>211</Start_Page><End_Page>213</End_Page><Periodical>Catheter.Cardiovasc.Interv.</Periodical><Volume>48</Volume><Issue>2</Issue><Address>Institute of Cardiology, the University of Milan, Fondazione "Monzino" IRCCS, Milan, Italy</Address><Web_URL>PM:10506783</Web_URL><ZZ_JournalStdAbbrev><f name="System">Catheter.Cardiovasc.Interv.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Stone</Author><Year>2005</Year><RecNum>185</RecNum><IDText>Distal Microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>185</Ref_ID><Title_Primary>Distal Microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction</Title_Primary><Authors_Primary>Stone,G</Authors_Primary><Authors_Primary>Webb,J</Authors_Primary><Authors_Primary>Cox,D</Authors_Primary><Authors_Primary>Brodie,B</Authors_Primary><Authors_Primary>Quereshi,M</Authors_Primary><Authors_Primary>Lalynych,A</Authors_Primary><Authors_Primary>Turco,M</Authors_Primary><Authors_Primary>Schultheiss,HP</Authors_Primary><Authors_Primary>Dulas,D</Authors_Primary><Authors_Primary>Rutherford,BD</Authors_Primary><Authors_Primary>Antoniucci,D</Authors_Primary><Authors_Primary>Krucoff,MW</Authors_Primary><Authors_Primary>Gibbons,RJ</Authors_Primary><Authors_Primary>Jones,D</Authors_Primary><Authors_Primary>Lansky,A</Authors_Primary><Authors_Primary>Mehran,R</Authors_Primary><Authors_Primary>for the Enhanced Myocardial Efficacy and Recovery by Aspiration of Liberated Debris (EMERALD) Investigators</Authors_Primary><Date_Primary>2005</Date_Primary><Reprint>Not in File</Reprint><Start_Page>1063</Start_Page><End_Page>1072</End_Page><Periodical>JAMA</Periodical><Volume>293</Volume><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Limbruno</Author><Year>2003</Year><RecNum>115</RecNum><IDText>Mechanical prevention of distal embolization during primary angioplasty: safety, feasibility, and impact on myocardial reperfusion</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>115</Ref_ID><Title_Primary>Mechanical prevention of distal embolization during primary angioplasty: safety, feasibility, and impact on myocardial reperfusion</Title_Primary><Authors_Primary>Limbruno,U.</Authors_Primary><Authors_Primary>Micheli,A.</Authors_Primary><Authors_Primary>De,Carlo M.</Authors_Primary><Authors_Primary>Amoroso,G.</Authors_Primary><Authors_Primary>Rossini,R.</Authors_Primary><Authors_Primary>Palagi,C.</Authors_Primary><Authors_Primary>Di,Bello,V</Authors_Primary><Authors_Primary>Petronio,A.S.</Authors_Primary><Authors_Primary>Fontanini,G.</Authors_Primary><Authors_Primary>Mariani,M.</Authors_Primary><Date_Primary>2003/7/15</Date_Primary><Keywords>adverse effects</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Biological Markers</Keywords><Keywords>blood</Keywords><Keywords>complications</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>Echocardiography</Keywords><Keywords>Embolism</Keywords><Keywords>etiology</Keywords><Keywords>Feasibility Studies</Keywords><Keywords>Filtration</Keywords><Keywords>Humans</Keywords><Keywords>instrumentation</Keywords><Keywords>Italy</Keywords><Keywords>methods</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Patient Selection</Keywords><Keywords>prevention & control</Keywords><Keywords>Prostheses and Implants</Keywords><Keywords>Safety</Keywords><Keywords>surgery</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>171</Start_Page><End_Page>176</End_Page><Periodical>Circulation</Periodical><Volume>108</Volume><Issue>2</Issue><Address>Cardiac and Thoracic Department, University of Pisa, Pisa, Italy. ulimbru@tin.it</Address><Web_URL>PM:12835216</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[56-58] have been used during PPCI among patients with heavy thrombus burden in the infarct related arteries in order to minimize distal embolization. The largest study using a distal protection device during PPCI is the EMERALD trial (Enhanced Myocardial Efficacy and Recovery by Aspiration of Liberated Debris) by Stone and colleagues ADDIN REFMGR.CITE <Refman><Author>Stone</Author><Year>2005</Year><RecNum>185</RecNum><IDText>Distal Microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>185</Ref_ID><Title_Primary>Distal Microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction</Title_Primary><Authors_Primary>Stone,G</Authors_Primary><Authors_Primary>Webb,J</Authors_Primary><Authors_Primary>Cox,D</Authors_Primary><Authors_Primary>Brodie,B</Authors_Primary><Authors_Primary>Quereshi,M</Authors_Primary><Authors_Primary>Lalynych,A</Authors_Primary><Authors_Primary>Turco,M</Authors_Primary><Authors_Primary>Schultheiss,HP</Authors_Primary><Authors_Primary>Dulas,D</Authors_Primary><Authors_Primary>Rutherford,BD</Authors_Primary><Authors_Primary>Antoniucci,D</Authors_Primary><Authors_Primary>Krucoff,MW</Authors_Primary><Authors_Primary>Gibbons,RJ</Authors_Primary><Authors_Primary>Jones,D</Authors_Primary><Authors_Primary>Lansky,A</Authors_Primary><Authors_Primary>Mehran,R</Authors_Primary><Authors_Primary>for the Enhanced Myocardial Efficacy and Recovery by Aspiration of Liberated Debris (EMERALD) Investigators</Authors_Primary><Date_Primary>2005</Date_Primary><Reprint>Not in File</Reprint><Start_Page>1063</Start_Page><End_Page>1072</End_Page><Periodical>JAMA</Periodical><Volume>293</Volume><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[57]. This study consisted of 501 patients with STEMI from around 7 countries. In total 252 patients underwent PPCI using the distal protection device (PercuSurge, GuardWireTM Plus, Medtronic Inc. Calif.). Aspiration was performed in 97% of the cases and in 73% visible debris was aspirated. There was no difference in the primary endpoint of ST segment resolution at 30 minutes following the PCI (63.3% vs. 61.9%, p=0.78) and the infarct size between days 5 and 14 using Tc 99m Sestamibi scan (12% vs. 9.5%, p=0.15) between the groups that had PCI with and without the device respectively. This was associated with no difference in the major adverse cardiac events at 6 months between the two groups (10% vs. 11%, p=0.66).
A study using the thrombus extraction device during primary PCI was performed by Svilaas and colleagues called the TAPAS study (Thrombus Aspiration in Percutaneous coronary intervention following Acute myocardial infarction Study) consisting of 1071 patients with acute myocardial infarction from a single center. Of these, 535 patients were randomized following coronary angiography to thrombus extraction and 536 patients were randomized to conventional PPCI. Thrombus was aspirated in 72.9% of the cases which was confirmed on histopathological examinations. The major component of the aspirated debris consisted of platelets in 67.7% of cases and erythrocytes in 15.1% of patients. Patients randomized to thrombus extraction had significant improvement in the myocardial blush grades (Grade 0/1 17.1% versus 26.3%, p<0.001) and ST segment resolution (complete ST segment resolution in 56.6% versus 44.2%, p<0.001) compared to those who had conventional PPCI only. Of the patients who had better MBG and ST segment resolution had better clinical outcomes at 30 days. Impaired myocardial blush (Grade 0 or 1) was related to worse outcomes (14.1%) as compared to Grade 2 blush (8.8%) or Grade 3 blush (4.2%, p<0.001) ADDIN REFMGR.CITE <Refman><Author>Svilaas</Author><Year>2008</Year><RecNum>2541</RecNum><IDText>Thrombus aspiration during primary percutaneous coronary intervention</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2541</Ref_ID><Title_Primary>Thrombus aspiration during primary percutaneous coronary intervention</Title_Primary><Authors_Primary>Svilaas,T.</Authors_Primary><Authors_Primary>Vlaar,P.J.</Authors_Primary><Authors_Primary>van,der Horst,I</Authors_Primary><Authors_Primary>Diercks,G.F.</Authors_Primary><Authors_Primary>de Smet,B.J.</Authors_Primary><Authors_Primary>van den Heuvel,A.F.</Authors_Primary><Authors_Primary>Anthonio,R.L.</Authors_Primary><Authors_Primary>Jessurun,G.A.</Authors_Primary><Authors_Primary>Tan,E.S.</Authors_Primary><Authors_Primary>Suurmeijer,A.J.</Authors_Primary><Authors_Primary>Zijlstra,F.</Authors_Primary><Date_Primary>2008/2/7</Date_Primary><Keywords>adverse effects</Keywords><Keywords>Aged</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Cardiology</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>Death</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Heart Catheterization</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>instrumentation</Keywords><Keywords>Logistic Models</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Microcirculation</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Netherlands</Keywords><Keywords>pathology</Keywords><Keywords>physiopathology</Keywords><Keywords>Prospective Studies</Keywords><Keywords>radiography</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Severity of Illness Index</Keywords><Keywords>Stents</Keywords><Keywords>Suction</Keywords><Keywords>therapy</Keywords><Keywords>Thorax</Keywords><Reprint>Not in File</Reprint><Start_Page>557</Start_Page><End_Page>567</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>358</Volume><Issue>6</Issue><Address>Thorax Center, Department of Cardiology, Triadegebouw, Gang LM1.004, University Medical Center Groningen, University of Groningen, P.O. Box 30.001, 9700 RB Groningen, the Netherlands. fzijlstra@thorax.umcg.nl</Address><Web_URL>PM:18256391</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[59].
A meta-analysis of thrombectomy devices and distal protection devices consisting of 14 clinical trials of 2630 patients demonstrated that there was no benefit in terms of reduction in death and reinfarction with the anti-embolic devices compared with standard PCI (4% vs. 4.5%, p=0.35). There was also no reduction in death and reinfarction when the thrombectomy and distal protection devices compared with standard PCI were analyzed separately (4.4% vs. 4.2%, p=0.95 and 3.5% vs. 5%, p=0.20 respectively) ADDIN REFMGR.CITE <Refman><Author>Kunadian</Author><Year>2007</Year><RecNum>1137</RecNum><IDText>Meta-Analysis of Randomised Trials Comparing Anti-Embolic Devices with Standard PCI for Improving Myocardial Reperfusion in Patients with Acute Myocardial Infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1137</Ref_ID><Title_Primary><f name="Verdana,Bold">Meta-Analysis of Randomised Trials Comparing Anti-Embolic Devices with Standard PCI for Improving Myocardial Reperfusion in Patients with Acute Myocardial Infarction</f></Title_Primary><Authors_Primary>Kunadian,B</Authors_Primary><Authors_Primary>Vijayalakshmi,K</Authors_Primary><Authors_Primary>Dunning,J</Authors_Primary><Authors_Primary>de Belder,M.A.</Authors_Primary><Date_Primary>2007</Date_Primary><Keywords>Myocardial Reperfusion</Keywords><Reprint>Not in File</Reprint><Periodical>Catheterizarion and Cardiovascular Interventions</Periodical><Volume>Accepted</Volume><ZZ_JournalFull><f name="System">Catheterizarion and Cardiovascular Interventions</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[60].
There are several potential reasons for the failure of the anti-embolic devices to improve clinical outcomes. First, in addition to distal embolization there are a number of other potential factors that result in microvascular dysfunction ADDIN REFMGR.CITE <Refman><Author>Gregorini</Author><Year>1999</Year><RecNum>328</RecNum><IDText>Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>328</Ref_ID><Title_Primary>Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction</Title_Primary><Authors_Primary>Gregorini,L.</Authors_Primary><Authors_Primary>Marco,J.</Authors_Primary><Authors_Primary>Kozakova,M.</Authors_Primary><Authors_Primary>Palombo,C.</Authors_Primary><Authors_Primary>Anguissola,G.B.</Authors_Primary><Authors_Primary>Marco,I.</Authors_Primary><Authors_Primary>Bernies,M.</Authors_Primary><Authors_Primary>Cassagneau,B.</Authors_Primary><Authors_Primary>Distante,A.</Authors_Primary><Authors_Primary>Bossi,I.M.</Authors_Primary><Authors_Primary>Fajadet,J.</Authors_Primary><Authors_Primary>Heusch,G.</Authors_Primary><Date_Primary>1999/2/2</Date_Primary><Keywords>Adrenergic alpha-Antagonists</Keywords><Keywords>Adrenergic beta-Antagonists</Keywords><Keywords>Aged</Keywords><Keywords>Angiography</Keywords><Keywords>Arteries</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Echocardiography</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Perfusion</Keywords><Keywords>Phentolamine</Keywords><Keywords>physiopathology</Keywords><Keywords>Piperazines</Keywords><Keywords>radiography</Keywords><Keywords>Receptors,Adrenergic,alpha</Keywords><Keywords>Stents</Keywords><Keywords>surgery</Keywords><Keywords>therapeutic use</Keywords><Keywords>Vasoconstriction</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>482</Start_Page><End_Page>490</End_Page><Periodical>Circulation</Periodical><Volume>99</Volume><Issue>4</Issue><Address>Clinique Pasteur, Centre de Cardiologie Interventionelle, Toulouse, France. luisa.gregorini@unimi.it</Address><Web_URL>PM:9927393</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Lefroy</Author><Year>1996</Year><RecNum>2526</RecNum><IDText>Regional changes in angiotensin II receptor density after experimental myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2526</Ref_ID><Title_Primary>Regional changes in angiotensin II receptor density after experimental myocardial infarction</Title_Primary><Authors_Primary>Lefroy,D.C.</Authors_Primary><Authors_Primary>Wharton,J.</Authors_Primary><Authors_Primary>Crake,T.</Authors_Primary><Authors_Primary>Knock,G.A.</Authors_Primary><Authors_Primary>Rutherford,R.A.</Authors_Primary><Authors_Primary>Suzuki,T.</Authors_Primary><Authors_Primary>Morgan,K.</Authors_Primary><Authors_Primary>Polak,J.M.</Authors_Primary><Authors_Primary>Poole-Wilson,P.A.</Authors_Primary><Date_Primary>1996/2</Date_Primary><Keywords>Angiotensin II</Keywords><Keywords>Animals</Keywords><Keywords>Arteries</Keywords><Keywords>Autoradiography</Keywords><Keywords>etiology</Keywords><Keywords>Evaluation Studies as Topic</Keywords><Keywords>Heart</Keywords><Keywords>Infarction</Keywords><Keywords>injuries</Keywords><Keywords>Ligation</Keywords><Keywords>London</Keywords><Keywords>Male</Keywords><Keywords>metabolism</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Rats</Keywords><Keywords>Rats,Sprague-Dawley</Keywords><Keywords>Receptors,Angiotensin</Keywords><Keywords>Research</Keywords><Reprint>Not in File</Reprint><Start_Page>429</Start_Page><End_Page>440</End_Page><Periodical>J.Mol.Cell Cardiol</Periodical><Volume>28</Volume><Issue>2</Issue><Address>Department of Histochemistry, Royal Postgraduate Medical School, London, UK</Address><Web_URL>PM:8729073</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Mol.Cell Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Murohara</Author><Year>1994</Year><RecNum>2525</RecNum><IDText>Polymorphonuclear leukocyte-induced vasocontraction and endothelial dysfunction. Role of selectins</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2525</Ref_ID><Title_Primary>Polymorphonuclear leukocyte-induced vasocontraction and endothelial dysfunction. Role of selectins</Title_Primary><Authors_Primary>Murohara,T.</Authors_Primary><Authors_Primary>Buerke,M.</Authors_Primary><Authors_Primary>Lefer,A.M.</Authors_Primary><Date_Primary>1994/9</Date_Primary><Keywords>Acetylcholine</Keywords><Keywords>Animals</Keywords><Keywords>antagonists & inhibitors</Keywords><Keywords>Antibodies</Keywords><Keywords>Antibodies,Monoclonal</Keywords><Keywords>Arteries</Keywords><Keywords>Cats</Keywords><Keywords>Cell Adhesion</Keywords><Keywords>Cell Adhesion Molecules</Keywords><Keywords>Coronary Vessels</Keywords><Keywords>drug effects</Keywords><Keywords>Endothelium</Keywords><Keywords>Endothelium,Vascular</Keywords><Keywords>Glycoproteins</Keywords><Keywords>Hydrogen Peroxide</Keywords><Keywords>immunology</Keywords><Keywords>L-Selectin</Keywords><Keywords>Male</Keywords><Keywords>Muscle,Smooth,Vascular</Keywords><Keywords>Neutrophils</Keywords><Keywords>Oligosaccharides</Keywords><Keywords>P-Selectin</Keywords><Keywords>pharmacology</Keywords><Keywords>physiology</Keywords><Keywords>Platelet Activating Factor</Keywords><Keywords>Platelet Membrane Glycoproteins</Keywords><Keywords>Receptors,Cell Surface</Keywords><Keywords>Receptors,G-Protein-Coupled</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Sodium Nitrite</Keywords><Keywords>Thrombin</Keywords><Keywords>Vasoconstriction</Keywords><Reprint>Not in File</Reprint><Start_Page>1509</Start_Page><End_Page>1519</End_Page><Periodical>Arterioscler.Thromb.</Periodical><Volume>14</Volume><Issue>9</Issue><Address>Department of Physiology, Jefferson Medical College, Thomas Jefferson University, Philadelphia, Pa. 19107-6799</Address><Web_URL>PM:7520747</Web_URL><ZZ_JournalStdAbbrev><f name="System">Arterioscler.Thromb.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Seydoux</Author><Year>1993</Year><RecNum>2527</RecNum><IDText>Platelet and neutrophil imaging techniques in the investigation of the response to thrombolytic therapy and the no-reflow phenomenon</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2527</Ref_ID><Title_Primary>Platelet and neutrophil imaging techniques in the investigation of the response to thrombolytic therapy and the no-reflow phenomenon</Title_Primary><Authors_Primary>Seydoux,C.</Authors_Primary><Authors_Primary>Goy,J.J.</Authors_Primary><Authors_Primary>Davies,G.</Authors_Primary><Date_Primary>1993/4</Date_Primary><Keywords>Acute Disease</Keywords><Keywords>Animals</Keywords><Keywords>Blood Platelets</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Coronary Disease</Keywords><Keywords>Coronary Thrombosis</Keywords><Keywords>diagnosis</Keywords><Keywords>Humans</Keywords><Keywords>methods</Keywords><Keywords>Neutrophils</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Platelet Activation</Keywords><Keywords>Research</Keywords><Keywords>Switzerland</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Reprint>Not in File</Reprint><Start_Page>1142</Start_Page><End_Page>1147</End_Page><Periodical>Am.Heart J.</Periodical><Volume>125</Volume><Issue>4</Issue><Address>Departement de Medecine Interne, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland</Address><Web_URL>PM:8465741</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.Heart J.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[32;61-63]. Thus the removal of thrombus alone might not be sufficient to restore microvascular function. Hence treatment strategies consisting of anti-embolic devices alone without addressing the other factors responsible for microvascular dysfunction does not lead to improved outcomes following an acute myocardial infarction. In addition, the use of devices can result in dislodgement of thrombus proximally into the non-culprit vessels, into the unprotected side branches and distally during the initial stages of trying to cross the lesion using the wire and the device which could lead to further myocardial damage in the previously uninvolved territories.
Delayed PCI
Although significant benefit has been demonstrated with primary PCI compared to fibrinolytic therapy among those who present early after symptom onset, it is important to determine the efficacy of primary PCI for patients who present late (>24 hours). This was examined by Hori et al in a small study of 83 patients presenting >24 hours after symptom onset comparing those who did (n=44) and did not (n=39) undergo PTCA ADDIN REFMGR.CITE <Refman><Author>Horie</Author><Year>1998</Year><RecNum>272</RecNum><IDText>Long-term beneficial effect of late reperfusion for acute anterior myocardial infarction with percutaneous transluminal coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>272</Ref_ID><Title_Primary>Long-term beneficial effect of late reperfusion for acute anterior myocardial infarction with percutaneous transluminal coronary angioplasty</Title_Primary><Authors_Primary>Horie,H.</Authors_Primary><Authors_Primary>Takahashi,M.</Authors_Primary><Authors_Primary>Minai,K.</Authors_Primary><Authors_Primary>Izumi,M.</Authors_Primary><Authors_Primary>Takaoka,A.</Authors_Primary><Authors_Primary>Nozawa,M.</Authors_Primary><Authors_Primary>Yokohama,H.</Authors_Primary><Authors_Primary>Fujita,T.</Authors_Primary><Authors_Primary>Sakamoto,T.</Authors_Primary><Authors_Primary>Kito,O.</Authors_Primary><Authors_Primary>Okamura,H.</Authors_Primary><Authors_Primary>Kinoshita,M.</Authors_Primary><Date_Primary>1998/12/1</Date_Primary><Keywords>Acute Disease</Keywords><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Disease</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart</Keywords><Keywords>Humans</Keywords><Keywords>Japan</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>physiology</Keywords><Keywords>Prognosis</Keywords><Keywords>Proportional Hazards Models</Keywords><Keywords>Recurrence</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>2377</Start_Page><End_Page>2382</End_Page><Periodical>Circulation</Periodical><Volume>98</Volume><Issue>22</Issue><Address>First Department of Internal Medicine, Section of Emergency and Critical Medicine (Medical Coordination Center) Shiga University of Medical Science, Shiga, Japan. hajime@belle.shiga-med.ac.jp</Address><Web_URL>PM:9832481</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[64]. At six months there was no difference in the left ventricular ejection fraction and regional wall motion score between the two groups. However, a five year Kaplan-Meier event free survival analysis (free from death, non-fatal reinfarction and congestive cardiac failure) demonstrated that PTCA was associated with better outcome (p<0.0001).
OAT study
The positive benefit with delayed PCI in the study by Hori et al was not demonstrated in the much larger OAT (Occluded Artery Trial) trial ADDIN REFMGR.CITE <Refman><Author>Hochman</Author><Year>2006</Year><RecNum>961</RecNum><IDText>Coronary intervention for persistent occlusion after myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>961</Ref_ID><Title_Primary>Coronary intervention for persistent occlusion after myocardial infarction</Title_Primary><Authors_Primary>Hochman,J.S.</Authors_Primary><Authors_Primary>Lamas,G.A.</Authors_Primary><Authors_Primary>Buller,C.E.</Authors_Primary><Authors_Primary>Dzavik,V.</Authors_Primary><Authors_Primary>Reynolds,H.R.</Authors_Primary><Authors_Primary>Abramsky,S.J.</Authors_Primary><Authors_Primary>Forman,S.</Authors_Primary><Authors_Primary>Ruzyllo,W.</Authors_Primary><Authors_Primary>Maggioni,A.P.</Authors_Primary><Authors_Primary>White,H.</Authors_Primary><Authors_Primary>Sadowski,Z.</Authors_Primary><Authors_Primary>Carvalho,A.C.</Authors_Primary><Authors_Primary>Rankin,J.M.</Authors_Primary><Authors_Primary>Renkin,J.P.</Authors_Primary><Authors_Primary>Steg,P.G.</Authors_Primary><Authors_Primary>Mascette,A.M.</Authors_Primary><Authors_Primary>Sopko,G.</Authors_Primary><Authors_Primary>Pfisterer,M.E.</Authors_Primary><Authors_Primary>Leor,J.</Authors_Primary><Authors_Primary>Fridrich,V.</Authors_Primary><Authors_Primary>Mark,D.B.</Authors_Primary><Authors_Primary>Knatterud,G.L.</Authors_Primary><Date_Primary>2006/12/7</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Cardiology</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>complications</Keywords><Keywords>Coronary Stenosis</Keywords><Keywords>drug therapy</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart</Keywords><Keywords>Heart Failure,Congestive</Keywords><Keywords>Humans</Keywords><Keywords>Kaplan-Meiers Estimate</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>New York</Keywords><Keywords>Patients</Keywords><Keywords>prevention & control</Keywords><Keywords>Proportional Hazards Models</Keywords><Keywords>Recurrence</Keywords><Keywords>Risk</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Reprint>Not in File</Reprint><Start_Page>2395</Start_Page><End_Page>2407</End_Page><Periodical>N Engl J Med</Periodical><Volume>355</Volume><Issue>23</Issue><Address>Cardiovascular Clinical Research Center, Leon Charney Division of Cardiology, New York University School of Medicine, New York 10016, USA</Address><Web_URL>PM:17105759</Web_URL><ZZ_JournalStdAbbrev><f name="System">N Engl J Med</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[65]. This study consisted of 2166 patients who had occluded arteries on coronary angiography 3-28 days after myocardial infarction (1082 underwent PCI and 1084 had medical therapy). The primary endpoint of death, reinfarction and New York Heart Association heart failure class IV at 4-year follow-up was not different between the PCI group and the medical therapy group [17.2% vs. 15.6% (HR 1.16, 95% confidence interval 0.92-1.45, p=0.2)]. When analysed separately for individual endpoints there was no difference in the occurrence of reinfarction (7% vs. 5.3%, p=0.13), heart failure (4.4% vs. 4.5%) and death (9.1% vs. 9.4%) between the two groups. The differences in the outcomes between the OAT study and the previous studies could be attributed to the aggressive medical therapy (86% of patients received beta-blocker therapy) in the OAT study compared to previous studies.
Specific considerations in primary PCI
Although PPCI is the optimal strategy for patients with acute STEMI it is also overcome by a number of limitations including the logistical difficulties of implementing the service particularly for patients who present to non-PCI centers. Some of these issues have been addressed in randomized clinical trials and are discussed in this section.
Door-to-balloon and door-to-needle times
One of the main challenges faced with primary PCI is the timely implementation of treatment to patients with ST elevation myocardial infarction. In an analysis of over 27,000 patients from the NRMI database (National Registry of Myocardial Infarction) of patients with STEMI who presented from June 1994 to March 1998 to 661 community and tertiary hospitals in the United States, Cannon et al demonstrated that the adjusted odds of mortality increased by 41-62% for door-to-balloon in excess of 2 hours. In this analysis the median door-to-balloon time was 1 hour 56 minutes. Around 8% of patients achieved a door-to-balloon time less than 60 minutes. The unadjusted mortality rose from 4.2%-8.5% with increasing door-to-balloon time (p<0.001) ADDIN REFMGR.CITE <Refman><Author>Cannon</Author><Year>2000</Year><RecNum>24</RecNum><IDText>Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>24</Ref_ID><Title_Primary>Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction</Title_Primary><Authors_Primary>Cannon,C.P.</Authors_Primary><Authors_Primary>Gibson,C.M.</Authors_Primary><Authors_Primary>Lambrew,C.T.</Authors_Primary><Authors_Primary>Shoultz,D.A.</Authors_Primary><Authors_Primary>Levy,D.</Authors_Primary><Authors_Primary>French,W.J.</Authors_Primary><Authors_Primary>Gore,J.M.</Authors_Primary><Authors_Primary>Weaver,W.D.</Authors_Primary><Authors_Primary>Rogers,W.J.</Authors_Primary><Authors_Primary>Tiefenbrunn,A.J.</Authors_Primary><Date_Primary>2000/6/14</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Emergency Medical Services</Keywords><Keywords>Female</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Humans</Keywords><Keywords>Logistic Models</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Outcome Assessment (Health Care)</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Registries</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>United States</Keywords><Reprint>Not in File</Reprint><Start_Page>2941</Start_Page><End_Page>2947</End_Page><Periodical>JAMA</Periodical><Volume>283</Volume><Issue>22</Issue><Address>Cardiovascular Division, Brigham and Women's Hospital, 75 Francis St, Boston, MA 02115, USA. ccannon@rics.bwh.harvard.edu</Address><Web_URL>PM:10865271</Web_URL><ZZ_JournalStdAbbrev><f name="System">JAMA</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[66]. In another analysis of the NRMI study, Pinto and coworkers studied the hospital PCI related delays [Door to balloon time (DB)-door to needle time (DN)] among 192,509 patients with STEMI treated with primary PCI (65,600) and fibrinolysis (n=126,909). This analysis demonstrated that 65% of patients presented within 2 hours of symptom onset. They demonstrated that as DB-DN increased, mortality increased also (p<0.001). For every 30 minute increase in the DB-DN there was approximately 10% increase in the relative risk of in-hospital death (p<0.001) ADDIN REFMGR.CITE <Refman><Author>Pinto</Author><Year>2006</Year><RecNum>522</RecNum><IDText>Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>522</Ref_ID><Title_Primary>Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy</Title_Primary><Authors_Primary>Pinto,D.S.</Authors_Primary><Authors_Primary>Kirtane,A.J.</Authors_Primary><Authors_Primary>Nallamothu,B.K.</Authors_Primary><Authors_Primary>Murphy,S.A.</Authors_Primary><Authors_Primary>Cohen,D.J.</Authors_Primary><Authors_Primary>Laham,R.J.</Authors_Primary><Authors_Primary>Cutlip,D.E.</Authors_Primary><Authors_Primary>Bates,E.R.</Authors_Primary><Authors_Primary>Frederick,P.D.</Authors_Primary><Authors_Primary>Miller,D.P.</Authors_Primary><Authors_Primary>Carrozza,J.P.,Jr.</Authors_Primary><Authors_Primary>Antman,E.M.</Authors_Primary><Authors_Primary>Cannon,C.P.</Authors_Primary><Authors_Primary>Gibson,C.M.</Authors_Primary><Date_Primary>2006/11/7</Date_Primary><Keywords>Aged</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolysis</Keywords><Keywords>Heart</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Hospitalization</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Israel</Keywords><Keywords>Male</Keywords><Keywords>Medical Staff,Hospital</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Registries</Keywords><Keywords>Reperfusion</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Time Factors</Keywords><Reprint>Not in File</Reprint><Start_Page>2019</Start_Page><End_Page>2025</End_Page><Periodical>Circulation</Periodical><Volume>114</Volume><Issue>19</Issue><Address>TIMI Study Group and the Cardiovascular Division, Department of Medicine, Beth Israel Deaconess Medical Center, 185 Pilgrim Rd, Boston, MA 02115, USA</Address><Web_URL>PM:17075010</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[67]. Another study from the NRMI study demonstrated that only a small proportion of patients (15%) received PPCI with door-to-balloon times <120 minutes, of which only 4% had door-to-balloon time <90 minutes ADDIN REFMGR.CITE <Refman><Author>Shavelle</Author><Year>2005</Year><RecNum>1233</RecNum><IDText>Outcome in patients transferred for percutaneous coronary intervention (a national registry of myocardial infarction 2/3/4 analysis)</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1233</Ref_ID><Title_Primary>Outcome in patients transferred for percutaneous coronary intervention (a national registry of myocardial infarction 2/3/4 analysis)</Title_Primary><Authors_Primary>Shavelle,D.M.</Authors_Primary><Authors_Primary>Rasouli,M.L.</Authors_Primary><Authors_Primary>Frederick,P.</Authors_Primary><Authors_Primary>Gibson,C.M.</Authors_Primary><Authors_Primary>French,W.J.</Authors_Primary><Date_Primary>2005/11/1</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Comparative Study</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Ischemia</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Patient Transfer</Keywords><Keywords>physiopathology</Keywords><Keywords>Prognosis</Keywords><Keywords>Registries</Keywords><Keywords>Research</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>Risk Factors</Keywords><Keywords>Shock</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Time Factors</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>trends</Keywords><Keywords>United States</Keywords><Reprint>Not in File</Reprint><Start_Page>1227</Start_Page><End_Page>1232</End_Page><Periodical>Am.J.Cardiol.</Periodical><Volume>96</Volume><Issue>9</Issue><Address>The Division of Cardiology, Harbor-UCLA Medical Center, Torrance, California, USA. dshavelle@hotmail.com</Address><Web_URL>PM:16253587</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.J.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[68].
Institutional volume
The data from the NRMI also determined the impact of institutional volume on mortality outcomes following PCI for acute myocardial infarction. A total of 450 hospitals in the United States were divided into quartiles according to the volume of primary angioplasty. The in-hospital mortality was reduced by 28% when PCI was performed in high volume centres compared to the low volume centres (p<0.001) ADDIN REFMGR.CITE <Refman><Author>Canto</Author><Year>2000</Year><RecNum>1780</RecNum><IDText>The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1780</Ref_ID><Title_Primary>The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators</Title_Primary><Authors_Primary>Canto,J.G.</Authors_Primary><Authors_Primary>Every,N.R.</Authors_Primary><Authors_Primary>Magid,D.J.</Authors_Primary><Authors_Primary>Rogers,W.J.</Authors_Primary><Authors_Primary>Malmgren,J.A.</Authors_Primary><Authors_Primary>Frederick,P.D.</Authors_Primary><Authors_Primary>French,W.J.</Authors_Primary><Authors_Primary>Tiefenbrunn,A.J.</Authors_Primary><Authors_Primary>Misra,V.K.</Authors_Primary><Authors_Primary>Kiefe,C.I.</Authors_Primary><Authors_Primary>Barron,H.V.</Authors_Primary><Date_Primary>2000/5/25</Date_Primary><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>drug therapy</Keywords><Keywords>education</Keywords><Keywords>epidemiology</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Logistic Models</Keywords><Keywords>methods</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Registries</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>statistics & numerical data</Keywords><Keywords>surgery</Keywords><Keywords>Survival</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>United States</Keywords><Keywords>utilization</Keywords><Reprint>Not in File</Reprint><Start_Page>1573</Start_Page><End_Page>1580</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>342</Volume><Issue>21</Issue><Address>Department of Medicine, and Center for Outcomes and Effectiveness Research and Education, University of Alabama at Birmingham, 35294-0012, USA</Address><Web_URL>PM:10824077</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[69]. The crude mortality rate was 7.7% among patients who underwent PPCI in high volume centers compared to 5.7% among those who underwent PCI in high volume centers (p<0.001).
Magid et al compared primary PTCA and fibrinolytic therapy in relation to the volume of primary angioplasties carried out in different hospitals among 62, 299 STEMI patients who underwent either therapy from 1994 to 1999 ADDIN REFMGR.CITE <Refman><Author>Magid</Author><Year>2000</Year><RecNum>2528</RecNum><IDText>Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2528</Ref_ID><Title_Primary>Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy</Title_Primary><Authors_Primary>Magid,D.J.</Authors_Primary><Authors_Primary>Calonge,B.N.</Authors_Primary><Authors_Primary>Rumsfeld,J.S.</Authors_Primary><Authors_Primary>Canto,J.G.</Authors_Primary><Authors_Primary>Frederick,P.D.</Authors_Primary><Authors_Primary>Every,N.R.</Authors_Primary><Authors_Primary>Barron,H.V.</Authors_Primary><Date_Primary>2000/12/27</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology Service,Hospital</Keywords><Keywords>Comparative Study</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>history</Keywords><Keywords>Hospital Mortality</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Outcome and Process Assessment (Health Care)</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>standards</Keywords><Keywords>Surgery Department,Hospital</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>United States</Keywords><Keywords>utilization</Keywords><Reprint>Not in File</Reprint><Start_Page>3131</Start_Page><End_Page>3138</End_Page><Periodical>JAMA</Periodical><Volume>284</Volume><Issue>24</Issue><Address>Colorado Permanente Clinical Research Unit, 10350 E Dakota Ave, Denver, CO 80231, USA. David.J.Magid@kp.org</Address><Web_URL>PM:11135776</Web_URL><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[70]. This study classified hospitals into 3 groups based on the number of primary angioplasties performed annually: low-volume group ≤16 procedures per year; intermediate-volume group 17-48 procedures per year and high-volume center ≥49 procedures per year. This study demonstrated that primary PTCA was associated with a significant reduction in mortality over fibrinolysis when primary PCI was performed in a high (3.5% vs. 5.4%, p<0.001) and intermediate (4.5% vs. 5.9%, p<0.001) volume center compared to a low volume center (6.2% vs. 5.9%, p=0.58). Thus in this analysis, primary PTCA in the low volume center did not offer mortality benefit over fibrinolytic therapy.
PPCI without surgical back up
The Atlantic C-PORT trial (Cardiovascular Patients Outcomes Research Team) investigated the feasibility of performing primary PCI in centers without surgical back up ADDIN REFMGR.CITE <Refman><Author>Aversano</Author><Year>2002</Year><RecNum>2581</RecNum><IDText>Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site cardiac surgery: a randomized controlled trial</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2581</Ref_ID><Title_Primary>Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site cardiac surgery: a randomized controlled trial</Title_Primary><Authors_Primary>Aversano,T.</Authors_Primary><Authors_Primary>Aversano,L.T.</Authors_Primary><Authors_Primary>Passamani,E.</Authors_Primary><Authors_Primary>Knatterud,G.L.</Authors_Primary><Authors_Primary>Terrin,M.L.</Authors_Primary><Authors_Primary>Williams,D.O.</Authors_Primary><Authors_Primary>Forman,S.A.</Authors_Primary><Date_Primary>2002/4/17</Date_Primary><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Comparative Study</Keywords><Keywords>Death</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Hospitals</Keywords><Keywords>Hospitals,Community</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Length of Stay</Keywords><Keywords>Male</Keywords><Keywords>Massachusetts</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Physicians</Keywords><Keywords>Plasminogen</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Recurrence</Keywords><Keywords>Research</Keywords><Keywords>Stroke</Keywords><Keywords>surgery</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Keywords>Treatment Outcome</Keywords><Reprint>Not in File</Reprint><Start_Page>1943</Start_Page><End_Page>1951</End_Page><Periodical>JAMA</Periodical><Volume>287</Volume><Issue>15</Issue><Address>Blalock 524, Johns Hopkins Hospital, 600 N Wolfe St, Baltimore, MD 21210, USA. taversan@jhmi.edu</Address><Web_URL>PM:11960536</Web_URL><ZZ_JournalFull><f name="System">JAMA</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[71]. A total 225 patients were randomized to undergo primary PCI and the remaining 226 patients were randomized to fibrinolytic therapy in 11 hospitals without cardiac surgery availability. The primary endpoint of death, recurrent myocardial infarction, stroke and median hospital length of stay was significantly reduced among those who underwent PPCI compared to those who received fibrinolysis (10.7% vs. 17.7%, p=0.03) at 6 weeks. This benefit extended to 6 months in favor of PPCI (12.4% vs. 19.9%, p=0.03). When analyzed for individual outcomes at 6 months, there was no benefit in terms of reduction in mortality (6.2% vs. 7.1%, p=0.72) and stroke (2.2% vs. 4%, p=0.28) with the PPCI strategy compared to fibrinolysis. However there was significant reduction in recurrent MI (5.3% vs. 10.6%, p=0.04) and median length of hospital stay (4.5 days vs. 6 days, p=0.02). Although this study is criticized for its early termination due to funding issues, it demonstrates that PPCI is feasible in centers without cardiac surgical back up.
Inter-hospital transfer
DANAMI study
The feasibility and safety of transport of patients from peripheral hospitals to centers where PPCI is performed was evaluated in the DANAMI-2 study (Danish Multicenter Randomized study on fibrinolytic therapy versus Acute Coronary Angioplasty in Acute Myocardial Infarction) ADDIN REFMGR.CITE <Refman><Author>Andersen</Author><Year>2003</Year><RecNum>1781</RecNum><IDText>A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1781</Ref_ID><Title_Primary>A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction</Title_Primary><Authors_Primary>Andersen,H.R.</Authors_Primary><Authors_Primary>Nielsen,T.T.</Authors_Primary><Authors_Primary>Rasmussen,K.</Authors_Primary><Authors_Primary>Thuesen,L.</Authors_Primary><Authors_Primary>Kelbaek,H.</Authors_Primary><Authors_Primary>Thayssen,P.</Authors_Primary><Authors_Primary>Abildgaard,U.</Authors_Primary><Authors_Primary>Pedersen,F.</Authors_Primary><Authors_Primary>Madsen,J.K.</Authors_Primary><Authors_Primary>Grande,P.</Authors_Primary><Authors_Primary>Villadsen,A.B.</Authors_Primary><Authors_Primary>Krusell,L.R.</Authors_Primary><Authors_Primary>Haghfelt,T.</Authors_Primary><Authors_Primary>Lomholt,P.</Authors_Primary><Authors_Primary>Husted,S.E.</Authors_Primary><Authors_Primary>Vigholt,E.</Authors_Primary><Authors_Primary>Kjaergard,H.K.</Authors_Primary><Authors_Primary>Mortensen,L.S.</Authors_Primary><Date_Primary>2003/8/21</Date_Primary><Keywords>Adult</Keywords><Keywords>adverse effects</Keywords><Keywords>Aged</Keywords><Keywords>Aged,80 and over</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Comparative Study</Keywords><Keywords>Denmark</Keywords><Keywords>drug therapy</Keywords><Keywords>epidemiology</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolysis</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Hospitals</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Patient Transfer</Keywords><Keywords>Plasminogen</Keywords><Keywords>Recurrence</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Stroke</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Time Factors</Keywords><Keywords>Tissue Plasminogen Activator</Keywords><Reprint>Not in File</Reprint><Start_Page>733</Start_Page><End_Page>742</End_Page><Periodical>N.Engl.J.Med.</Periodical><Volume>349</Volume><Issue>8</Issue><Address>Department of Cardiology at Skejby Hospital, Aarhus University Hospital, Aarhus, Denmark. henning.rud.andersen@iekf.au.dk</Address><Web_URL>PM:12930925</Web_URL><ZZ_JournalStdAbbrev><f name="System">N.Engl.J.Med.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[72] which enrolled 1572 patients between December 1997 to October 2001. A total of 1129 patients presented to 24 referral hospitals and 443 were admitted to 5 invasive treatment centers. All patients were randomized to undergo either primary PCI or fibrinolysis using IV alteplase. The primary endpoint of this trial consisted of death, clinical evidence of reinfarction or disabling stroke at 30 days. Of those who were transferred from the referral centers, the primary endpoint occurred in 8.5% of cases in the PPCI group and 14.2% in the fibrinolysis group (p=0.002). Similarly, among patients who were admitted directly to the invasive centers, the primary endpoint occurred in 6.7% of patients who underwent PPCI and 12.3% of patients who had fibrinolysis (p=0.05). Among all patients, the incidence of reinfarction was 1.6% in those who had PPCI and 6.3% among those who had fibrinolysis (p<0.001) with no difference in the incidence of death and stroke. In this study, 96% of patients were transferred to a median distance of 50 km (range 3-150 km). The median transfer time was 67 minutes (interquartile range 50-85 minutes). Of these 43% of patients were transferred within <60 minutes.
PRAGUE study
The PRAGUE trial (PRimary Angioplasty in patients transferred from General community hospitals to specialized PTCA Units with or without Emergency fibrinolysis) is another trial that tested the safety and feasibility of transport of patients with STEMI to a PCI center ADDIN REFMGR.CITE <Refman><Author>Widimsky</Author><Year>2000</Year><RecNum>1762</RecNum><IDText>Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE study</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1762</Ref_ID><Title_Primary>Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE study</Title_Primary><Authors_Primary>Widimsky,P.</Authors_Primary><Authors_Primary>Groch,L.</Authors_Primary><Authors_Primary>Zelizko,M.</Authors_Primary><Authors_Primary>Aschermann,M.</Authors_Primary><Authors_Primary>Bednar,F.</Authors_Primary><Authors_Primary>Suryapranata,H.</Authors_Primary><Date_Primary>2000/5</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Catheterization</Keywords><Keywords>Comparative Study</Keywords><Keywords>complications</Keywords><Keywords>Czech Republic</Keywords><Keywords>Emergencies</Keywords><Keywords>Feasibility Studies</Keywords><Keywords>Female</Keywords><Keywords>Hospitals</Keywords><Keywords>Hospitals,Community</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Laboratories</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multicenter Studies</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Patient Transfer</Keywords><Keywords>Reperfusion</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Fibrillation</Keywords><Reprint>Not in File</Reprint><Start_Page>823</Start_Page><End_Page>831</End_Page><Periodical>Eur.Heart J.</Periodical><Volume>21</Volume><Issue>10</Issue><Address>Cardiocenter, University Hospital, Vinohrady, Prague, Czech Republic</Address><Web_URL>PM:10781354</Web_URL><ZZ_JournalStdAbbrev><f name="System">Eur.Heart J.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[73]. This study consisted of 300 STEMI patients who presented to General Community hospitals within 6 hours of symptom onset and were randomized to receive fibrinolysis alone (n=99), receive fibrinolysis and transport for primary angioplasty (n=100) or undergo primary angioplasty without fibrinolysis (n=101). In the PRAGUE study, primary angioplasty was superior in terms of reductions in death, reinfarction and stroke compared to the fibrinolysis group and fibrinolysis and transport group (8% vs. 23% vs. 15%, p<0.02 respectively). The incidence of reinfarction was reduced using the transport strategy compared to fibrinolysis alone (1% PPCI vs. 7% fibrinolysis and transport vs. 10% in fibrinolysis group, p<0.03). Hence this study demonstrated the feasibility of transport of STEMI patients and that primary PCI was a superior strategy.
Assessment of reperfusion following primary PCI
Electrocardiographic changes
A number of techniques have been adopted to assess reperfusion following percutaneous coronary intervention for acute myocardial infarction. The extent of ST segment resolution on the electrocardiogram is a commonly used method to assess reperfusion. Several studies have determined the relationship between the extent of ST segment resolution and their impact on left ventricular function improvement and clinical outcomes ADDIN REFMGR.CITE <Refman><Author>Santoro</Author><Year>1997</Year><RecNum>2535</RecNum><IDText>Rapid reduction of ST-segment elevation after successful direct angioplasty in acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2535</Ref_ID><Title_Primary>Rapid reduction of ST-segment elevation after successful direct angioplasty in acute myocardial infarction</Title_Primary><Authors_Primary>Santoro,G.M.</Authors_Primary><Authors_Primary>Antoniucci,D.</Authors_Primary><Authors_Primary>Valenti,R.</Authors_Primary><Authors_Primary>Bolognese,L.</Authors_Primary><Authors_Primary>Buonamici,P.</Authors_Primary><Authors_Primary>Trapani,M.</Authors_Primary><Authors_Primary>Boddi,V.</Authors_Primary><Authors_Primary>Fazzini,P.F.</Authors_Primary><Date_Primary>1997/9/15</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Aged,80 and over</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Creatine Kinase</Keywords><Keywords>diagnosis</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>pathology</Keywords><Keywords>physiopathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Reperfusion</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>685</Start_Page><End_Page>689</End_Page><Periodical>Am.J.Cardiol</Periodical><Volume>80</Volume><Issue>6</Issue><Address>Division of Cardiology, Careggi Hospital, Viale Morgagni, and the Institute of General Pathology, University of Florence, Italy</Address><Web_URL>PM:9315569</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.J.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Santoro</Author><Year>1998</Year><RecNum>2534</RecNum><IDText>Relation between ST-segment changes and myocardial perfusion evaluated by myocardial contrast echocardiography in patients with acute myocardial infarction treated with direct angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2534</Ref_ID><Title_Primary>Relation between ST-segment changes and myocardial perfusion evaluated by myocardial contrast echocardiography in patients with acute myocardial infarction treated with direct angioplasty</Title_Primary><Authors_Primary>Santoro,G.M.</Authors_Primary><Authors_Primary>Valenti,R.</Authors_Primary><Authors_Primary>Buonamici,P.</Authors_Primary><Authors_Primary>Bolognese,L.</Authors_Primary><Authors_Primary>Cerisano,G.</Authors_Primary><Authors_Primary>Moschi,G.</Authors_Primary><Authors_Primary>Trapani,M.</Authors_Primary><Authors_Primary>Antoniucci,D.</Authors_Primary><Authors_Primary>Fazzini,P.F.</Authors_Primary><Date_Primary>1998/10/15</Date_Primary><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Prognosis</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Reperfusion</Keywords><Keywords>Risk</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>therapy</Keywords><Keywords>ultrasonography</Keywords><Reprint>Not in File</Reprint><Start_Page>932</Start_Page><End_Page>937</End_Page><Periodical>Am.J.Cardiol</Periodical><Volume>82</Volume><Issue>8</Issue><Address>Division of Cardiology, Careggi Hospital, Florence, Italy</Address><Web_URL>PM:9794347</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.J.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Matetzky</Author><Year>1999</Year><RecNum>2532</RecNum><IDText>The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2532</Ref_ID><Title_Primary>The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA</Title_Primary><Authors_Primary>Matetzky,S.</Authors_Primary><Authors_Primary>Novikov,M.</Authors_Primary><Authors_Primary>Gruberg,L.</Authors_Primary><Authors_Primary>Freimark,D.</Authors_Primary><Authors_Primary>Feinberg,M.</Authors_Primary><Authors_Primary>Elian,D.</Authors_Primary><Authors_Primary>Novikov,I.</Authors_Primary><Authors_Primary>Di,Segni E.</Authors_Primary><Authors_Primary>Agranat,O.</Authors_Primary><Authors_Primary>Har-Zahav,Y.</Authors_Primary><Authors_Primary>Rabinowitz,B.</Authors_Primary><Authors_Primary>Kaplinsky,E.</Authors_Primary><Authors_Primary>Hod,H.</Authors_Primary><Date_Primary>1999/12</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>diagnosis</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Heart Failure</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Israel</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Myocardium</Keywords><Keywords>Odds Ratio</Keywords><Keywords>physiopathology</Keywords><Keywords>Prevalence</Keywords><Keywords>Regression Analysis</Keywords><Keywords>Reperfusion</Keywords><Keywords>Survival Rate</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1932</Start_Page><End_Page>1938</End_Page><Periodical>J.Am.Coll.Cardiol</Periodical><Volume>34</Volume><Issue>7</Issue><Address>Heart Institute, Chaim Sheba Medical Center, Tel Hashomer, Tel Aviv, Israel</Address><Web_URL>PM:10588206</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Claeys</Author><Year>1999</Year><RecNum>2536</RecNum><IDText>Determinants and prognostic implications of persistent ST-segment elevation after primary angioplasty for acute myocardial infarction: importance of microvascular reperfusion injury on clinical outcome</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2536</Ref_ID><Title_Primary>Determinants and prognostic implications of persistent ST-segment elevation after primary angioplasty for acute myocardial infarction: importance of microvascular reperfusion injury on clinical outcome</Title_Primary><Authors_Primary>Claeys,M.J.</Authors_Primary><Authors_Primary>Bosmans,J.</Authors_Primary><Authors_Primary>Veenstra,L.</Authors_Primary><Authors_Primary>Jorens,P.</Authors_Primary><Authors_Primary>De,RaedtH</Authors_Primary><Authors_Primary>Vrints,C.J.</Authors_Primary><Date_Primary>1999/4/20</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arrhythmias,Cardiac</Keywords><Keywords>Arteries</Keywords><Keywords>Biological Markers</Keywords><Keywords>blood</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Creatine Kinase</Keywords><Keywords>Death</Keywords><Keywords>Electrocardiography</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart Failure</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>injuries</Keywords><Keywords>Isoenzymes</Keywords><Keywords>Life Tables</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Microcirculation</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion Injury</Keywords><Keywords>Pressure</Keywords><Keywords>Prognosis</Keywords><Keywords>Proportional Hazards Models</Keywords><Keywords>Reperfusion</Keywords><Keywords>Reperfusion Injury</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Dysfunction,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1972</Start_Page><End_Page>1977</End_Page><Periodical>Circulation</Periodical><Volume>99</Volume><Issue>15</Issue><Address>Department of Cardiology, Antwerp University Hospital, Edegem, Belgium.mclaeys@uia.ua.ac.be</Address><Web_URL>PM:10209000</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[74-77]. Santoro et al demonstrated that patients with >50% ST segment resolution post PCI had significantly better wall motion score index (p<0.001), LVEF (p<0.001), and functional recovery (>0.22 decrease in infarct zone wall motion score index) [34% vs. 78%, p<0.001] at one month compared to those who had <50% ST segment resolution ADDIN REFMGR.CITE <Refman><Author>Santoro</Author><Year>1997</Year><RecNum>2535</RecNum><IDText>Rapid reduction of ST-segment elevation after successful direct angioplasty in acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2535</Ref_ID><Title_Primary>Rapid reduction of ST-segment elevation after successful direct angioplasty in acute myocardial infarction</Title_Primary><Authors_Primary>Santoro,G.M.</Authors_Primary><Authors_Primary>Antoniucci,D.</Authors_Primary><Authors_Primary>Valenti,R.</Authors_Primary><Authors_Primary>Bolognese,L.</Authors_Primary><Authors_Primary>Buonamici,P.</Authors_Primary><Authors_Primary>Trapani,M.</Authors_Primary><Authors_Primary>Boddi,V.</Authors_Primary><Authors_Primary>Fazzini,P.F.</Authors_Primary><Date_Primary>1997/9/15</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Aged,80 and over</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Creatine Kinase</Keywords><Keywords>diagnosis</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>pathology</Keywords><Keywords>physiopathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Reperfusion</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>685</Start_Page><End_Page>689</End_Page><Periodical>Am.J.Cardiol</Periodical><Volume>80</Volume><Issue>6</Issue><Address>Division of Cardiology, Careggi Hospital, Viale Morgagni, and the Institute of General Pathology, University of Florence, Italy</Address><Web_URL>PM:9315569</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.J.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[74]. In addition to better LV function recovery, Matetzky et al demonstrated that patients with ST segment resolution >50% had significant improvement in congestive cardiac failure (19% vs. 28%, p=0.04) and long term (>2 years) mortality (OR 7.3, 95% confidence interval 1.9-28, p=0.004) compared to those who did not have significant ST segment resolution post PTCA ADDIN REFMGR.CITE <Refman><Author>Matetzky</Author><Year>1999</Year><RecNum>2532</RecNum><IDText>The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2532</Ref_ID><Title_Primary>The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA</Title_Primary><Authors_Primary>Matetzky,S.</Authors_Primary><Authors_Primary>Novikov,M.</Authors_Primary><Authors_Primary>Gruberg,L.</Authors_Primary><Authors_Primary>Freimark,D.</Authors_Primary><Authors_Primary>Feinberg,M.</Authors_Primary><Authors_Primary>Elian,D.</Authors_Primary><Authors_Primary>Novikov,I.</Authors_Primary><Authors_Primary>Di,Segni E.</Authors_Primary><Authors_Primary>Agranat,O.</Authors_Primary><Authors_Primary>Har-Zahav,Y.</Authors_Primary><Authors_Primary>Rabinowitz,B.</Authors_Primary><Authors_Primary>Kaplinsky,E.</Authors_Primary><Authors_Primary>Hod,H.</Authors_Primary><Date_Primary>1999/12</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>diagnosis</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Heart</Keywords><Keywords>Heart Failure</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>Israel</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Myocardium</Keywords><Keywords>Odds Ratio</Keywords><Keywords>physiopathology</Keywords><Keywords>Prevalence</Keywords><Keywords>Regression Analysis</Keywords><Keywords>Reperfusion</Keywords><Keywords>Survival Rate</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1932</Start_Page><End_Page>1938</End_Page><Periodical>J.Am.Coll.Cardiol</Periodical><Volume>34</Volume><Issue>7</Issue><Address>Heart Institute, Chaim Sheba Medical Center, Tel Hashomer, Tel Aviv, Israel</Address><Web_URL>PM:10588206</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[76]. Likewise, Claeys et al demonstrated decreased cardiac death rate among those who had ≥50% ST segment resolution after successful PTCA compared to those who had <50% resolution ADDIN REFMGR.CITE <Refman><Author>Claeys</Author><Year>1999</Year><RecNum>2536</RecNum><IDText>Determinants and prognostic implications of persistent ST-segment elevation after primary angioplasty for acute myocardial infarction: importance of microvascular reperfusion injury on clinical outcome</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2536</Ref_ID><Title_Primary>Determinants and prognostic implications of persistent ST-segment elevation after primary angioplasty for acute myocardial infarction: importance of microvascular reperfusion injury on clinical outcome</Title_Primary><Authors_Primary>Claeys,M.J.</Authors_Primary><Authors_Primary>Bosmans,J.</Authors_Primary><Authors_Primary>Veenstra,L.</Authors_Primary><Authors_Primary>Jorens,P.</Authors_Primary><Authors_Primary>De,RaedtH</Authors_Primary><Authors_Primary>Vrints,C.J.</Authors_Primary><Date_Primary>1999/4/20</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arrhythmias,Cardiac</Keywords><Keywords>Arteries</Keywords><Keywords>Biological Markers</Keywords><Keywords>blood</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Creatine Kinase</Keywords><Keywords>Death</Keywords><Keywords>Electrocardiography</Keywords><Keywords>epidemiology</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart Failure</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>injuries</Keywords><Keywords>Isoenzymes</Keywords><Keywords>Life Tables</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Microcirculation</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion Injury</Keywords><Keywords>Pressure</Keywords><Keywords>Prognosis</Keywords><Keywords>Proportional Hazards Models</Keywords><Keywords>Reperfusion</Keywords><Keywords>Reperfusion Injury</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>Ventricular Dysfunction,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1972</Start_Page><End_Page>1977</End_Page><Periodical>Circulation</Periodical><Volume>99</Volume><Issue>15</Issue><Address>Department of Cardiology, Antwerp University Hospital, Edegem, Belgium.mclaeys@uia.ua.ac.be</Address><Web_URL>PM:10209000</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[77].
Coronary flow velocity assessment
Coronary flow velocity assessments using coronary Doppler FloWire (Cardiometrics, Inc) can be used to determine myocardial functional recovery at a later stage. Kawamoto et al studied 23 patients with acute anterior myocardial infarction undergoing primary PTCA. Wall motion score index were measured by echocardiography before PTCA and one month following the procedure. During PTCA coronary flow velocities [average systolic peak velocity (ASPV) and deceleration time of diastolic flow velocity (DDT)] were measured. The one month wall motion score index was correlated with ASPV (r=-0.54, p=0.007) and DDT (r=-0.62, p0.002). The cut-off values to predict viable myocardium was 6.5 cm/s for ASPV (sensitivity 79%, specificity 89%) and 600ms for DDT (sensitivity 86%, specificity 89%) ADDIN REFMGR.CITE <Refman><Author>Kawamoto</Author><Year>1999</Year><RecNum>1861</RecNum><IDText>Can coronary blood flow velocity pattern after primary percutaneous transluminal coronary angioplasty [correction of angiography] predict recovery of regional left ventricular function in patients with acute myocardial infarction?</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1861</Ref_ID><Title_Primary>Can coronary blood flow velocity pattern after primary percutaneous transluminal coronary angioplasty [correction of angiography] predict recovery of regional left ventricular function in patients with acute myocardial infarction?</Title_Primary><Authors_Primary>Kawamoto,T.</Authors_Primary><Authors_Primary>Yoshida,K.</Authors_Primary><Authors_Primary>Akasaka,T.</Authors_Primary><Authors_Primary>Hozumi,T.</Authors_Primary><Authors_Primary>Takagi,T.</Authors_Primary><Authors_Primary>Kaji,S.</Authors_Primary><Authors_Primary>Ueda,Y.</Authors_Primary><Date_Primary>1999/7/27</Date_Primary><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>blood</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>diagnosis</Keywords><Keywords>Echocardiography</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>injuries</Keywords><Keywords>Japan</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Prognosis</Keywords><Keywords>Risk</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>339</Start_Page><End_Page>345</End_Page><Periodical>Circulation</Periodical><Volume>100</Volume><Issue>4</Issue><Address>Department of Cardiology, Kobe General Hospital, Kobe, Japan</Address><Web_URL>PM:10421592</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[78]. Thus, the Doppler FloWire during PTCA can be used to predict myocardial viability at a later stage. In addition to predicting myocardial viability, coronary flow reserve ≤1.3 measured using the Doppler FloWire during primary PTCA was associated with long term adverse events (cardiac death, reinfarction and congestive cardiac failure) ADDIN REFMGR.CITE <Refman><Author>Takahashi</Author><Year>2007</Year><RecNum>2538</RecNum><IDText>Usefulness of coronary flow reserve immediately after primary coronary angioplasty for acute myocardial infarction in predicting long-term adverse cardiac events</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2538</Ref_ID><Title_Primary>Usefulness of coronary flow reserve immediately after primary coronary angioplasty for acute myocardial infarction in predicting long-term adverse cardiac events</Title_Primary><Authors_Primary>Takahashi,T.</Authors_Primary><Authors_Primary>Hiasa,Y.</Authors_Primary><Authors_Primary>Ohara,Y.</Authors_Primary><Authors_Primary>Miyazaki,S.</Authors_Primary><Authors_Primary>Ogura,R.</Authors_Primary><Authors_Primary>Miyajima,H.</Authors_Primary><Authors_Primary>Yuba,K.</Authors_Primary><Authors_Primary>Suzuki,N.</Authors_Primary><Authors_Primary>Hosokawa,S.</Authors_Primary><Authors_Primary>Kishi,K.</Authors_Primary><Authors_Primary>Ohtani,R.</Authors_Primary><Date_Primary>2007/9/1</Date_Primary><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>blood</Keywords><Keywords>Blood Flow Velocity</Keywords><Keywords>Cardiac Volume</Keywords><Keywords>Cardiology</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>Creatine Kinase</Keywords><Keywords>Death</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Forecasting</Keywords><Keywords>Heart</Keywords><Keywords>Heart Arrest</Keywords><Keywords>Heart Failure</Keywords><Keywords>Humans</Keywords><Keywords>Incidence</Keywords><Keywords>Infarction</Keywords><Keywords>injuries</Keywords><Keywords>Japan</Keywords><Keywords>Longitudinal Studies</Keywords><Keywords>Male</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>physiology</Keywords><Keywords>Recovery of Function</Keywords><Keywords>Recurrence</Keywords><Keywords>Reperfusion</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>Stroke Volume</Keywords><Keywords>Survival</Keywords><Keywords>Survival Analysis</Keywords><Keywords>therapy</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>806</Start_Page><End_Page>811</End_Page><Periodical>Am.J.Cardiol</Periodical><Volume>100</Volume><Issue>5</Issue><Address>Department of Cardiology, Tokushima Red Cross Hospital, Komatsushima, Japan. ttak@tokushima-med.jrc.or.jp</Address><Web_URL>PM:17719324</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.J.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[79].
Myocardial Imaging
Myocardial imaging techniques such as dobutamine stress echocardiography, myocardial contrast echocardiography ADDIN REFMGR.CITE <Refman><Author>Balcells</Author><Year>2003</Year><RecNum>239</RecNum><IDText>Detection of myocardial viability by contrast echocardiography in acute infarction predicts recovery of resting function and contractile reserve</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>239</Ref_ID><Title_Primary>Detection of myocardial viability by contrast echocardiography in acute infarction predicts recovery of resting function and contractile reserve</Title_Primary><Authors_Primary>Balcells,E.</Authors_Primary><Authors_Primary>Powers,E.R.</Authors_Primary><Authors_Primary>Lepper,W.</Authors_Primary><Authors_Primary>Belcik,T.</Authors_Primary><Authors_Primary>Wei,K.</Authors_Primary><Authors_Primary>Ragosta,M.</Authors_Primary><Authors_Primary>Samady,H.</Authors_Primary><Authors_Primary>Lindner,J.R.</Authors_Primary><Date_Primary>2003/3/5</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Comparative Study</Keywords><Keywords>Contrast Media</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>diagnostic use</Keywords><Keywords>Dobutamine</Keywords><Keywords>Echocardiography</Keywords><Keywords>Echocardiography,Doppler</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>instrumentation</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Contraction</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Necrosis</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Prognosis</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Radiographic Image Enhancement</Keywords><Keywords>Recovery of Function</Keywords><Keywords>Research Support,Non-U.S.Gov't</Keywords><Keywords>Research Support,U.S.Gov't,P.H.S.</Keywords><Keywords>Sampling Studies</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>Severity of Illness Index</Keywords><Keywords>Stents</Keywords><Keywords>Systole</Keywords><Keywords>therapy</Keywords><Keywords>Treatment Outcome</Keywords><Keywords>ultrasonography</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>827</Start_Page><End_Page>833</End_Page><Periodical>J Am.Coll.Cardiol.</Periodical><Volume>41</Volume><Issue>5</Issue><Address>Cardiovascular Division, University of Virginia, Charlottesville, Virginia 22908, USA</Address><Web_URL>PM:12628729</Web_URL><ZZ_JournalStdAbbrev><f name="System">J Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[80] and Tc 99m sestamibi scans have been used as a tool to predict late functional recovery following primary PTCA for acute myocardial infarction ADDIN REFMGR.CITE <Refman><Author>Christian</Author><Year>1999</Year><RecNum>2530</RecNum><IDText>Threshold values for preserved viability with a noninvasive measurement of collateral blood flow during acute myocardial infarction treated by direct coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2530</Ref_ID><Title_Primary>Threshold values for preserved viability with a noninvasive measurement of collateral blood flow during acute myocardial infarction treated by direct coronary angioplasty</Title_Primary><Authors_Primary>Christian,T.F.</Authors_Primary><Authors_Primary>Berger,P.B.</Authors_Primary><Authors_Primary>O'Connor,M.K.</Authors_Primary><Authors_Primary>Hodge,D.O.</Authors_Primary><Authors_Primary>Gibbons,R.J.</Authors_Primary><Date_Primary>1999/12/14</Date_Primary><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>blood</Keywords><Keywords>Collateral Circulation</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>diagnostic use</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Perfusion</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Prospective Studies</Keywords><Keywords>radiography</Keywords><Keywords>radionuclide imaging</Keywords><Keywords>Reperfusion</Keywords><Keywords>Risk</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>Technetium</Keywords><Keywords>Technetium Tc 99m Sestamibi</Keywords><Keywords>therapy</Keywords><Keywords>Time</Keywords><Keywords>Tomography,X-Ray Computed</Keywords><Reprint>Not in File</Reprint><Start_Page>2392</Start_Page><End_Page>2395</End_Page><Periodical>Circulation</Periodical><Volume>100</Volume><Issue>24</Issue><Address>Mayo Clinic and Mayo Foundation, Rochester, MN 55905, USA. christian.timothy@mayo.edu</Address><Web_URL>PM:10595949</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Bolognese</Author><Year>1996</Year><RecNum>1815</RecNum><IDText>Myocardial contrast echocardiography versus dobutamine echocardiography for predicting functional recovery after acute myocardial infarction treated with primary coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1815</Ref_ID><Title_Primary>Myocardial contrast echocardiography versus dobutamine echocardiography for predicting functional recovery after acute myocardial infarction treated with primary coronary angioplasty</Title_Primary><Authors_Primary>Bolognese,L.</Authors_Primary><Authors_Primary>Antoniucci,D.</Authors_Primary><Authors_Primary>Rovai,D.</Authors_Primary><Authors_Primary>Buonamici,P.</Authors_Primary><Authors_Primary>Cerisano,G.</Authors_Primary><Authors_Primary>Santoro,G.M.</Authors_Primary><Authors_Primary>Marini,C.</Authors_Primary><Authors_Primary>L'Abbate,A.</Authors_Primary><Authors_Primary>Fazzini,P.F.</Authors_Primary><Date_Primary>1996/12</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Aged,80 and over</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Cardiology</Keywords><Keywords>Cardiotonic Agents</Keywords><Keywords>Comparative Study</Keywords><Keywords>Contrast Media</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>diagnostic use</Keywords><Keywords>Dobutamine</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Iopamidol</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Contraction</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Reperfusion</Keywords><Keywords>Reproducibility of Results</Keywords><Keywords>Risk</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>Stroke Volume</Keywords><Keywords>therapy</Keywords><Keywords>ultrasonography</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1677</Start_Page><End_Page>1683</End_Page><Periodical>J.Am.Coll.Cardiol.</Periodical><Volume>28</Volume><Issue>7</Issue><Address>Division of Cardiology, Careggi Hospital, Florence, Italy. carddept@mbox.vol.it</Address><Web_URL>PM:8962551</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL><Author>Brodie</Author><Year>1998</Year><RecNum>2537</RecNum><IDText>Importance of time to reperfusion for 30-day and late survival and recovery of left ventricular function after primary angioplasty for acute myocardial infarction</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2537</Ref_ID><Title_Primary>Importance of time to reperfusion for 30-day and late survival and recovery of left ventricular function after primary angioplasty for acute myocardial infarction</Title_Primary><Authors_Primary>Brodie,B.R.</Authors_Primary><Authors_Primary>Stuckey,T.D.</Authors_Primary><Authors_Primary>Wall,T.C.</Authors_Primary><Authors_Primary>Kissling,G.</Authors_Primary><Authors_Primary>Hansen,C.J.</Authors_Primary><Authors_Primary>Muncy,D.B.</Authors_Primary><Authors_Primary>Weintraub,R.A.</Authors_Primary><Authors_Primary>Kelly,T.A.</Authors_Primary><Date_Primary>1998/11</Date_Primary><Keywords>Aged</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Aspirin</Keywords><Keywords>Catheterization</Keywords><Keywords>Cause of Death</Keywords><Keywords>Comparative Study</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Drug Therapy,Combination</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Fibrinolytic Agents</Keywords><Keywords>Follow-Up Studies</Keywords><Keywords>Heart Catheterization</Keywords><Keywords>Heparin</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>North Carolina</Keywords><Keywords>Observation</Keywords><Keywords>physiology</Keywords><Keywords>physiopathology</Keywords><Keywords>Reperfusion</Keywords><Keywords>Research</Keywords><Keywords>Retrospective Studies</Keywords><Keywords>Stroke Volume</Keywords><Keywords>Survival</Keywords><Keywords>Survival Rate</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Thrombolytic Therapy</Keywords><Keywords>Time</Keywords><Keywords>Time Factors</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1312</Start_Page><End_Page>1319</End_Page><Periodical>J.Am.Coll.Cardiol</Periodical><Volume>32</Volume><Issue>5</Issue><Address>Department of Medicine, The Moses H. Cone Memorial Hospital, University of North Carolina at Greensboro, USA</Address><Web_URL>PM:9809941</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[81-83]. Dobutamine stress echocardiography (DSE) performed 3 days following an index myocardial infarction might be a better tool in the assessment of myocardial recovery compared with myocardial contrast echocardiography (MCE). In a study by Bolognese et al, the overall accuracy of predicting late functional recovery was 47% with MCE and 90% with DSE (p<0.001) ADDIN REFMGR.CITE <Refman><Author>Bolognese</Author><Year>1996</Year><RecNum>1815</RecNum><IDText>Myocardial contrast echocardiography versus dobutamine echocardiography for predicting functional recovery after acute myocardial infarction treated with primary coronary angioplasty</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1815</Ref_ID><Title_Primary>Myocardial contrast echocardiography versus dobutamine echocardiography for predicting functional recovery after acute myocardial infarction treated with primary coronary angioplasty</Title_Primary><Authors_Primary>Bolognese,L.</Authors_Primary><Authors_Primary>Antoniucci,D.</Authors_Primary><Authors_Primary>Rovai,D.</Authors_Primary><Authors_Primary>Buonamici,P.</Authors_Primary><Authors_Primary>Cerisano,G.</Authors_Primary><Authors_Primary>Santoro,G.M.</Authors_Primary><Authors_Primary>Marini,C.</Authors_Primary><Authors_Primary>L'Abbate,A.</Authors_Primary><Authors_Primary>Fazzini,P.F.</Authors_Primary><Date_Primary>1996/12</Date_Primary><Keywords>Adult</Keywords><Keywords>Aged</Keywords><Keywords>Aged,80 and over</Keywords><Keywords>Angiography</Keywords><Keywords>Angioplasty</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Arteries</Keywords><Keywords>Cardiology</Keywords><Keywords>Cardiotonic Agents</Keywords><Keywords>Comparative Study</Keywords><Keywords>Contrast Media</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>diagnostic use</Keywords><Keywords>Dobutamine</Keywords><Keywords>Echocardiography</Keywords><Keywords>Electrocardiography</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Iopamidol</Keywords><Keywords>Italy</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Myocardial Contraction</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Prospective Studies</Keywords><Keywords>Reperfusion</Keywords><Keywords>Reproducibility of Results</Keywords><Keywords>Risk</Keywords><Keywords>Sensitivity and Specificity</Keywords><Keywords>Stroke Volume</Keywords><Keywords>therapy</Keywords><Keywords>ultrasonography</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>1677</Start_Page><End_Page>1683</End_Page><Periodical>J.Am.Coll.Cardiol.</Periodical><Volume>28</Volume><Issue>7</Issue><Address>Division of Cardiology, Careggi Hospital, Florence, Italy. carddept@mbox.vol.it</Address><Web_URL>PM:8962551</Web_URL><ZZ_JournalStdAbbrev><f name="System">J.Am.Coll.Cardiol.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[82]. Myocardial perfusion imaging using Tc 99m sestamibi scans can be used to identify patients at increased risk for large infarcts. This was indeed demonstrated by Kaltoft et al in a study where assessment of tissue perfusion by Tc 99m sestamibi scans was an independent predictor of infarct size after successful PTCA following an acute myocardial infarction ADDIN REFMGR.CITE <Refman><Author>Kaltoft</Author><Year>2006</Year><RecNum>1820</RecNum><IDText>Sestamibi single photon emission computed tomography immediately after primary percutaneous coronary intervention identifies patients at risk for large infarcts</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1820</Ref_ID><Title_Primary>Sestamibi single photon emission computed tomography immediately after primary percutaneous coronary intervention identifies patients at risk for large infarcts</Title_Primary><Authors_Primary>Kaltoft,A.</Authors_Primary><Authors_Primary>Bottcher,M.</Authors_Primary><Authors_Primary>Sand,N.P.</Authors_Primary><Authors_Primary>Rehling,M.</Authors_Primary><Authors_Primary>Andersen,N.T.</Authors_Primary><Authors_Primary>Zijlstra,F.</Authors_Primary><Authors_Primary>Nielsen,T.T.</Authors_Primary><Date_Primary>2006/5</Date_Primary><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Denmark</Keywords><Keywords>diagnosis</Keywords><Keywords>diagnostic use</Keywords><Keywords>Electrocardiography</Keywords><Keywords>etiology</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Perfusion</Keywords><Keywords>physiopathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Radiopharmaceuticals</Keywords><Keywords>Recurrence</Keywords><Keywords>Research</Keywords><Keywords>Risk</Keywords><Keywords>Risk Factors</Keywords><Keywords>Technetium</Keywords><Keywords>Technetium Tc 99m Sestamibi</Keywords><Keywords>therapy</Keywords><Keywords>Tomography,Emission-Computed,Single-Photon</Keywords><Reprint>Not in File</Reprint><Start_Page>1108</Start_Page><End_Page>1114</End_Page><Periodical>Am.Heart J.</Periodical><Volume>151</Volume><Issue>5</Issue><Address>Department of Cardiology, Aarhus University Hospital, Skejby, Denmark</Address><Web_URL>PM:16644346</Web_URL><ZZ_JournalStdAbbrev><f name="System">Am.Heart J.</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[84].
Angiographic assessment of myocardial perfusion
Angiographic assessment by TIMI myocardial perfusion grade ADDIN REFMGR.CITE <Refman><Author>Gibson</Author><Year>2000</Year><RecNum>101</RecNum><IDText>Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>101</Ref_ID><Title_Primary>Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs</Title_Primary><Authors_Primary>Gibson,C.M.</Authors_Primary><Authors_Primary>Cannon,C.P.</Authors_Primary><Authors_Primary>Murphy,S.A.</Authors_Primary><Authors_Primary>Ryan,K.A.</Authors_Primary><Authors_Primary>Mesley,R.</Authors_Primary><Authors_Primary>Marble,S.J.</Authors_Primary><Authors_Primary>McCabe,C.H.</Authors_Primary><Authors_Primary>Van de,Werf F.</Authors_Primary><Authors_Primary>Braunwald,E.</Authors_Primary><Date_Primary>2000/1/18</Date_Primary><Keywords>Aged</Keywords><Keywords>Antifibrinolytic Agents</Keywords><Keywords>blood</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>drug effects</Keywords><Keywords>drug therapy</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardium</Keywords><Keywords>Perfusion</Keywords><Keywords>Pericardium</Keywords><Keywords>physiopathology</Keywords><Keywords>radiography</Keywords><Keywords>Randomized Controlled Trials</Keywords><Keywords>Risk</Keywords><Keywords>Risk Assessment</Keywords><Keywords>therapeutic use</Keywords><Reprint>Not in File</Reprint><Start_Page>125</Start_Page><End_Page>130</End_Page><Periodical>Circulation</Periodical><Volume>101</Volume><Issue>2</Issue><Address>Cardiovascular Divisions of the Departments of Medicine, the University of California at San Francisco, San Francisco 94118, USA</Address><Web_URL>PM:10637197</Web_URL><ZZ_JournalStdAbbrev><f name="System">Circulation</f></ZZ_JournalStdAbbrev><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[85] and myocardial blush grade has been developed as a simple tool to assess myocardial perfusion in the cardiac catheterization laboratory. In a previous study van’t Hof et al demonstrated that myocardial blush grade (MBG) measured during primary angioplasty was a predictor of long-term mortality. The mortality at a mean±SD follow-up of 1.9±1.7 years for patients with MBG 3 (normal blush) was significantly lower compared to those who had MBG 2 (moderate blush) and MBG 0/1 (no blush/minimal blush) [3%, vs. 6%, vs. 23%, <0.0001 respectively] ADDIN REFMGR.CITE <Refman><Author>van 't Hof</Author><Year>1998</Year><RecNum>2540</RecNum><IDText>Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>2540</Ref_ID><Title_Primary>Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group</Title_Primary><Authors_Primary>van 't Hof,A.W.</Authors_Primary><Authors_Primary>Liem,A.</Authors_Primary><Authors_Primary>Suryapranata,H.</Authors_Primary><Authors_Primary>Hoorntje,J.C.</Authors_Primary><Authors_Primary>de Boer,M.J.</Authors_Primary><Authors_Primary>Zijlstra,F.</Authors_Primary><Date_Primary>1998/6/16</Date_Primary><Keywords>Aged</Keywords><Keywords>analysis</Keywords><Keywords>Angioplasty</Keywords><Keywords>Arteries</Keywords><Keywords>blood</Keywords><Keywords>Cardiology</Keywords><Keywords>Coronary Angiography</Keywords><Keywords>Coronary Circulation</Keywords><Keywords>diagnosis</Keywords><Keywords>Electrocardiography</Keywords><Keywords>enzymology</Keywords><Keywords>Female</Keywords><Keywords>Humans</Keywords><Keywords>Infarction</Keywords><Keywords>L-Lactate Dehydrogenase</Keywords><Keywords>Male</Keywords><Keywords>methods</Keywords><Keywords>Middle Aged</Keywords><Keywords>mortality</Keywords><Keywords>Multivariate Analysis</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Myocardium</Keywords><Keywords>Netherlands</Keywords><Keywords>pathology</Keywords><Keywords>Predictive Value of Tests</Keywords><Keywords>Prognosis</Keywords><Keywords>Reperfusion</Keywords><Keywords>Stroke Volume</Keywords><Keywords>therapy</Keywords><Keywords>Ventricular Function</Keywords><Keywords>Ventricular Function,Left</Keywords><Reprint>Not in File</Reprint><Start_Page>2302</Start_Page><End_Page>2306</End_Page><Periodical>Circulation</Periodical><Volume>97</Volume><Issue>23</Issue><Address>Department of Cardiology, Hospital De Weezenlanden, Zwolle, The Netherlands</Address><Web_URL>PM:9639373</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[86]. Another study from the same group demonstrated that combined major adverse cardiac events (death, reinfarction and target vessel revascularization) were significantly increased at 16±11 months among those with MBG 0/1 compared to those with MBG 2/3 following primary angioplasty for acute myocardial infarction (relative risk 1.8, 95% confidence interval 1.1-2.8, p=0.009) ADDIN REFMGR.CITE <Refman><Author>Henriques</Author><Year>2003</Year><RecNum>149</RecNum><IDText>Angiographic assessment of reperfusion in acute myocardial infraction by myocardial blush grade</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>149</Ref_ID><Title_Primary>Angiographic assessment of reperfusion in acute myocardial infraction by myocardial blush grade</Title_Primary><Authors_Primary>Henriques,J</Authors_Primary><Authors_Primary>Zijlstra,F</Authors_Primary><Authors_Primary>van't Hof,A</Authors_Primary><Authors_Primary>de Boer,M</Authors_Primary><Authors_Primary>Dambrink,J</Authors_Primary><Authors_Primary>Gosselink,M</Authors_Primary><Date_Primary>2003</Date_Primary><Reprint>In File</Reprint><Start_Page>2115</Start_Page><End_Page>2119</End_Page><Periodical>Circulation</Periodical><Volume>107</Volume><Issue>16</Issue><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[87].
Recommendations
The 2007 focused update of the American College of Cardiology/American Heart Association 2004 guidelines for the management of STEMI provides a class 1 recommendation for the performance of primary PCI for STEMI patients presenting to a hospital with PCI facility within 90 minutes of initial medical contact (Level of evidence A) ADDIN REFMGR.CITE <Refman><Author>Antman</Author><Year>2008</Year><RecNum>1662</RecNum><IDText>2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee</IDText><MDL Ref_Type="Journal"><Ref_Type>Journal</Ref_Type><Ref_ID>1662</Ref_ID><Title_Primary>2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee</Title_Primary><Authors_Primary>Antman,E.M.</Authors_Primary><Authors_Primary>Hand,M.</Authors_Primary><Authors_Primary>Armstrong,P.W.</Authors_Primary><Authors_Primary>Bates,E.R.</Authors_Primary><Authors_Primary>Green,L.A.</Authors_Primary><Authors_Primary>Halasyamani,L.K.</Authors_Primary><Authors_Primary>Hochman,J.S.</Authors_Primary><Authors_Primary>Krumholz,H.M.</Authors_Primary><Authors_Primary>Lamas,G.A.</Authors_Primary><Authors_Primary>Mullany,C.J.</Authors_Primary><Authors_Primary>Pearle,D.L.</Authors_Primary><Authors_Primary>Sloan,M.A.</Authors_Primary><Authors_Primary>Smith,S.C.,Jr.</Authors_Primary><Authors_Primary>Anbe,D.T.</Authors_Primary><Authors_Primary>Kushner,F.G.</Authors_Primary><Authors_Primary>Ornato,J.P.</Authors_Primary><Authors_Primary>Jacobs,A.K.</Authors_Primary><Authors_Primary>Adams,C.D.</Authors_Primary><Authors_Primary>Anderson,J.L.</Authors_Primary><Authors_Primary>Buller,C.E.</Authors_Primary><Authors_Primary>Creager,M.A.</Authors_Primary><Authors_Primary>Ettinger,S.M.</Authors_Primary><Authors_Primary>Halperin,J.L.</Authors_Primary><Authors_Primary>Hunt,S.A.</Authors_Primary><Authors_Primary>Lytle,B.W.</Authors_Primary><Authors_Primary>Nishimura,R.</Authors_Primary><Authors_Primary>Page,R.L.</Authors_Primary><Authors_Primary>Riegel,B.</Authors_Primary><Authors_Primary>Tarkington,L.G.</Authors_Primary><Authors_Primary>Yancy,C.W.</Authors_Primary><Date_Primary>2008/1/15</Date_Primary><Keywords>Adrenergic beta-Antagonists</Keywords><Keywords>American Heart Association</Keywords><Keywords>Angioplasty,Transluminal,Percutaneous Coronary</Keywords><Keywords>Anticoagulants</Keywords><Keywords>Combined Modality Therapy</Keywords><Keywords>Disease Management</Keywords><Keywords>Heart</Keywords><Keywords>Infarction</Keywords><Keywords>Myocardial Infarction</Keywords><Keywords>Myocardial Reperfusion</Keywords><Keywords>Physicians</Keywords><Keywords>Platelet Aggregation Inhibitors</Keywords><Keywords>Practice Guidelines</Keywords><Keywords>therapeutic use</Keywords><Keywords>therapy</Keywords><Keywords>Writing</Keywords><Reprint>Not in File</Reprint><Start_Page>296</Start_Page><End_Page>329</End_Page><Periodical>Circulation</Periodical><Volume>117</Volume><Issue>2</Issue><Web_URL>PM:18071078</Web_URL><ZZ_JournalFull><f name="System">Circulation</f></ZZ_JournalFull><ZZ_WorkformID>1</ZZ_WorkformID></MDL></Refman>[88].
Conclusions
Primary angioplasty is the optimal management strategy for patients with acute myocardial infarction and is associated with reduction in mortality and bleeding events.
ADDIN REFMGR.REFLIST Reference List
1. Davies MJ, Woolf N, Robertson WB (1976) Pathology of acute myocardial infarction with particular reference to occlusive coronary thrombi. Br Heart J 38:659-664
2. Reimer KA, Lowe JE, Rasmussen MM, Jennings RB (1977) The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. Circulation 56:786-794
3. (1994) Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Lancet 343:311-322
4. Topol EJ, Califf RM, George BS, Kereiakes DJ, Abbottsmith CW, Candela RJ, Lee KL, Pitt B, Stack RS, O'Neill WW (1987) A randomized trial of immediate versus delayed elective angioplasty after intravenous tissue plasminogen activator in acute myocardial infarction. N Engl J Med 317:581-588
5. Simoons ML, Arnold AE, Betriu A, de Bono DP, Col J, Dougherty FC, von ER, Lambertz H, Lubsen J, Meier B, . (1988) Thrombolysis with tissue plasminogen activator in acute myocardial infarction: no additional benefit from immediate percutaneous coronary angioplasty. Lancet 1:197-203
6. Cannon CP, Bahit M, Haugland JM, Henry TD, Schweiger MJ, McKendall G, Shah PK, Murphy SA, Gibson CM, McCabe CH, Antman E, Braunwald E (2002) Under-utilization of evidence based medications in acute ST elevation myocardial infarction. Results of the Thrombolysis in Myocardial Infarction (TIMI 9) registry. Crit Pathways Cardiol 1:44-52
7. Weaver WD, Cerqueira M, Hallstrom AP, Litwin PE, Martin JS, Kudenchuk PJ, Eisenberg M (1993) Prehospital-initiated vs hospital-initiated thrombolytic therapy. The Myocardial Infarction Triage and Intervention Trial. JAMA 270:1211-1216
8. Boersma E, Maas AC, Deckers JW, Simoons ML (1996) Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 348:771-775
9. Gore JM, Granger CB, Simoons ML, Sloan MA, Weaver WD, White HD, Barbash GI, Van de WF, Aylward PE, Topol EJ, . (1995) Stroke after thrombolysis. Mortality and functional outcomes in the GUSTO-I trial. Global Use of Strategies to Open Occluded Coronary Arteries. Circulation 92:2811-2818
10. Gurwitz JH, Gore JM, Goldberg RJ, Barron HV, Breen T, Rundle AC, Sloan MA, French W, Rogers WJ (1998) Risk for intracranial hemorrhage after tissue plasminogen activator treatment for acute myocardial infarction. Participants in the National Registry of Myocardial Infarction 2. Ann Intern Med 129:597-604
11. (1993) The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. The GUSTO Angiographic Investigators. N Engl J Med 329:1615-1622
12. Hudson MP, Granger CB, Topol EJ, Pieper KS, Armstrong PW, Barbash GI, Guerci AD, Vahanian A, Califf RM, Ohman EM (2001) Early reinfarction after fibrinolysis: experience from the global utilization of streptokinase and tissue plasminogen activator (alteplase) for occluded coronary arteries (GUSTO I) and global use of strategies to open occluded coronary arteries (GUSTO III) trials. Circulation 104:1229-1235
13. O'Neill W, Timmis GC, Bourdillon PD, Lai P, Ganghadarhan V, Walton J, Jr., Ramos R, Laufer N, Gordon S, Schork MA, . (1986) A prospective randomized clinical trial of intracoronary streptokinase versus coronary angioplasty for acute myocardial infarction. N Engl J Med 314:812-818
14. Michels KB, Yusuf S (1995) Does PTCA in acute myocardial infarction affect mortality and reinfarction rates? A quantitative overview (meta-analysis) of the randomized clinical trials. Circulation 91:476-485
15. Weaver WD, Simes RJ, Betriu A, Grines CL, Zijlstra F, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, DeWood MA, Ribichini F (1997) Comparison of primary coronary angioplasty and intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review. JAMA 278:2093-2098
16. (1997) A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTO IIb) Angioplasty Substudy Investigators. N Engl J Med 336:1621-1628
17. Grines CL, Browne KF, Marco J, Rothbaum D, Stone GW, O'Keefe J, Overlie P, Donohue B, Chelliah N, Timmis GC, . (1993) A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group. N Engl J Med 328:673-679
18. Zijlstra F, Hoorntje JC, de Boer MJ, Reiffers S, Miedema K, Ottervanger JP, van't Hof AW, Suryapranata H (1999) Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med 341:1413-1419
19. Keeley EC, Boura JA, Grines CL (2003) Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361:13-20
20. Kernis SJ, Harjai KJ, Stone GW, Grines LL, Boura JA, Yerkey MW, O'Neill W, Grines CL (2003) The incidence, predictors, and outcomes of early reinfarction after primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 42:1173-1177
21. Stenestrand U, Lindback J, Wallentin L (2006) Long-term outcome of primary percutaneous coronary intervention vs prehospital and in-hospital thrombolysis for patients with ST-elevation myocardial infarction. JAMA 296:1749-1756
22. Stone GW, Brodie BR, Griffin JJ, Morice MC, Costantini C, St Goar FG, Overlie PA, Popma JJ, McDonnell J, Jones D, O'Neill WW, Grines CL (1998) Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators. J Am Coll Cardiol 31:23-30
23. Stone GW, Brodie BR, Griffin JJ, Costantini C, Morice MC, St Goar FG, Overlie PA, Popma JJ, McDonnell J, Jones D, O'Neill WW, Grines CL (1999) Clinical and angiographic follow-Up after primary stenting in acute myocardial infarction: the Primary Angioplasty in Myocardial Infarction (PAMI) stent pilot trial. Circulation 99:1548-1554
24. Schomig A, Kastrati A, Dirschinger J, Mehilli J, Schricke U, Pache J, Martinoff S, Neumann FJ, Schwaiger M (2000) Coronary stenting plus platelet glycoprotein IIb/IIIa blockade compared with tissue plasminogen activator in acute myocardial infarction. Stent versus Thrombolysis for Occluded Coronary Arteries in Patients with Acute Myocardial Infarction Study Investigators. N Engl J Med 343:385-391
25. Spaulding C, Henry P, Teiger E, Beatt K, Bramucci E, Carrie D, Slama MS, Merkely B, Erglis A, Margheri M, Varenne O, Cebrian A, Stoll HP, Snead DB, Bode C (2006) Sirolimus-eluting versus uncoated stents in acute myocardial infarction. N Engl J Med 355:1093-1104
26. Menichelli M, Parma A, Pucci E, Fiorilli R, De FF, Nazzaro M, Giulivi A, Alborino D, Azzellino A, Violini R (2007) Randomized trial of Sirolimus-Eluting Stent Versus Bare-Metal Stent in Acute Myocardial Infarction (SESAMI). J Am Coll Cardiol 49:1924-1930
27. Valgimigli M, Percoco G, Malagutti P, Campo G, Ferrari F, Barbieri D, Cicchitelli G, McFadden EP, Merlini F, Ansani L, Guardigli G, Bettini A, Parrinello G, Boersma E, Ferrari R (2005) Tirofiban and sirolimus-eluting stent vs abciximab and bare-metal stent for acute myocardial infarction: a randomized trial. JAMA 293:2109-2117
28. Laarman GJ, Suttorp MJ, Dirksen MT, van HL, Kiemeneij F, Slagboom T, van der Wieken LR, Tijssen JG, Rensing BJ, Patterson M (2006) Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention. N Engl J Med 355:1105-1113
29. Brener SJ, Barr LA, Burchenal JE, Katz S, George BS, Jones AA, Cohen ED, Gainey PC, White HJ, Cheek HB, Moses JW, Moliterno DJ, Effron MB, Topol EJ (1998) Randomized, placebo-controlled trial of platelet glycoprotein IIb/IIIa blockade with primary angioplasty for acute myocardial infarction. ReoPro and Primary PTCA Organization and Randomized Trial (RAPPORT) Investigators. Circulation 98:734-741
30. Montalescot G, Barragan P, Wittenberg O, Ecollan P, Elhadad S, Villain P, Boulenc JM, Morice MC, Maillard L, Pansieri M, Choussat R, Pinton P (2001) Platelet glycoprotein IIb/IIIa inhibition with coronary stenting for acute myocardial infarction. N Engl J Med 344:1895-1903
31. Piana RN, Paik GY, Moscucci M, Cohen DJ, Gibson CM, Kugelmass AD, Carrozza JP, Jr., Kuntz RE, Baim DS (1994) Incidence and treatment of 'no-reflow' after percutaneous coronary intervention. Circulation 89:2514-2518
32. Gregorini L, Marco J, Kozakova M, Palombo C, Anguissola GB, Marco I, Bernies M, Cassagneau B, Distante A, Bossi IM, Fajadet J, Heusch G (1999) Alpha-adrenergic blockade improves recovery of myocardial perfusion and function after coronary stenting in patients with acute myocardial infarction. Circulation 99:482-490
33. Gregorini L, Marco J, Farah B, Bernies M, Palombo C, Kozakova M, Bossi IM, Cassagneau B, Fajadet J, Di MC, Albiero R, Cugno M, Grossi A, Heusch G (2002) Effects of selective alpha1- and alpha2-adrenergic blockade on coronary flow reserve after coronary stenting. Circulation 106:2901-2907
34. Sezgin AT, Sigirci A, Barutcu I, Topal E, Sezgin N, Ozdemir R, Yetkin E, Tandogan I, Kosar F, Ermis N, Yologlu S, Bariskaner E, Cehreli S (2003) Vascular endothelial function in patients with slow coronary flow. Coron Artery Dis 14:155-161
35. Pekdemir H, Cicek D, Camsari A, Akkus MN, Cin VG, Doven O, Parmaksiz HT, Katircibasi MT, Ozcan IT (2004) The relationship between plasma endothelin-1, nitric oxide levels, and heart rate variability in patients with coronary slow flow. Ann Noninvasive Electrocardiol 9:24-33
36. Turhan H, Saydam GS, Erbay AR, Ayaz S, Yasar AS, Aksoy Y, Basar N, Yetkin E (2006) Increased plasma soluble adhesion molecules; ICAM-1, VCAM-1, and E-selectin levels in patients with slow coronary flow. Int J Cardiol 108:224-230
37. Barutcu I, Sezgin AT, Sezgin N, Gullu H, Esen AM, Topal E, Ozdemir R (2005) Elevated plasma homocysteine level in slow coronary flow. Int J Cardiol 101:143-145
38. Selcuk MT, Selcuk H, Temizhan A, Maden O, Ulupinar H, Baysal E, Ozeke O, Sasmaz A (2007) Asymmetric dimethylarginine plasma concentrations and L-arginine/asymmetric dimethylarginine ratio in patients with slow coronary flow. Coron Artery Dis 18:545-551
39. Li JJ, Qin XW, Li ZC, Zeng HS, Gao Z, Xu B, Zhang CY, Li J (2007) Increased plasma C-reactive protein and interleukin-6 concentrations in patients with slow coronary flow. Clin Chim Acta 385:43-47
40. Eeckhout E, Kern MJM (2001) The coronary no-reflow: a review of mechanisms and therapies. European Heart Journal 22:729-739
41. Taniyama Y, Ito H, Iwakura K, Masuyama T, Hori M, Takiuchi S, Nishikawa N, Higashino Y, Fujii K, Minamino T (1997) Beneficial effect of intracoronary verapamil on microvascular and myocardial salvage in patients with acute myocardial infarction. J Am Coll Cardiol 30:1193-1199
42. Ota S, Nishikawa H, Takeuchi M, Nakajima K, Nakamura T, Okamoto S, Setsuda M, Makino K, Yamakado T, Nakano T (2006) Impact of nicorandil to prevent reperfusion injury in patients with acute myocardial infarction: Sigmart Multicenter Angioplasty Revascularization Trial (SMART). Circ J 70:1099-1104
43. Stoel MG, Marques KM, de Cock CC, Bronzwaer JG, von BC, Zijlstra F (2008) High dose adenosine for suboptimal myocardial reperfusion after primary PCI: A randomized placebo-controlled pilot study. Catheter Cardiovasc Interv 71:283-289
44. Wohrle J, Grebe OC, Nusser T, Al-Khayer E, Schaible S, Kochs M, Hombach V, Hoher M (2003) Reduction of major adverse cardiac events with intracoronary compared with intravenous bolus application of abciximab in patients with acute myocardial infarction or unstable angina undergoing coronary angioplasty. Circulation 107:1840-1843
45. Romagnoli E, Burzotta F, Trani C, Biondi-Zoccai GG, Giannico F, Crea F (2007) Rationale for intracoronary administration of abciximab. J Thromb Thrombolysis 23:57-63
46. Simon DI, Xu H, Ortlepp S, Rogers C, Rao NK (1997) 7E3 monoclonal antibody directed against the platelet glycoprotein IIb/IIIa cross-reacts with the leukocyte integrin Mac-1 and blocks adhesion to fibrinogen and ICAM-1. Arterioscler Thromb Vasc Biol 17:528-535
47. Kintscher U, Kappert K, Schmidt G, Doerr G, Grill M, Wollert-Wulf B, Graefe M, Fleck E, Graf K (2000) Effects of abciximab and tirofiban on vitronectin receptors in human endothelial and smooth muscle cells. Eur J Pharmacol 390:75-87
48. Pinto DS, Kirtane AJ, Ruocco NA, Deibele AJ, Shui A, Buros J, Murphy SA, Gibson CM (2005) Administration of intracoronary eptifibatide during ST-elevation myocardial infarction. Am J Cardiol 96:1494-1497
49. Sezer M, Oflaz H, Goren T, Okcular I, Umman B, Nisanci Y, Bilge AK, Sanli Y, Meric M, Umman S (2007) Intracoronary streptokinase after primary percutaneous coronary intervention. N Engl J Med 356:1823-1834
50. Beran G, Lang I, Schreiber W, Denk S, Stefenelli T, Syeda B, Maurer G, Glogar D, Siostrzonek P (2002) Intracoronary thrombectomy with the X-sizer catheter system improves epicardial flow and accelerates ST-segment resolution in patients with acute coronary syndrome: a prospective, randomized, controlled study. Circulation 105:2355-2360
51. Dudek D, Mielecki W, Legutko J, Chyrchel M, Sorysz D, Bartus S, Rzeszutko L, Dubiel JS (2004) Percutaneous thrombectomy with the RESCUE system in acute myocardial infarction. Kardiol Pol 61:523-533
52. Vijayalakshmi K, Kunadian B, Wright RA, Sutton AG, Hall JA, de Belder MA (2006) Successful thrombus extraction with the Rescue thrombus management system during acute percutaneous coronary intervention improves flow but does not necessarily restore optimal myocardial tissue perfusion. Catheter Cardiovasc Interv 67:879-886
53. Silva-Orrego P, Colombo P, Bigi R, Gregori D, Delgado A, Salvade P, Oreglia J, Orrico P, de BA, Piccalo G, Bossi I, Klugmann S (2006) Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction) study. J Am Coll Cardiol 48:1552-1559
54. Lefevre T, Garcia E, Reimers B, Lang I, di MC, Colombo A, Neumann FJ, Chavarri MV, Brunel P, Grube E, Thomas M, Glatt B, Ludwig J (2005) X-sizer for thrombectomy in acute myocardial infarction improves ST-segment resolution: results of the X-sizer in AMI for negligible embolization and optimal ST resolution (X AMINE ST) trial. J Am Coll Cardiol 46:246-252
55. Koch KT, Haeck JD, Van Der Schaaf RJ, Alidjan FM, Henriques JP, Baan J, Jr., Piek JJ, Van Der Wal AC, Tijssen JG, Sutsch G, de Winter RJ (2007) Proximal Embolic Protection With Aspiration in Percutaneous Corononary Intervention Using the Proxistrade mark Device. Rev Cardiovasc Med 8:160-166
56. Bartorelli AL, Trabattoni D, Galli S, Grancini L, Cozzi S, Ravagnani P (1999) Successful dissolution of occlusive coronary thrombus with local administration of abciximab during PTCA. Catheter Cardiovasc Interv 48:211-213
57. Stone G, Webb J, Cox D, Brodie B, Quereshi M, Lalynych A, Turco M, Schultheiss H, Dulas D, Rutherford B, Antoniucci D, Krucoff M, Gibbons R, Jones D, Lansky A, Mehran R, for the Enhanced Myocardial Efficacy and Recovery by Aspiration of Liberated Debris (EMERALD) Investigators (2005) Distal Microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction. JAMA 293:1063-1072
58. Limbruno U, Micheli A, De CM, Amoroso G, Rossini R, Palagi C, Di B, V, Petronio AS, Fontanini G, Mariani M (2003) Mechanical prevention of distal embolization during primary angioplasty: safety, feasibility, and impact on myocardial reperfusion. Circulation 108:171-176
59. Svilaas T, Vlaar PJ, van dH, I, Diercks GF, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F (2008) Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med 358:557-567
60. Kunadian B, Vijayalakshmi K, Dunning J, de Belder MA (2007) Meta-Analysis of Randomised Trials Comparing Anti-Embolic Devices with Standard PCI for Improving Myocardial Reperfusion in Patients with Acute Myocardial Infarction. Catheterizarion and Cardiovascular Interventions Accepted:
61. Lefroy DC, Wharton J, Crake T, Knock GA, Rutherford RA, Suzuki T, Morgan K, Polak JM, Poole-Wilson PA (1996) Regional changes in angiotensin II receptor density after experimental myocardial infarction. J Mol Cell Cardiol 28:429-440
62. Murohara T, Buerke M, Lefer AM (1994) Polymorphonuclear leukocyte-induced vasocontraction and endothelial dysfunction. Role of selectins. Arterioscler Thromb 14:1509-1519
63. Seydoux C, Goy JJ, Davies G (1993) Platelet and neutrophil imaging techniques in the investigation of the response to thrombolytic therapy and the no-reflow phenomenon. Am Heart J 125:1142-1147
64. Horie H, Takahashi M, Minai K, Izumi M, Takaoka A, Nozawa M, Yokohama H, Fujita T, Sakamoto T, Kito O, Okamura H, Kinoshita M (1998) Long-term beneficial effect of late reperfusion for acute anterior myocardial infarction with percutaneous transluminal coronary angioplasty. Circulation 98:2377-2382
65. Hochman JS, Lamas GA, Buller CE, Dzavik V, Reynolds HR, Abramsky SJ, Forman S, Ruzyllo W, Maggioni AP, White H, Sadowski Z, Carvalho AC, Rankin JM, Renkin JP, Steg PG, Mascette AM, Sopko G, Pfisterer ME, Leor J, Fridrich V, Mark DB, Knatterud GL (2006) Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 355:2395-2407
66. Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, Gore JM, Weaver WD, Rogers WJ, Tiefenbrunn AJ (2000) Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 283:2941-2947
67. Pinto DS, Kirtane AJ, Nallamothu BK, Murphy SA, Cohen DJ, Laham RJ, Cutlip DE, Bates ER, Frederick PD, Miller DP, Carrozza JP, Jr., Antman EM, Cannon CP, Gibson CM (2006) Hospital delays in reperfusion for ST-elevation myocardial infarction: implications when selecting a reperfusion strategy. Circulation 114:2019-2025
68. Shavelle DM, Rasouli ML, Frederick P, Gibson CM, French WJ (2005) Outcome in patients transferred for percutaneous coronary intervention (a national registry of myocardial infarction 2/3/4 analysis). Am J Cardiol 96:1227-1232
69. Canto JG, Every NR, Magid DJ, Rogers WJ, Malmgren JA, Frederick PD, French WJ, Tiefenbrunn AJ, Misra VK, Kiefe CI, Barron HV (2000) The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. N Engl J Med 342:1573-1580
70. Magid DJ, Calonge BN, Rumsfeld JS, Canto JG, Frederick PD, Every NR, Barron HV (2000) Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy. JAMA 284:3131-3138
71. Aversano T, Aversano LT, Passamani E, Knatterud GL, Terrin ML, Williams DO, Forman SA (2002) Thrombolytic therapy vs primary percutaneous coronary intervention for myocardial infarction in patients presenting to hospitals without on-site cardiac surgery: a randomized controlled trial. JAMA 287:1943-1951
72. Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, Thayssen P, Abildgaard U, Pedersen F, Madsen JK, Grande P, Villadsen AB, Krusell LR, Haghfelt T, Lomholt P, Husted SE, Vigholt E, Kjaergard HK, Mortensen LS (2003) A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 349:733-742
73. Widimsky P, Groch L, Zelizko M, Aschermann M, Bednar F, Suryapranata H (2000) Multicentre randomized trial comparing transport to primary angioplasty vs immediate thrombolysis vs combined strategy for patients with acute myocardial infarction presenting to a community hospital without a catheterization laboratory. The PRAGUE study. Eur Heart J 21:823-831
74. Santoro GM, Antoniucci D, Valenti R, Bolognese L, Buonamici P, Trapani M, Boddi V, Fazzini PF (1997) Rapid reduction of ST-segment elevation after successful direct angioplasty in acute myocardial infarction. Am J Cardiol 80:685-689
75. Santoro GM, Valenti R, Buonamici P, Bolognese L, Cerisano G, Moschi G, Trapani M, Antoniucci D, Fazzini PF (1998) Relation between ST-segment changes and myocardial perfusion evaluated by myocardial contrast echocardiography in patients with acute myocardial infarction treated with direct angioplasty. Am J Cardiol 82:932-937
76. Matetzky S, Novikov M, Gruberg L, Freimark D, Feinberg M, Elian D, Novikov I, Di SE, Agranat O, Har-Zahav Y, Rabinowitz B, Kaplinsky E, Hod H (1999) The significance of persistent ST elevation versus early resolution of ST segment elevation after primary PTCA. J Am Coll Cardiol 34:1932-1938
77. Claeys MJ, Bosmans J, Veenstra L, Jorens P, De R, Vrints CJ (1999) Determinants and prognostic implications of persistent ST-segment elevation after primary angioplasty for acute myocardial infarction: importance of microvascular reperfusion injury on clinical outcome. Circulation 99:1972-1977
78. Kawamoto T, Yoshida K, Akasaka T, Hozumi T, Takagi T, Kaji S, Ueda Y (1999) Can coronary blood flow velocity pattern after primary percutaneous transluminal coronary angioplasty [correction of angiography] predict recovery of regional left ventricular function in patients with acute myocardial infarction? Circulation 100:339-345
79. Takahashi T, Hiasa Y, Ohara Y, Miyazaki S, Ogura R, Miyajima H, Yuba K, Suzuki N, Hosokawa S, Kishi K, Ohtani R (2007) Usefulness of coronary flow reserve immediately after primary coronary angioplasty for acute myocardial infarction in predicting long-term adverse cardiac events. Am J Cardiol 100:806-811
80. Balcells E, Powers ER, Lepper W, Belcik T, Wei K, Ragosta M, Samady H, Lindner JR (2003) Detection of myocardial viability by contrast echocardiography in acute infarction predicts recovery of resting function and contractile reserve. J Am Coll Cardiol 41:827-833
81. Christian TF, Berger PB, O'Connor MK, Hodge DO, Gibbons RJ (1999) Threshold values for preserved viability with a noninvasive measurement of collateral blood flow during acute myocardial infarction treated by direct coronary angioplasty. Circulation 100:2392-2395
82. Bolognese L, Antoniucci D, Rovai D, Buonamici P, Cerisano G, Santoro GM, Marini C, L'Abbate A, Fazzini PF (1996) Myocardial contrast echocardiography versus dobutamine echocardiography for predicting functional recovery after acute myocardial infarction treated with primary coronary angioplasty. J Am Coll Cardiol 28:1677-1683
83. Brodie BR, Stuckey TD, Wall TC, Kissling G, Hansen CJ, Muncy DB, Weintraub RA, Kelly TA (1998) Importance of time to reperfusion for 30-day and late survival and recovery of left ventricular function after primary angioplasty for acute myocardial infarction. J Am Coll Cardiol 32:1312-1319
84. Kaltoft A, Bottcher M, Sand NP, Rehling M, Andersen NT, Zijlstra F, Nielsen TT (2006) Sestamibi single photon emission computed tomography immediately after primary percutaneous coronary intervention identifies patients at risk for large infarcts. Am Heart J 151:1108-1114
85. Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, McCabe CH, Van de WF, Braunwald E (2000) Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 101:125-130
86. van 't Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F (1998) Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation 97:2302-2306
87. Henriques J, Zijlstra F, van't Hof A, de Boer M, Dambrink J, Gosselink M (2003) Angiographic assessment of reperfusion in acute myocardial infraction by myocardial blush grade. Circulation 107:2115-2119
88. Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC, Jr., Anbe DT, Kushner FG, Ornato JP, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW (2008) 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation 117:296-329
References