Rapidly progressive glomerulonephritis pathophysiology: Difference between revisions
| Line 29: | Line 29: | ||
*** Example of diseases: polyangiitis with granulomatosis and polyarteritis nodosa. | *** Example of diseases: polyangiitis with granulomatosis and polyarteritis nodosa. | ||
While the majority of patients with pauci-immune RPGN indeed have elevated levels of ANCA, the remaining 20% of patients with the same disease do not. Interestingly, 30% of patients in remission continue to have elevated levels of ANCA. Both these problematic findings raise the question of the actual importance of ANCA in the pathogenesis of RPGN.<ref name="pmid11007827">{{cite journal| author=Hedger N, Stevens J, Drey N, Walker S, Roderick P| title=Incidence and outcome of pauci-immune rapidly progressive glomerulonephritis in Wessex, UK: a 10-year retrospective study. | journal=Nephrol Dial Transplant | year= 2000 | volume= 15 | issue= 10 | pages= 1593-9 | pmid=11007827 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11007827 }} </ref> A novel hypothesis currently suggests that RPGN is in fact a podocytopathy, defined as an intrinsic disease of the podocytes that normally maintains glomerular capillary membranes.<ref name="pmid14675045">{{cite journal| author=Yoshimoto K, Yokoyama H, Wada T, Furuichi K, Sakai N, Iwata Y et al.| title=Pathologic findings of initial biopsies reflect the outcomes of membranous nephropathy. | journal=Kidney Int | year= 2004 | volume= 65 | issue= 1 | pages= 148-53 | pmid=14675045 | doi=10.1111/j.1523-1755.2004.00403.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14675045 }} </ref> As such, it is thought that the CXCR4 and VHL-HIF pathway target gene expression in renal biopsies, based on experimental studies on mice.<ref name="pmid16906157">{{cite journal| author=Ding M, Cui S, Li C, Jothy S, Haase V, Steer BM et al.| title=Loss of the tumor suppressor Vhlh leads to upregulation of Cxcr4 and rapidly progressive glomerulonephritis in mice. | journal=Nat Med | year= 2006 | volume= 12 | issue= 9 | pages= 1081-7 | pmid=16906157 | doi=10.1038/nm1460 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16906157 }} </ref> | *The cause of [[renal injury]] is due to [[Anti-glomerular basement membrane antibody|anti-glomerular basement membrane antibodies]] ability to bind and activate [[complement system]] and [[proteases]], resulting in an interruption between the [[filtration]] barrier and the [[Bowman's capsule|Bowman’s capsule]]. | ||
*The interruption of the [[Bowman's capsule]] and [[filtration]] barrier, induces [[Crescentic glomerulonephritis|crescent]] shaped antigen-antibody complex formation in the [[Renal corpuscles|renal corpuscles,]] invoking [[proteinuria]] and activating [[T cells]] ([[CD4+]] and [[CD8+ T cells|CD8+]]), [[macrophages]], and [[neutrophils]].<ref name="pmid12815141">{{cite journal |vauthors=Hudson BG, Tryggvason K, Sundaramoorthy M, Neilson EG |title=Alport's syndrome, Goodpasture's syndrome, and type IV collagen |journal=N. Engl. J. Med. |volume=348 |issue=25 |pages=2543–56 |date=June 2003 |pmid=12815141 |doi=10.1056/NEJMra022296 |url=}}</ref><ref name="pmid21168945">{{cite journal |vauthors=Cui Z, Zhao J, Jia XY, Zhu SN, Zhao MH |title=Clinical features and outcomes of anti-glomerular basement membrane disease in older patients |journal=Am. J. Kidney Dis. |volume=57 |issue=4 |pages=575–82 |date=April 2011 |pmid=21168945 |doi=10.1053/j.ajkd.2010.09.022 |url=}}</ref> | |||
*While the majority of patients with pauci-immune RPGN indeed have elevated levels of ANCA, the remaining 20% of patients with the same disease do not. Interestingly, 30% of patients in remission continue to have elevated levels of ANCA. Both these problematic findings raise the question of the actual importance of ANCA in the pathogenesis of RPGN.<ref name="pmid11007827">{{cite journal| author=Hedger N, Stevens J, Drey N, Walker S, Roderick P| title=Incidence and outcome of pauci-immune rapidly progressive glomerulonephritis in Wessex, UK: a 10-year retrospective study. | journal=Nephrol Dial Transplant | year= 2000 | volume= 15 | issue= 10 | pages= 1593-9 | pmid=11007827 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11007827 }} </ref> A novel hypothesis currently suggests that RPGN is in fact a podocytopathy, defined as an intrinsic disease of the podocytes that normally maintains glomerular capillary membranes.<ref name="pmid14675045">{{cite journal| author=Yoshimoto K, Yokoyama H, Wada T, Furuichi K, Sakai N, Iwata Y et al.| title=Pathologic findings of initial biopsies reflect the outcomes of membranous nephropathy. | journal=Kidney Int | year= 2004 | volume= 65 | issue= 1 | pages= 148-53 | pmid=14675045 | doi=10.1111/j.1523-1755.2004.00403.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14675045 }} </ref> As such, it is thought that the CXCR4 and VHL-HIF pathway target gene expression in renal biopsies, based on experimental studies on mice.<ref name="pmid16906157">{{cite journal| author=Ding M, Cui S, Li C, Jothy S, Haase V, Steer BM et al.| title=Loss of the tumor suppressor Vhlh leads to upregulation of Cxcr4 and rapidly progressive glomerulonephritis in mice. | journal=Nat Med | year= 2006 | volume= 12 | issue= 9 | pages= 1081-7 | pmid=16906157 | doi=10.1038/nm1460 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16906157 }} </ref> | |||
== Microscopic pathology == | == Microscopic pathology == | ||
Revision as of 19:55, 5 June 2018
|
Rapidly progressive glomerulonephritis Microchapters |
|
Differentiating Rapidly progressive glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Rapidly progressive glomerulonephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Rapidly progressive glomerulonephritis pathophysiology |
|
FDA on Rapidly progressive glomerulonephritis pathophysiology |
|
CDC on Rapidly progressive glomerulonephritis pathophysiology |
|
Rapidly progressive glomerulonephritis pathophysiology in the news |
|
Blogs on Rapidly progressive glomerulonephritis pathophysiology |
|
Directions to Hospitals Treating Rapidly progressive glomerulonephritis |
|
Risk calculators and risk factors for Rapidly progressive glomerulonephritis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
Anatomy
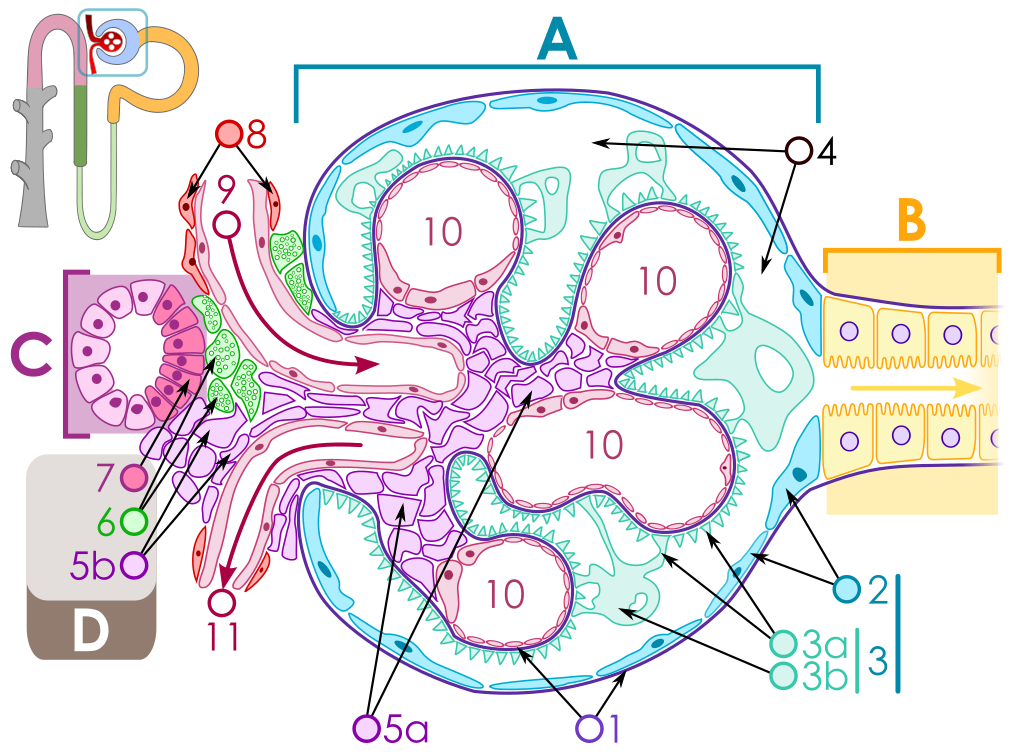
The key for the renal corpuscle figure is: A – Renal corpuscle, B – Proximal tubule, C – Distal convoluted tubule, D – Juxtaglomerular apparatus, 1. Basement membrane (Basal lamina), 2. Bowman's capsule – parietal layer, 3. Bowman's capsule – visceral layer, 3a. Pedicels (Foot processes from podocytes), 3b. Podocyte, 4. Bowman's space (urinary space), 5a. Mesangium – Intraglomerular cell, 5b. Mesangium – Extraglomerular cell, 6. Granular cells (Juxtaglomerular cells), 7. Macula densa, 8. Myocytes (smooth muscle), 9. Afferent arteriole, 10. Glomerulus Capillaries, 11. Efferent arteriole.
Pathogenesis
- Although the pathogenesis of RPGN is poorly understood, it is thought that some circulating factors have a significant role in the progression of the glomerulonephritis.[1]
- The pathophysiology of RPGN is considered as a combination of pathways that lead to the glomerular injury as an outcome. Genetic susceptibility has been shown to be associated with elevated levels of circulating antibodies, such as anti-GBM and ANCA, but little has been elaborated.[2]
- The pathogenesis according to the different types of RPGN as the following:
- Type I anti-GBM glomerulonephritis:[3][4][5]
- Antibodies against non-collagenous domain of alpha 3 chain of type IV collagen of the glomerular basement membrane.
- Linear pattern on immunofluorescence which indicates deposition of IgG and C3.
- This type is predominent in Goodpasture syndrome.
- Type II pauci-immune glomerulonephritis: [1][6][7][8]
- Findings of p-ANCA and c-ANCA in patients serum.
- These findings indicate the interaction between ANCA and the myeloperoxidases on the surface of the neutrophils. This lead to oxidative burst and end up with production of oxygen radicals causing glomerular injury.
- Tumor Necrosis Factor (TNF) also plays a role in neutrophils degranulation and free radicals production.
- TNF production during infections and inflammatory diseases in vivo may prime neutrophils in ANCA-positive patients to facilitate neutrophilic activation and subsequent pro-inflammatory cascade of RPGN disease.
- Example of diseases: polyangiitis with granulomatosis and polyarteritis nodosa.
- Type I anti-GBM glomerulonephritis:[3][4][5]
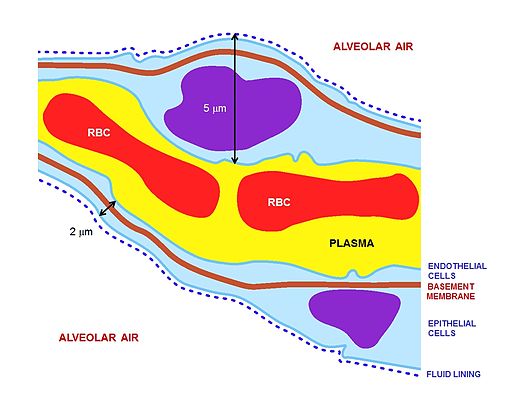
- The cause of renal injury is due to anti-glomerular basement membrane antibodies ability to bind and activate complement system and proteases, resulting in an interruption between the filtration barrier and the Bowman’s capsule.
- The interruption of the Bowman's capsule and filtration barrier, induces crescent shaped antigen-antibody complex formation in the renal corpuscles, invoking proteinuria and activating T cells (CD4+ and CD8+), macrophages, and neutrophils.[9][10]
- While the majority of patients with pauci-immune RPGN indeed have elevated levels of ANCA, the remaining 20% of patients with the same disease do not. Interestingly, 30% of patients in remission continue to have elevated levels of ANCA. Both these problematic findings raise the question of the actual importance of ANCA in the pathogenesis of RPGN.[11] A novel hypothesis currently suggests that RPGN is in fact a podocytopathy, defined as an intrinsic disease of the podocytes that normally maintains glomerular capillary membranes.[12] As such, it is thought that the CXCR4 and VHL-HIF pathway target gene expression in renal biopsies, based on experimental studies on mice.[13]
Microscopic pathology
{{#ev:youtube|CqSyj4cVZPE}}
References
- ↑ 1.0 1.1 Falk RJ, Terrell RS, Charles LA, Jennette JC (1990). "Anti-neutrophil cytoplasmic autoantibodies induce neutrophils to degranulate and produce oxygen radicals in vitro". Proc Natl Acad Sci U S A. 87 (11): 4115–9. PMC 54058. PMID 2161532.
- ↑ Short AK, Esnault VL, Lockwood CM (1995). "Anti-neutrophil cytoplasm antibodies and anti-glomerular basement membrane antibodies: two coexisting distinct autoreactivities detectable in patients with rapidly progressive glomerulonephritis". Am J Kidney Dis. 26 (3): 439–45. PMID 7544065.
- ↑ Ramaswami A, Kandaswamy T, Rajendran T, Aung H, Jacob CK, Zinna HS; et al. (2008). "Goodpasture's syndrome with positive C-ANCA and normal renal function: a case report". J Med Case Rep. 2: 223. doi:10.1186/1752-1947-2-223. PMC 2475522. PMID 18590526.
- ↑ Lewis EJ, Cavallo T, Harrington JT, Cotran RS (1971). "An immunopathologic study of rapidly progressive glomerulonephritis in the adult". Hum Pathol. 2 (2): 185–208. PMID 4937848.
- ↑ Cunningham RJ, Gilfoil M, Cavallo T, Brouhard BH, Travis LB, Berger M; et al. (1980). "Rapidly progressive glomerulonephritis in children: a report of thirteen cases and a review of the literature". Pediatr Res. 14 (2): 128–32. doi:10.1203/00006450-198002000-00012. PMID 7360526.
- ↑ Davies DJ, Moran JE, Niall JF, Ryan GB (1982). "Segmental necrotising glomerulonephritis with antineutrophil antibody: possible arbovirus aetiology?". Br Med J (Clin Res Ed). 285 (6342): 606. PMC 1499415. PMID 6297657.
- ↑ Klebanoff SJ, Vadas MA, Harlan JM, Sparks LH, Gamble JR, Agosti JM; et al. (1986). "Stimulation of neutrophils by tumor necrosis factor". J Immunol. 136 (11): 4220–5. PMID 3009619.
- ↑ Gallin JI, Fletcher MP, Seligmann BE, Hoffstein S, Cehrs K, Mounessa N (1982). "Human neutrophil-specific granule deficiency: a model to assess the role of neutrophil-specific granules in the evolution of the inflammatory response". Blood. 59 (6): 1317–29. PMID 7044447.
- ↑ Hudson BG, Tryggvason K, Sundaramoorthy M, Neilson EG (June 2003). "Alport's syndrome, Goodpasture's syndrome, and type IV collagen". N. Engl. J. Med. 348 (25): 2543–56. doi:10.1056/NEJMra022296. PMID 12815141.
- ↑ Cui Z, Zhao J, Jia XY, Zhu SN, Zhao MH (April 2011). "Clinical features and outcomes of anti-glomerular basement membrane disease in older patients". Am. J. Kidney Dis. 57 (4): 575–82. doi:10.1053/j.ajkd.2010.09.022. PMID 21168945.
- ↑ Hedger N, Stevens J, Drey N, Walker S, Roderick P (2000). "Incidence and outcome of pauci-immune rapidly progressive glomerulonephritis in Wessex, UK: a 10-year retrospective study". Nephrol Dial Transplant. 15 (10): 1593–9. PMID 11007827.
- ↑ Yoshimoto K, Yokoyama H, Wada T, Furuichi K, Sakai N, Iwata Y; et al. (2004). "Pathologic findings of initial biopsies reflect the outcomes of membranous nephropathy". Kidney Int. 65 (1): 148–53. doi:10.1111/j.1523-1755.2004.00403.x. PMID 14675045.
- ↑ Ding M, Cui S, Li C, Jothy S, Haase V, Steer BM; et al. (2006). "Loss of the tumor suppressor Vhlh leads to upregulation of Cxcr4 and rapidly progressive glomerulonephritis in mice". Nat Med. 12 (9): 1081–7. doi:10.1038/nm1460. PMID 16906157.