Rapidly progressive glomerulonephritis pathophysiology: Difference between revisions
No edit summary |
|||
| (12 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
{{Rapidly progressive glomerulonephritis}} | {{Rapidly progressive glomerulonephritis}} | ||
{{CMG}} | .{{CMG}} {{AE}} {{JSS}} {{SAH}} | ||
==Overview== | |||
Rapidly progressive glomerulonephritis is a disease of the kidney in which the [[renal function]] deteriorates in a few days. Atleast 50% reduction in [[Glomerular filtration rate|GFR]] occurs in RPGN in a few days to weeks. RPGN occurs from severe and fast damage to the [[GBM]] which results in [[Crescent Rising|crescent]] formation, the main pathological finding in RPGN. Injury can occur by anti [[GBM]] antibodies-type I RPGN, [[Immune complex]]- type II RPGN or pauci immune RPGN(ANCAs)-type III RPGN. Crescents are present in the [[Bowman's capsule|Bowmans space]]. Light, immunofluoresnce and electron microscopy are used to diagnose RPGN. | |||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 15: | Line 17: | ||
=== Pathogenesis === | === Pathogenesis === | ||
* | * Rapidly progressive glomerulonephritis is a disease of the kidney in which the [[renal function]] deteriorates in a few days<ref name="pmid3287904">{{cite journal| author=Couser WG| title=Rapidly progressive glomerulonephritis: classification, pathogenetic mechanisms, and therapy. | journal=Am J Kidney Dis | year= 1988 | volume= 11 | issue= 6 | pages= 449-64 | pmid=3287904 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3287904 }} </ref><ref name="pmid9507491">{{cite journal| author=Couser WG| title=Pathogenesis of glomerular damage in glomerulonephritis. | journal=Nephrol Dial Transplant | year= 1998 | volume= 13 Suppl 1 | issue= | pages= 10-5 | pmid=9507491 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9507491 }} </ref>. | ||
* Atleast 50% reduction in [[Glomerular filtration rate|GFR]] occurs in RPGN in a few days to weeks. | |||
* RPGN occurs from severe and fast damage to the [[GBM]] which results in [[Crescent Rising|crescent]] formation, the main pathological finding in RPGN. | |||
* The injury to [[GBM]] can be caused by multiple factors. | |||
* [[Crescent Rising|Crescent]] formation is the major pathological finding. | |||
* In some cases crescents might be absent. | |||
====== Cresent formation ====== | |||
* Crescents are defined as 2 or more layers of proliferating cells in the [[Bowman's capsule|Bowman's space.]]<ref name="pmid9507491">{{cite journal| author=Couser WG| title=Pathogenesis of glomerular damage in glomerulonephritis. | journal=Nephrol Dial Transplant | year= 1998 | volume= 13 Suppl 1 | issue= | pages= 10-5 | pmid=9507491 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9507491 }} </ref><ref name="pmid7205449">{{cite journal| author=Roy S, Murphy WM, Arant BS| title=Poststreptococcal crescenteric glomerulonephritis in children: comparison of quintuple therapy versus supportive care. | journal=J Pediatr | year= 1981 | volume= 98 | issue= 3 | pages= 403-10 | pmid=7205449 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7205449 }} </ref><ref name="pmid8959617">{{cite journal| author=Atkins RC, Nikolic-Paterson DJ, Song Q, Lan HY| title=Modulators of crescentic glomerulonephritis. | journal=J Am Soc Nephrol | year= 1996 | volume= 7 | issue= 11 | pages= 2271-8 | pmid=8959617 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8959617 }} </ref> | |||
* The crescents are made up of [[Epithelium|epithelial cells]] and macrophages which undergo [[fibrosis]]<ref name="pmid16105041">{{cite journal| author=Bariéty J, Bruneval P, Meyrier A, Mandet C, Hill G, Jacquot C| title=Podocyte involvement in human immune crescentic glomerulonephritis. | journal=Kidney Int | year= 2005 | volume= 68 | issue= 3 | pages= 1109-19 | pmid=16105041 | doi=10.1111/j.1523-1755.2005.00503.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16105041 }} </ref><ref name="pmid16155400">{{cite journal| author=Tipping PG, Timoshanko J| title=Contributions of intrinsic renal cells to crescentic glomerulonephritis. | journal=Nephron Exp Nephrol | year= 2005 | volume= 101 | issue= 4 | pages= e173-8 | pmid=16155400 | doi=10.1159/000088165 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16155400 }} </ref>. | |||
* Crescents are formed after a severe injury to the [[glomerulus]]. | |||
* Injury to the glomerulus causes leakage of cells(epithelial[[Macrophages|, macrophages]], [[Coagulation|coagulation proteins]] and [[Fibroblast|fibroblasts]]) and [[Cytokine|cytokines]]([[Interleukin 12|IL-12]], [[Tumor necrosis factor-alpha|TNF-alpha]]) into the [[Bowman's capsule|Bowmans space]]. | |||
* The presence of cytokines and coagulation proteins initiates [[fibrosis]] around the epithelial cells. | |||
* The fibrosis blocks the [[glomerulus]] and [[Glomerular filtration|filteration]] is hindered. | |||
* This results in [[Renal insufficiency|renal failure]]. | |||
====== Glomerular injury ====== | |||
* Injury to the glomerulus is the initiating factor for crescent formation. | |||
* Injury can occur by the following. | |||
# Anti [[GBM]] antibodies-Type I RPGN | |||
* These are [[Autoantibody|autoantibodie]]<nowiki/>s that cross react with [[Type-IV collagen|type IV collagen]] of the [[GBM]]. | |||
* These can be produced due to genetic causes such as in [[Goodpasture syndrome]] or they can be produced after viral [[Upper respiratory tract infection|URTI]] or cigarette smoking. | |||
* These autoantibodies react with the GBM resulting in [[Immunoglobulin G|IgG]] deposition over the GBM. | |||
* The IgG activates [[T helper cell|helper T cells]] that attract the [[Inflammation|inflammatory]] mediators to the GBM damaging the glomeruli<ref name="pmid9218836">{{cite journal| author=Huang XR, Tipping PG, Apostolopoulos J, Oettinger C, D'Souza M, Milton G et al.| title=Mechanisms of T cell-induced glomerular injury in anti-glomerular basement membrane (GBM) glomerulonephritis in rats. | journal=Clin Exp Immunol | year= 1997 | volume= 109 | issue= 1 | pages= 134-42 | pmid=9218836 | doi= | pmc=1904710 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9218836 }} </ref>. | |||
* This damage causes leakage of cells and inflammatory mediators resulting in crescent formation. | |||
* The anti GBM antibodies can affect the lungs as well as in [[Goodpasture syndrome]] resulting in glomerular [[necrosis]] and pulmonary [[Bleeding|haemorrhages]]. | |||
2. [[Immune complex]]- Type II RPGN | |||
* Immune complexes are formed in certain infections, [[Connective tissue disease|connective tissue diseases]], side effects of some drugs and in some [[Myeloproliferative neoplasm|myeloproliferative]] disorders<ref name="pmid17164315">{{cite journal| author=Izzedine H, Camous L, Deray G| title=New insight on crescentic glomerulonephritis. | journal=Nephrol Dial Transplant | year= 2007 | volume= 22 | issue= 5 | pages= 1480-1 | pmid=17164315 | doi=10.1093/ndt/gfl742 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17164315 }} </ref>. | |||
* These immune complexes are deposited over the GBM. | |||
* The immune complexes activate the [[complement]] system which sets off the inflammatory process. | |||
* The complement cascade is activated, attracting [[Inflammation|inflammatory]] cells and mediators to the GBM. | |||
* The serum levels of [[C3-convertase|c3]] and [[C4A|c4]] fall down and is an indicator of immune complex mediated glomerular injury. | |||
* This damages the glomeruli and causes leakage of cells and inflammatory mediators resulting in crescent formation. | |||
** Examples include: | |||
** Postinfectious ([[Staphylococcus aureus|staphylococci]]/[[Streptococcus|streptococci]]) | |||
** [[Connective tissue disease|Connective tissue disorders]] | |||
** [[Lupus nephritis]] | |||
** [[Henoch-Schönlein purpura|Henoch-Schönlein purpural]]) | |||
** [[IgA nephropathy|Immunoglobulin A nephropathy]]<ref name="pmid25018935">{{cite journal| author=| title=Chapter 10: Immunoglobulin A nephropathy. | journal=Kidney Int Suppl (2011) | year= 2012 | volume= 2 | issue= 2 | pages= 209-217 | pmid=25018935 | doi=10.1038/kisup.2012.23 | pmc=4089745 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25018935 }} </ref> | |||
** Mixed [[cryoglobulinemia]] | |||
** [[Membranoproliferative glomerulonephritis]] | |||
3. Pauci immune RPGN-Type III RPGN | |||
* No circulating [[Immune complex|immune complexes]] or [[antibodies]]. | |||
* Glomerular damage is caused by circulating [[Antinuclear antibodies|ANCAs]](anti nuclear cytoplasmic antibodies) or it can be idiopathic(non ANCA). | |||
* ANCAs cause glomerular damage by releasing lytic enzymes from white blood cells such as [[Neutrophil|neutrophils]]<ref name="pmid8909258">{{cite journal| author=Heeringa P, Brouwer E, Klok PA, Huitema MG, van den Born J, Weening JJ et al.| title=Autoantibodies to myeloperoxidase aggravate mild anti-glomerular-basement-membrane-mediated glomerular injury in the rat. | journal=Am J Pathol | year= 1996 | volume= 149 | issue= 5 | pages= 1695-706 | pmid=8909258 | doi= | pmc=1865281 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8909258 }} </ref><ref name="pmid15960143">{{cite journal| author=Yang G, Tang Z, Chen Y, Zeng C, Chen H, Liu Z et al.| title=Antineutrophil cytoplasmic antibodies (ANCA) in Chinese patients with anti-GBM crescentic glomerulonephritis. | journal=Clin Nephrol | year= 2005 | volume= 63 | issue= 6 | pages= 423-8 | pmid=15960143 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15960143 }} </ref><ref name="pmid16825335">{{cite journal| author=de Lind van Wijngaarden RA, Hauer HA, Wolterbeek R, Jayne DR, Gaskin G, Rasmussen N et al.| title=Clinical and histologic determinants of renal outcome in ANCA-associated vasculitis: A prospective analysis of 100 patients with severe renal involvement. | journal=J Am Soc Nephrol | year= 2006 | volume= 17 | issue= 8 | pages= 2264-74 | pmid=16825335 | doi=10.1681/ASN.2005080870 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16825335 }} </ref><ref name="pmid21160463">{{cite journal| author=Bomback AS, Appel GB, Radhakrishnan J, Shirazian S, Herlitz LC, Stokes B et al.| title=ANCA-associated glomerulonephritis in the very elderly. | journal=Kidney Int | year= 2011 | volume= 79 | issue= 7 | pages= 757-64 | pmid=21160463 | doi=10.1038/ki.2010.489 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21160463 }} </ref>. | |||
* These lytic enzymes damage the GBM and cause leakage of circulating cells and initiate crescent formationin the Bowmans space. | |||
* ANCAs are associated with systemic [[Vasculitis|vasculitis.]]<ref name="pmid17215440">{{cite journal| author=Chen M, Yu F, Wang SX, Zou WZ, Zhao MH, Wang HY| title=Antineutrophil cytoplasmic autoantibody-negative Pauci-immune crescentic glomerulonephritis. | journal=J Am Soc Nephrol | year= 2007 | volume= 18 | issue= 2 | pages= 599-605 | pmid=17215440 | doi=10.1681/ASN.2006091021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17215440 }} </ref> | |||
* Examples include | |||
** [[Granulomatosis with polyangiitis]] (Wegener granulomatosis) | |||
** [[Microscopic polyangiitis]] (MPA) | |||
** Renal-limited necrotizing crescentic glomerulonephritis (NCGN) | |||
** [[Langerhans cell histiocytosis|Eosinophilic granulomatosis]] with polyangiitis (EGPA; Churg-Strauss syndrome) | |||
** Drugs- [[hydralazine]], [[allopurinol]] and [[rifampin]]. | |||
==Associated Conditions== | |||
Consitions associated with membranous glomerulonephritis include:<ref name="pmid10495797">{{cite journal |vauthors=Wasserstein AG |title=Membranous glomerulonephritis |journal=J. Am. Soc. Nephrol. |volume=8 |issue=4 |pages=664–74 |date=April 1997 |pmid=10495797 |doi= |url=}}</ref> | |||
*[[Hepatitis B/History & Symptoms|Hepatitis B]] | |||
*[[Hepatitis C]] | |||
*Congenital [[Syphilis]] | |||
*[[SLE|Systemic Lupus Erythematosis]] | |||
*Malignancy | |||
**[[Lung]] | |||
**[[Breast]] | |||
**[[Colon]] | |||
**[[Stomach]] | |||
**[[Kidney]] | |||
**[[Leukemia]] | |||
**[[Lymphomas]] ([[Hodgkin]]’s and [[non-Hodgkin]]’s) | |||
== Gross pathology == | |||
* The kidneys appear to be having having [[Bleeding|haemorrhages]] and [[Necrosis|necrosed]] tissue. | |||
* Pulmonary haemorrhages may also be present in [[Goodpasture syndrome]] and type III RPGN. | |||
* Type III RPGN may present with [[Petechia|petechiae]], [[Rash|rashes]] and purpuras. | |||
== Microscopic pathology == | == Microscopic pathology == | ||
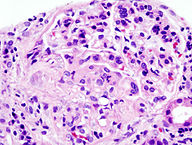
=== Histopathology === | |||
* [[Glomerular disease|Glomerular inflammation]] with signs of necrosis are present<ref name="pmid20616173">{{cite journal| author=Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K et al.| title=Histopathologic classification of ANCA-associated glomerulonephritis. | journal=J Am Soc Nephrol | year= 2010 | volume= 21 | issue= 10 | pages= 1628-36 | pmid=20616173 | doi=10.1681/ASN.2010050477 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20616173 }} </ref><ref name="pmid3392885">{{cite journal| author=Bonsib SM| title=Glomerular basement membrane necrosis and crescent organization. | journal=Kidney Int | year= 1988 | volume= 33 | issue= 5 | pages= 966-74 | pmid=3392885 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3392885 }} </ref>. | |||
* .Glomerular caplillary wall rupture and damage to GBM. | |||
* Crescents are present in the [[Bowman's capsule|Bowmans space]]. | |||
* Crescents are formed by proliferating epithelial cells and [[Monocyte|monocytes]] | |||
* [[Fibroblast|Fibroblasts]] migrate to the Bowman’s space and synthesize [[collagen]]. | |||
* When cellular components are mixed with collagen the lesion is called [[Crescent Rising|fibroepithelial crescent]]. | |||
* Renal vessels can show transmural [[vasculitis]], with necrosis and [[lymphocyte]] infiltrates. | |||
* [[Tubular]] necrosis may also be present. | |||
* Interstitial [[Granuloma|granulomas]] in the glomeruli indicate [[Granulomatosis with polyangiitis|Wegener’s granulomatosis]]. | |||
[[File:192px-Crescentic glomerulonephritis (1).jpg|200px|center|thumb| Microscopic findings of RPGN Source:By Nephron - Own work<ref> https://commons.wikimedia.org/w/index.php?curid=17591464 </ref>]] | |||
=== Immunoflourescence === | |||
* In type I RPGN- diffuse and linear deposition of [[Immunoglobulin G|IgG]] along the [[GBM]]. | |||
* In ttype II RPGN- diffuse and irregular deposition of IgG and C3 in the [[Mesangial cell|mesangial]] matrix. | |||
* In type III RPGN- no finding. | |||
=== Electron microscopy === | |||
* In type I and type III, no electron dense deposits are seen. | |||
* In type II RPGN, subepithelial electron dense deposits indiacting the presence of [[Immune complex|immune complexes]] are seen. | |||
{{#ev:youtube|CqSyj4cVZPE} | == Genetics == | ||
People with [[Human leukocyte antigen|HLA]] DP1,DQ and DRB4 are more susceptible to develop RPGN<ref name="pmid15652778">{{cite journal| author=Jagiello P, Gross WL, Epplen JT| title=Complex genetics of Wegener granulomatosis. | journal=Autoimmun Rev | year= 2005 | volume= 4 | issue= 1 | pages= 42-7 | pmid=15652778 | doi=10.1016/j.autrev.2004.06.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15652778 }} </ref>. | |||
{{#ev:youtube|CqSyj4cVZPE}} | |||
==References== | ==References== | ||
Latest revision as of 18:43, 31 July 2018
|
Rapidly progressive glomerulonephritis Microchapters |
|
Differentiating Rapidly progressive glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Rapidly progressive glomerulonephritis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Rapidly progressive glomerulonephritis pathophysiology |
|
FDA on Rapidly progressive glomerulonephritis pathophysiology |
|
CDC on Rapidly progressive glomerulonephritis pathophysiology |
|
Rapidly progressive glomerulonephritis pathophysiology in the news |
|
Blogs on Rapidly progressive glomerulonephritis pathophysiology |
|
Directions to Hospitals Treating Rapidly progressive glomerulonephritis |
|
Risk calculators and risk factors for Rapidly progressive glomerulonephritis pathophysiology |
.Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Jogeet Singh Sekhon, M.D. [2] Syed Ahsan Hussain, M.D.[3]
Overview
Rapidly progressive glomerulonephritis is a disease of the kidney in which the renal function deteriorates in a few days. Atleast 50% reduction in GFR occurs in RPGN in a few days to weeks. RPGN occurs from severe and fast damage to the GBM which results in crescent formation, the main pathological finding in RPGN. Injury can occur by anti GBM antibodies-type I RPGN, Immune complex- type II RPGN or pauci immune RPGN(ANCAs)-type III RPGN. Crescents are present in the Bowmans space. Light, immunofluoresnce and electron microscopy are used to diagnose RPGN.
Pathophysiology
Anatomy
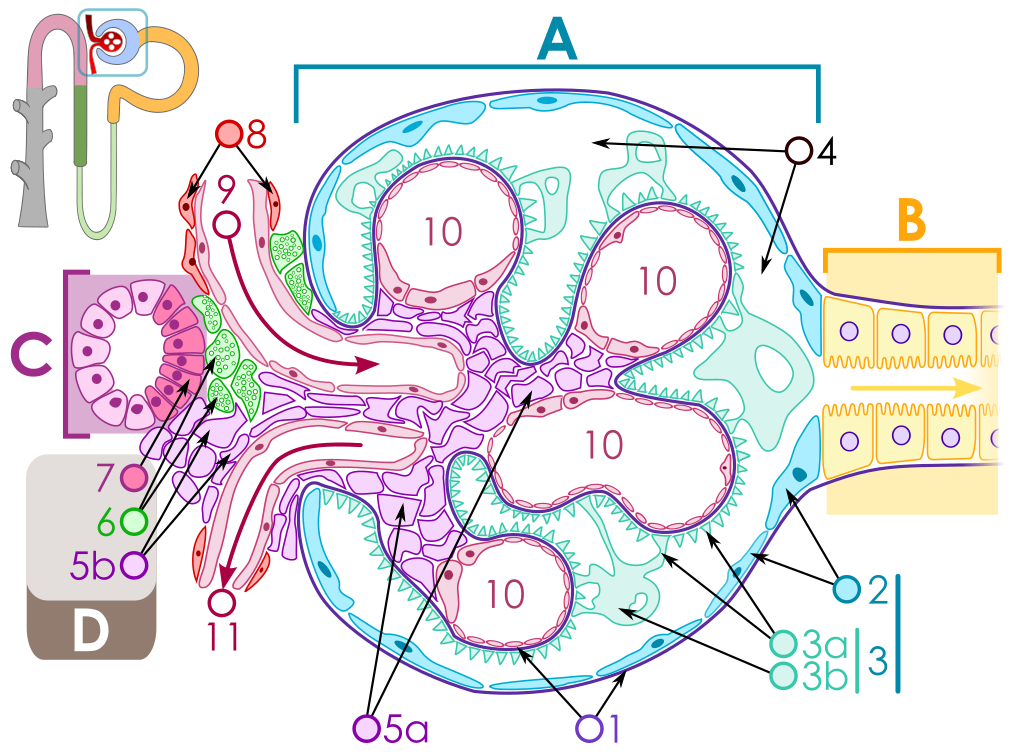
The key for the renal corpuscle figure is: A – Renal corpuscle, B – Proximal tubule, C – Distal convoluted tubule, D – Juxtaglomerular apparatus, 1. Basement membrane (Basal lamina), 2. Bowman's capsule – parietal layer, 3. Bowman's capsule – visceral layer, 3a. Pedicels (Foot processes from podocytes), 3b. Podocyte, 4. Bowman's space (urinary space), 5a. Mesangium – Intraglomerular cell, 5b. Mesangium – Extraglomerular cell, 6. Granular cells (Juxtaglomerular cells), 7. Macula densa, 8. Myocytes (smooth muscle), 9. Afferent arteriole, 10. Glomerulus Capillaries, 11. Efferent arteriole.
Pathogenesis
- Rapidly progressive glomerulonephritis is a disease of the kidney in which the renal function deteriorates in a few days[1][2].
- Atleast 50% reduction in GFR occurs in RPGN in a few days to weeks.
- RPGN occurs from severe and fast damage to the GBM which results in crescent formation, the main pathological finding in RPGN.
- The injury to GBM can be caused by multiple factors.
- Crescent formation is the major pathological finding.
- In some cases crescents might be absent.
Cresent formation
- Crescents are defined as 2 or more layers of proliferating cells in the Bowman's space.[2][3][4]
- The crescents are made up of epithelial cells and macrophages which undergo fibrosis[5][6].
- Crescents are formed after a severe injury to the glomerulus.
- Injury to the glomerulus causes leakage of cells(epithelial, macrophages, coagulation proteins and fibroblasts) and cytokines(IL-12, TNF-alpha) into the Bowmans space.
- The presence of cytokines and coagulation proteins initiates fibrosis around the epithelial cells.
- The fibrosis blocks the glomerulus and filteration is hindered.
- This results in renal failure.
Glomerular injury
- Injury to the glomerulus is the initiating factor for crescent formation.
- Injury can occur by the following.
- Anti GBM antibodies-Type I RPGN
- These are autoantibodies that cross react with type IV collagen of the GBM.
- These can be produced due to genetic causes such as in Goodpasture syndrome or they can be produced after viral URTI or cigarette smoking.
- These autoantibodies react with the GBM resulting in IgG deposition over the GBM.
- The IgG activates helper T cells that attract the inflammatory mediators to the GBM damaging the glomeruli[7].
- This damage causes leakage of cells and inflammatory mediators resulting in crescent formation.
- The anti GBM antibodies can affect the lungs as well as in Goodpasture syndrome resulting in glomerular necrosis and pulmonary haemorrhages.
2. Immune complex- Type II RPGN
- Immune complexes are formed in certain infections, connective tissue diseases, side effects of some drugs and in some myeloproliferative disorders[8].
- These immune complexes are deposited over the GBM.
- The immune complexes activate the complement system which sets off the inflammatory process.
- The complement cascade is activated, attracting inflammatory cells and mediators to the GBM.
- The serum levels of c3 and c4 fall down and is an indicator of immune complex mediated glomerular injury.
- This damages the glomeruli and causes leakage of cells and inflammatory mediators resulting in crescent formation.
- Examples include:
- Postinfectious (staphylococci/streptococci)
- Connective tissue disorders
- Lupus nephritis
- Henoch-Schönlein purpural)
- Immunoglobulin A nephropathy[9]
- Mixed cryoglobulinemia
- Membranoproliferative glomerulonephritis
3. Pauci immune RPGN-Type III RPGN
- No circulating immune complexes or antibodies.
- Glomerular damage is caused by circulating ANCAs(anti nuclear cytoplasmic antibodies) or it can be idiopathic(non ANCA).
- ANCAs cause glomerular damage by releasing lytic enzymes from white blood cells such as neutrophils[10][11][12][13].
- These lytic enzymes damage the GBM and cause leakage of circulating cells and initiate crescent formationin the Bowmans space.
- ANCAs are associated with systemic vasculitis.[14]
- Examples include
- Granulomatosis with polyangiitis (Wegener granulomatosis)
- Microscopic polyangiitis (MPA)
- Renal-limited necrotizing crescentic glomerulonephritis (NCGN)
- Eosinophilic granulomatosis with polyangiitis (EGPA; Churg-Strauss syndrome)
- Drugs- hydralazine, allopurinol and rifampin.
Associated Conditions
Consitions associated with membranous glomerulonephritis include:[15]
- Hepatitis B
- Hepatitis C
- Congenital Syphilis
- Systemic Lupus Erythematosis
- Malignancy
Gross pathology
- The kidneys appear to be having having haemorrhages and necrosed tissue.
- Pulmonary haemorrhages may also be present in Goodpasture syndrome and type III RPGN.
- Type III RPGN may present with petechiae, rashes and purpuras.
Microscopic pathology
Histopathology
- Glomerular inflammation with signs of necrosis are present[16][17].
- .Glomerular caplillary wall rupture and damage to GBM.
- Crescents are present in the Bowmans space.
- Crescents are formed by proliferating epithelial cells and monocytes
- Fibroblasts migrate to the Bowman’s space and synthesize collagen.
- When cellular components are mixed with collagen the lesion is called fibroepithelial crescent.
- Renal vessels can show transmural vasculitis, with necrosis and lymphocyte infiltrates.
- Tubular necrosis may also be present.
- Interstitial granulomas in the glomeruli indicate Wegener’s granulomatosis.
Immunoflourescence
- In type I RPGN- diffuse and linear deposition of IgG along the GBM.
- In ttype II RPGN- diffuse and irregular deposition of IgG and C3 in the mesangial matrix.
- In type III RPGN- no finding.
Electron microscopy
- In type I and type III, no electron dense deposits are seen.
- In type II RPGN, subepithelial electron dense deposits indiacting the presence of immune complexes are seen.
Genetics
People with HLA DP1,DQ and DRB4 are more susceptible to develop RPGN[19]. {{#ev:youtube|CqSyj4cVZPE}}
References
- ↑ Couser WG (1988). "Rapidly progressive glomerulonephritis: classification, pathogenetic mechanisms, and therapy". Am J Kidney Dis. 11 (6): 449–64. PMID 3287904.
- ↑ 2.0 2.1 Couser WG (1998). "Pathogenesis of glomerular damage in glomerulonephritis". Nephrol Dial Transplant. 13 Suppl 1: 10–5. PMID 9507491.
- ↑ Roy S, Murphy WM, Arant BS (1981). "Poststreptococcal crescenteric glomerulonephritis in children: comparison of quintuple therapy versus supportive care". J Pediatr. 98 (3): 403–10. PMID 7205449.
- ↑ Atkins RC, Nikolic-Paterson DJ, Song Q, Lan HY (1996). "Modulators of crescentic glomerulonephritis". J Am Soc Nephrol. 7 (11): 2271–8. PMID 8959617.
- ↑ Bariéty J, Bruneval P, Meyrier A, Mandet C, Hill G, Jacquot C (2005). "Podocyte involvement in human immune crescentic glomerulonephritis". Kidney Int. 68 (3): 1109–19. doi:10.1111/j.1523-1755.2005.00503.x. PMID 16105041.
- ↑ Tipping PG, Timoshanko J (2005). "Contributions of intrinsic renal cells to crescentic glomerulonephritis". Nephron Exp Nephrol. 101 (4): e173–8. doi:10.1159/000088165. PMID 16155400.
- ↑ Huang XR, Tipping PG, Apostolopoulos J, Oettinger C, D'Souza M, Milton G; et al. (1997). "Mechanisms of T cell-induced glomerular injury in anti-glomerular basement membrane (GBM) glomerulonephritis in rats". Clin Exp Immunol. 109 (1): 134–42. PMC 1904710. PMID 9218836.
- ↑ Izzedine H, Camous L, Deray G (2007). "New insight on crescentic glomerulonephritis". Nephrol Dial Transplant. 22 (5): 1480–1. doi:10.1093/ndt/gfl742. PMID 17164315.
- ↑ "Chapter 10: Immunoglobulin A nephropathy". Kidney Int Suppl (2011). 2 (2): 209–217. 2012. doi:10.1038/kisup.2012.23. PMC 4089745. PMID 25018935.
- ↑ Heeringa P, Brouwer E, Klok PA, Huitema MG, van den Born J, Weening JJ; et al. (1996). "Autoantibodies to myeloperoxidase aggravate mild anti-glomerular-basement-membrane-mediated glomerular injury in the rat". Am J Pathol. 149 (5): 1695–706. PMC 1865281. PMID 8909258.
- ↑ Yang G, Tang Z, Chen Y, Zeng C, Chen H, Liu Z; et al. (2005). "Antineutrophil cytoplasmic antibodies (ANCA) in Chinese patients with anti-GBM crescentic glomerulonephritis". Clin Nephrol. 63 (6): 423–8. PMID 15960143.
- ↑ de Lind van Wijngaarden RA, Hauer HA, Wolterbeek R, Jayne DR, Gaskin G, Rasmussen N; et al. (2006). "Clinical and histologic determinants of renal outcome in ANCA-associated vasculitis: A prospective analysis of 100 patients with severe renal involvement". J Am Soc Nephrol. 17 (8): 2264–74. doi:10.1681/ASN.2005080870. PMID 16825335.
- ↑ Bomback AS, Appel GB, Radhakrishnan J, Shirazian S, Herlitz LC, Stokes B; et al. (2011). "ANCA-associated glomerulonephritis in the very elderly". Kidney Int. 79 (7): 757–64. doi:10.1038/ki.2010.489. PMID 21160463.
- ↑ Chen M, Yu F, Wang SX, Zou WZ, Zhao MH, Wang HY (2007). "Antineutrophil cytoplasmic autoantibody-negative Pauci-immune crescentic glomerulonephritis". J Am Soc Nephrol. 18 (2): 599–605. doi:10.1681/ASN.2006091021. PMID 17215440.
- ↑ Wasserstein AG (April 1997). "Membranous glomerulonephritis". J. Am. Soc. Nephrol. 8 (4): 664–74. PMID 10495797.
- ↑ Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K; et al. (2010). "Histopathologic classification of ANCA-associated glomerulonephritis". J Am Soc Nephrol. 21 (10): 1628–36. doi:10.1681/ASN.2010050477. PMID 20616173.
- ↑ Bonsib SM (1988). "Glomerular basement membrane necrosis and crescent organization". Kidney Int. 33 (5): 966–74. PMID 3392885.
- ↑ https://commons.wikimedia.org/w/index.php?curid=17591464
- ↑ Jagiello P, Gross WL, Epplen JT (2005). "Complex genetics of Wegener granulomatosis". Autoimmun Rev. 4 (1): 42–7. doi:10.1016/j.autrev.2004.06.003. PMID 15652778.