Pulsus alternans: Difference between revisions
No edit summary |
No edit summary |
||
| Line 147: | Line 147: | ||
[[Category:Mature chapter]] | [[Category:Mature chapter]] | ||
[[Category:Signs and symptoms]] | [[Category:Signs and symptoms]] | ||
[[Category:Physical examination]] | |||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
{{Circulatory system pathology}} | {{Circulatory system pathology}} | ||
{{WH}} | {{WH}} | ||
Revision as of 06:35, 20 November 2013
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Varun Kumar, M.B.B.S.
Overview
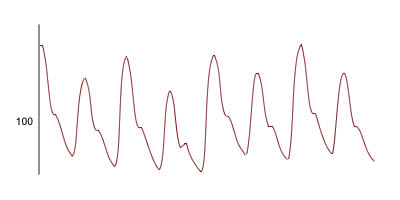
Pulsus alternans is a physical finding with arterial pulse waveform showing alternating strong and weak beats.[1] It is almost always indicative of left ventricular systolic impairment, and carries a poor prognosis.
Pathophysiology
In left ventricular dysfunction, the ejection fraction will decrease significantly, causing reduction in stroke volume, hence causing a increase in end-diastolic volume. There may initially be a tachycardia as a compensatory mechanism to try to keep the cardiac output constant. As a result, during the next cycle of systolic phase, the myocardial muscle will be stretched more than usual and as a result cause an increase in myocardial contraction, related to the Frank–Starling physiology of the heart. This in turn results in a stronger systolic pulse.
Causes
Life Threatening Causes
Common Causes
Causes by Organ System
Causes in Alphabetical Order
Related Chapters
References
- ↑ Euler D (1999) Cardiac alternans: mechanisms and pathophysiological significance. Cardiovascular Research. Vol. 42. P. 583-590. PMID 10533597
- ↑ Nayak NC, Chitale AR (2013). "Indian childhood cirrhosis (ICC) & ICC-like diseases: the changing scenario of facts versus notions". Indian J Med Res. 137 (6): 1029–42. PMC 3734708. PMID 23852284.
- ↑ Schultze AE, Roth RA (1998). "Chronic pulmonary hypertension--the monocrotaline model and involvement of the hemostatic system". J Toxicol Environ Health B Crit Rev. 1 (4): 271–346. doi:10.1080/10937409809524557. PMID 9776954.
- ↑ Kashyap S, Mohapatra PR (2013). "Pulmonary alveolar microlithiasis". Lung India. 30 (2): 143–7. doi:10.4103/0970-2113.110424. PMC 3669555. PMID 23741096.