Schistosoma mansoni
| Schistosoma mansoni | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
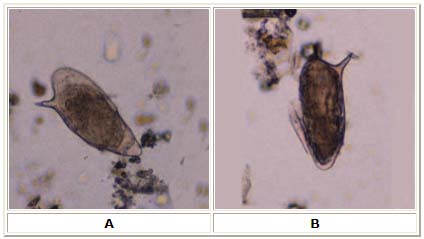
| Schistosomes encopula Schistosomes encopula
| ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Schistosoma mansoni Sambon, 1907 |
For the WikiDoc page on Schistosomiasis, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Schistosoma mansoni is a significant parasite of humans. Of the trematodes, schistosomes are atypical in that the adult stages have two sexes (dioecious) and are located in blood vessels of the definitive host. Most other trematodes are hermaphroditic and are found in the intestinal tract, or organs such as the liver. The lifecycle of schistosomes includes two hosts: a definitive host (i.e. man) where the parasite undergoes sexual reproduction, and a single intermediate snail host where there are a number of asexual reproductive stages. Schistoma mansoni is one of the major agents of schistosomiasis and is named after Sir Patrick Manson who first identified it.
Morphology of adult helminths
Schistosomes, contrary to other trematodes, are long and slim worms. The male S. mansoni is approximately 1 cm long (0.6 to 1.4 cm) and is 0.11 cm wide. It is white and it has a funnel-shaped oral sucker at its anterior end followed by a second pediculated sucker. The external part of the worm is composed of seven layers and is continually renewed the outer layer is continually shedding. The tegument has a large quantity of small tubercules. The suckers have small thorns in their inner part as well as in the buttons around it. The male genital apparatus is composed of 6 to 9 testicular masses, situated dorsal. There is one deferent canal beginning at each testicle, which is connected to a single deferent that dilates into a reservatory the seminal vesicle located at the beginning of the gynacophoric canal. The copula happens through the coaptation of the male and female genital orifices.[1]
The female has a cilindric body, longer and thinner than the male (1.2 to 1.6 cm long by 0.016 cm wide). The female parasite is darker and it looks gray. The darker color is due to the presence of a pigment (hemozoin) in its digestive tube. This pigment is derived from the digestion of blood. The ovary is elongated, slightly lobulated and is located on the anterior half of the body. A short oviduct conducts to the ootype which continues with the uterine tube. In this tube it is possible to find 1 to 2 eggs (rarely 3 to 4) but only 1 egg is observed in the ootype at any one time. The genital pore opens ventrally. The posterior two thirds of the body contain the vittelogenic glands and their winding canal, which unites with the oviduct a little bit before it reaches the ootype.
In only one sex the digestive tube begins at the anterior extremity of the worm, at the bottom of the oral sucker. The digestive tube is composed of an esophagus which divides in two branches (right and left) and that reunite in a single cecum. There isn't any anus.
Epidemiology
Schistosoma mansoni is a parasite that is found in Africa, Madagascar, parts of South America (such as Venezuela and Brazil), Puerto Rico and the West Indies. Among human parasitic diseases, schistosomiasis (sometimes called bilharziasis) ranks second behind malaria in terms of socio-economic and public health importance in tropical and subtropical areas. The disease is endemic in 76 developing countries, infecting more than 200 million people in rural agricultural and peri-urban areas, and placing more than 600 million people at risk.[2]
Of the infected patients, 20 million suffer severe consequences from the disease and 120 million are symptomatic. Some estimate that there are approximately 20.000 deaths related to schistosomiasis yearly. In many areas, schistosomiasis infects a large proportion of under-14 children. An estimated 500-600 million people worldwide are at risk from the disease.
Life Cycle
After the eggs of the human-dwelling parasite are emitted in the feces and into the water, the ripe miracidium hatches out of the egg. The hatching happens in response to temperature, light and dilution of feces with water. The miracidium searches for a suitable fresh water snail (Biomphalaria glabrata, B. straminea or B. tenagophila) to act as an intermediate host and penetrates it. Following this, the parasite develops via a so-called mother-sporocyst and daughter-sporocyst generation to the cercaria. The purpose of the growth in the snail is the numerical multiplication of the parasite. From a single miracidium results a few thousand cercaria, every one of which is capable of infecting man. The cercaria emerge from the snail during day light and they propel themselves in water with the aid of their bifurcated tail, actively seeking out their final host. When they recognise human skin, they penetrate it within a very short time. This occurs in three stages, an initial attachment to the skin, followed by the cercaria creeping over the skin searching for a suitable penetration site, often a hair follicle, and finally penetration of the skin into the epidermis using proteolytic secretions from the cercarial post-acetabular, then pre-acetabular glands. On penetration, the head of the cercaria transforms into an endoparasitic larva, the schistosomule. Each schistosomule spends a few days in the skin and then enters the circulation starting at the dermal lymphatics and venules. The schistosomule migrates to the lungs (5-7 days post penetration) and then moves via circulation through the left side of the heart to the hepatoportal circulation (>15 days) where, if they meet a partner of the opposite sex, develop into sexually mature adults and migrate to the mesenteric veins.[3]
Male schistosomes undergo normal maturation and morphological development in the presence or absence of a female, although behavioural, physiological and antigenic differences between males from single, as opposed to bisex infections, have been reported. On the other hand, female schistosomes do not mature without a male. Females schistosomes from single sex infections are underdeveloped and exhibit immature reproductive system. Although the maturation of the female worm seems to be dependent on the presence of the mature male, the stimuli for female growth and for reproductive development seem to be independent from each other.
The adult female worm resides within the adult male worm gynacophoric canal, which is a modification of the ventral surface of the male forming a groove. The paired worms move against the flow of blood to their final niche in the mesenteric circulation where they begin egg production (>32 days). The S. mansoni parasites are found predominantly in the small inferior mesenteric blood vessels surrounding the large intestine and caecal region. Each female lays approximately 300 eggs per day (one egg every 4.8 min), which are deposited on the endothelial lining of the venous capillary walls.[4] Most of the body mass of female schistosomes is devoted to the reproductive system. The female converts the equivalent of almost her own body dry weight into eggs each day. The eggs move into the lumen of the intestines and are released into the environment with the feces.
Genome
Schistosoma mansoni has 8 pairs of chromosomes (2n = 16), 7 autosomal pairs and 1 sex pair. The female schistosome is heterogametic or ZW and the male is homogametic or ZZ. Sex is determined in the zygote by a chromossomal mechanism. The Schistosoma genome is approximately 270 MB with a GC content of 34%, 4-8% highly repetitive sequence, 32-36% middle repetitive sequence and 60% single copy sequence. Numerous highly or moderately repetitive elements have been identified and their frequency in genomic sequence data also suggests at least 30% repetitive DNA. Schistosoma possesses 7 pairs of autosomes and one pair of sex chromosomes (female = ZW, male = ZZ). Chromosomes range in size from 18 to 73 MB and can be distinguished by size, shape and C banding. There are estimated to be 15-20,000 expressed genes. [5]
In June 2003, a ~5x whole genome shotgun sequencing project was initiated at the Sanger Institute. Together with the shotgun data being generated by TIGR, an ~8x coverage of the genome will be obtained, assembled and annotated. [6] Also in 2003, 163000 ESTs (expressed sequence tags) were generated (by a consortium headed by the University of São Paulo) from six selected developmental stages of this parasite, resulting in 31000 assembled sequences and an estimated 92% of the 14000 gene complement. [7]
Pathology
Schistosome eggs, which may become lodged within the hosts tissues, are the major cause of pathology in schistosomiasis. Part of the deposited eggs reach the outside environment by passing through the wall of the intestine; the rest are swept into the circulation and filter out in the periportal tracts of the liver resulting in periportal fibrosis. Onset of egg laying in humans is sometimes associated with an onset of fever (Katayama fever). This "Acute Schistosomiasis" is not however as important as the chronic forms of the disease. For S. mansoni and S. japonicum these are "Intestinal" and "Hepatic Schistosomiasis", associated with formation of granulomas around trapped eggs lodged in the intestinal wall or in the liver respectively. The hepatic form of the disease is the most important, granulomas here giving rise to fibrosis of the liver and hepatosplenomegaly in severe cases. Symptoms and signs depend on the number and location of eggs trapped in the tissues. Initially, the inflammatory reaction is readily reversible. In the latter stages of the disease, the pathology is associated with collagen deposition and fibrosis resulting in organ damage that may be only partially reversible.
Granuloma formation is initiated by antigens secreted by the miracidium through microscopic pores within the rigid egg shell and there is strong evidence that the vigorous granulomatous response, rather than the direct action of a parasite egg antigen(s), is responsible for the pathologic tissue manifestations in schistosomiasis [8]. The granulomas formed around the eggs impair blood flow in the liver and consequently induce portal hypertension. With time, collateral circulation is formed and the eggs disseminate into lungs, where they cause more granulomas, pulmonary arteritis and later cor pulmonale. A contributory factor to portal hypertension is Symmers' fibrosis which develops around branches of the portal veins. This fibrosis occur only many years afters the infection and apparently is caused in part by soluble egg antigens and various immune cells which react to them.
Symptoms
Many individuals do not experience symptoms. If present, it usually takes four to six weeks for symptoms to appear. The first symptom of the disease may be a general ill feeling. Within twelve hours of infection, an individual may complain of a tingling sensation or light rash, commonly referred to as "swimmer's itch," due to irritation at the point of entrance. The rash that may develop can mimic scabies and other types of rashes. Other symptoms can occur two to ten weeks later and can include fever, aching, cough, diarrhea, or gland enlargement. These symptoms can also be related to avian schistosomiasis which does not cause any further symptoms in humans.
Katayama fever
Another primary condition, called Katayama fever, may also develop from infection with these worms, and it can be very difficult to recognize. Symptoms include fever, lethargy, the eruption of pale temporary bumps associated with severe itching (urticarial) rash, liver and spleen enlargement, and bronchospasm.
Intestinal schistosomiasis
In intestinal schistosomiasis, eggs become lodged in the intestinal wall and cause an immune system reaction called a granulomatous reaction. This immune response can lead to obstruction of the colon and blood loss. The infected individual may have what appears to be a potbelly. Eggs can also become lodged in the liver, leading to high blood pressure through the liver, enlarged spleen, the build-up of fluid in the abdomen ascites), and potentially life-threatening dilations or swollen areas in the esophagus or gastrointestinal tract that can tear and bleed profusely (esophageal varices). Rarely, the central nervous system may be affected. Individuals with chronic active schistosomiasis may not complain of typical symptoms.
Diagnosis and treatment
Diagnosis of infection is confirmed by the identification of eggs in stools. Eggs of Schistosoma mansoni are approximately 140 x 60 µm in size and have a lateral spine. The diagnosis is improved by the utilization of the Kato-Katz technique (a semi-quantitative stool examination technique). Other methods which can be used are enzyme linked immunosorbent assay (ELISA), circumoval precipitation test (COPT) and alkaline phosphatase immunoassay (APIA).[9]
Currently there are two drugs available, Praziquantel and Oxamniquine, for the treatment of [10] schistosomiasis. They are considered equivalent in relation to efficacy and safety. Due to its lower cost per treatment, Praziquantel is generally considered the first option for treatment. The recommended dose is: Praziquantel, 60mg/kg of body weight for children up to 15 years old, and 50mg/kg of body weight for adults; Oxamniquine, 15mg/kg for adults, and 20mg/kg for children up to 15 years old. Both drugs are administered as a single dose treatment. The treatment objective is to cure the disease and to prevent the evolution of infected patients to the chronic form of the disease. All confirmed cases should be treated.
References
- ↑ Rey, Luíz (1991). Parasitologia. Rio de Janeiro, RJ: Editora Guanabara Koogan S.A. pp. 351&ndash, 62. ISBN 85-277-0189-8.
- ↑ Oliveira, G. (2004). "Genome and Genomics of Schistosomes". Can. J. Zool. 82: 375–90. doi:10.1139/Z03-220. Unknown parameter
|coauthors=ignored (help) - ↑ "DPDx - Schistosomiasis". CDC. Retrieved 2007-14-06. Check date values in:
|accessdate=(help) - ↑ Loverde, P.T. (1991). "Schistosome female reproductive development". Parasitol. Today. 7 (11): 303–308. Unknown parameter
|coauthors=ignored (help) - ↑ "Schistosoma mansoni Genome Project". Sanger Institute. Retrieved 2007-14-06. Check date values in:
|accessdate=(help) - ↑ "Schistosoma mansoni Genome Project". The Institute for Genomic Research. Retrieved 2007-14-06. Check date values in:
|accessdate=(help) - ↑ "Schistosoma mansoni EST Genome Project". University of São Paulo. Retrieved 2007-14-06. Check date values in:
|accessdate=(help) - ↑ Boros, D.L. (1989). "Immunopathology of Schistosoma mansoni infection" (pdf). Clin Microbiol Rev. 2 (3): 250–69. PMID: 2504481. Retrieved 14/06/2007. Check date values in:
|accessdate=(help) - ↑ "Clinical Aspects". University of Tsukuba School of Medicine. Retrieved 2007-14-06. Check date values in:
|accessdate=(help) - ↑ "eMedicine - Schistosomiasis". eMedicine. Retrieved 2007-14-06. Check date values in:
|accessdate=(help)
Further reading
- Adel A. F. Mahmoud. Schistosomiasis. World Scientific Publishing Company, Imperial College Press, London, 2001. (ISBN 978-1860941467)