Pleural effusion: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
}} | }} | ||
{{SI}} | {{SI}} | ||
'''For the WikiPatient page for this topic, click [[Pleural effusion (patient information)|here]]''' | |||
{{CMG}} | {{CMG}} | ||
__NOTOC__ | __NOTOC__ | ||
Revision as of 14:42, 12 August 2011
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Pleural effusion |
|
Articles |
|---|
|
Most recent articles on Pleural effusion Most cited articles on Pleural effusion |
|
Media |
|
Powerpoint slides on Pleural effusion |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pleural effusion at Clinical Trials.gov Trial results on Pleural effusion Clinical Trials on Pleural effusion at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pleural effusion NICE Guidance on Pleural effusion
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pleural effusion Discussion groups on Pleural effusion Patient Handouts on Pleural effusion Directions to Hospitals Treating Pleural effusion Risk calculators and risk factors for Pleural effusion
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pleural effusion |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For the WikiPatient page for this topic, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Related Key Words and Synonyms: Pleural fluid
Pleural effusion is excess fluid that accumulates in the pleural cavity, the fluid-filled space that surrounds the lungs.
Four types of fluids can accumulate in the pleural space:
- Serous fluid (hydrothorax)
- Blood (hemothorax)
- Chyle (chylothorax)
- Pus (pyothorax or empyema)
Pathophysiology & Etiology
Healthy individuals have less than 15 ml of fluid in each pleural space. Normally, fluid enters the pleural space from the capillaries in the parietal pleura, from interstitial spaces of the lung via the visceral pleura, or from the peritoneal cavity through small holes in the diaphragm. This fluid is normally removed by lymphatics in the visceral pleura, which have the capacity to absorb 20 times more fluid than is normally formed. When this capacity is overwhelmed, either through excess formation or decreased lymphatic absorption, a pleural effusion develops.
- Increase entry of fluid versus decreased exit of fluid.
- Lymphatics have a large reserve capacity to deal with excess fluid.
Increased Fluid Entry
- Increased permeability
- Increase in fluid conductance or protein permeability.
- Increased microvascular pressure
- Usually increased venous outflow pressure. Arterial pressures usually not transmitted due to capillary resistance. Thought to be lung interstitial fluid when hydrostatic pressure.
- Decreased pleural pressure
- i.e. Significant atalectasis, reduces pressures around nearby vessels.
- Decreased plasma oncotic pressure
- Hypoalbuminemia alone not usually enough but can lower threshold for other factors.
- Increased permeability
Decreased Fluid Exit
- Reflects a reduction in lymphatic function.
- Much of how is speculative.
- There are intrinsic and extrinsic factors.
- Intrinsic
- Prevent ability of lymphatic vessels to transport fluid- products of inflammation, endocrine problems (hypothyroidism), direct injury (chemotherapy, radiotherapy), infiltration with cancer.
- Extrinsic
- Limitation of respiratory motion (diaphragm paralysis, lung collapse), compression of lymphatics (pleural fibrosis, pleural granulomas), blockage (pleural malignancy), increased systemic venous pressure (only acutely because chronically lymphatics can adapt), decreased liquid availability (ie after pneumothorax liquid contacts fewer lymphatic openings)
- Common postoperative in patients undergoing cardiac surgical procedures
- Predominantly left-sided: suggests underlying pericarditis is a causative factor.
- Majority are small and not serious.
- Pathogenesis may relate to immunologic cause
- Respond to steroids and prolonged latent period from injury to onset
History and Symptoms
- Only symptomatic pleural effusions or effusions larger than 50% of hemithorax require thoracentesis or chest tube drainage.
- Most resolve spontaneously.
- Postcardiac injury syndrome (PCIS)
- A general term for fever and pleuropericardial disease days or months after cardiac injury (myocardial infarction or surgery).
- Typically present two to three weeks post op.
- Chest pain
- Pericardial rub
- Fever
- Leukocytosis
- Elevated erythrocyte sedimentation rate (ESR)
- Variable combinations of pulmonary effusions and infiltrates.
Diagnosis
Pleural effusion is usually diagnosed on the basis of the history of your family and physical exam, and confirmed by chest x-ray. Chest films acquired in the lateral decubitus position (with the patient lying on their side) are more sensitive, and can pick up as little as 50 ml of fluid. At least 300 ml of fluid must be present before upright chest films can pick up signs of pleural effusion (e.g., blunted costophrenic angles). Once accumulated fluid is more than 500 ml, there are usually detectable clinical signs in the patient, such as decreased movement of the chest on the affected side, dullness to percussion over the fluid, diminished breath sounds on the affected side, decreased vocal fremitus and resonance, pleural friction rub, and egophony.
Once a pleural effusion is diagnosed, the cause must be determined. Pleural fluid is drawn out of the pleural space in a process called thoracentesis. A needle is inserted through the back of the chest wall into the pleural space. The fluid may then be evaluated for the following:
- Chemical composition including protein, lactate dehydrogenase (LDH), albumin, amylase, pH and glucose
- Gram stain and culture to identify possible bacterial infections
- Cell count and differential
- Cytology to identify cancer cells, but may also identify some infective organisms
- Other tests as suggested by the clinical situation - lipids, fungal culture, viral culture, specific immunoglobulins
Electrolyte and Biomarker Studies
- Definite diagnoses can be made by specific analyses of fluid.
- Culture
- Cytology
- Lupus erythematosus (LE) cells
- Antinuclear antibody (ANA) >1 (systemic lupus erythematosus)
- Amylase and severe acidosis (esophageal rupture)
- KOH prep
- Triglycerides (>110mg/dL = chylothorax)
- Hematocrit (pleural fluid to blood >0.5)
- Creatinine (urinothorax)
- Protein <1g/dL
- Glucose 300 to 400 (peritoneal dialysis).
- Look at the fluid- milky, bloody, clear.
- Transudate
- Imbalance between hydrostatic and oncotic pressure in chest.
- May also be movement of fluid from abdominal cavity or retroperitoneal space.
- Exudates:
- Result from pleural and lung inflammation (resulting in a capillary protein leak) or impaired lymphatic drainage of pleural space (so slow removal of protein from pleural space).
- Can also result from movement of fluid form peritoneal space.
- If at least one of the following 3 is present, the fluid is virtually always and exudate; in none is present, the fluid is virtually always a transudate:
- Pleural fluid protein/serum protein ratio >0.5
- Fluid/serum lactic dehydrogenase (LDH) ratio >0.6
- Fluid LDH greater than 2/3 the upper limits of normal of the serum LDH
- Some tidbits
- Tuberculosis (TB) effusions virtually always have a protein above 4.0 g/dL.
- Pleural fluid protein in the 7 to 8 g/dL range, consider Waldenstrom’s macroglobulinemia and mult myeloma.
- LDH avove 1000 usually found in empyema, rheumatoid pleurisy and sometime malignancy.
- Pleural fluid in Pneumocystis carinii pneumonia (PCP) has fluid/serum LDH greater than 1 and fluid/serum protein ratio less than 0.5.
- Glucose
- Lower then 60mg/dL or fluid/serum ratio < 0.5 not seen in transudates and limits exudates to the following
- Rheumatoid pleurisy
- Parapneumonic effusion or empyema
- Malignant effusion
- TB
- Lupus pleuritis
- Esophageal rupture.
- Lower then 60mg/dL or fluid/serum ratio < 0.5 not seen in transudates and limits exudates to the following
- pH
- Less than 7.30 with nrl blood pH found with same diagnosis as low glucose.
- Nrl pleural fluid is around 7.6 due to a bicarbonate gradient between pleural fluid and blood.
- Amylase
- Greater than the upper limit of normal for serum or a pleural fluid to serum ration >1 narrows an exudate to acute pancreatitis, chronic pancreatic effusion, esophageal rupture or malignancy.
Transudate vs. exudate
The third step in the evaluation of pleural fluid is to determine whether the effusion is a transudate or an exudate. Transudative pleural effusions are caused by systemic factors that alter the balance of the formation and absorption of pleural fluid (e.g., left ventricular failure, pulmonary embolism, and cirrhosis), while exudative pleural effusions are caused by alterations in local factors that influence the formation and absorption of pleural fluid (e.g., bacterial pneumonia, cancer, and viral infection).
Transudative and exudative pleural effusions are differentiated by comparing chemistries in the pleural fluid to those in the blood. According to a meta-analysis, exudative pleural effusions meet at least one of the following criteria [1]:
- Pleural fluid protein >2.9 g/dL (29 g/L)
- Pleural fluid cholesterol >45 mg/dL (1.16 mmol/L)
- Pleural fluid LDH >60 percent of upper limit for serum
Previously criteria proposed by Light for an exudative effusion are met if at least one of the following exists (Light's criteria) [2]:
- The ratio of pleural fluid protein to serum protein is greater than 0.5
- The ratio of pleural fluid LDH and serum LDH is greater than 0.6
- Pleural fluid LDH is more than two-thirds normal upper limit for serum
Twenty-five percent of patients with transudative pleural effusions are mistakenly identified as having exudative pleural effusions by Light's criteria. Therefore, additional testing is needed if a patient identified as having an exudative pleural effusion appears clinically to have a condition that produces a transudative effusion. In such cases albumin levels in blood and pleural fluid are measured. If the difference between the albumin levels in the blood and the pleural fluid is greater than 1.2 g/dL (12 g/L), it can be assumed that the patient has a transudative pleural effusion.
If the fluid is definitively identified as exudative, additional testing is necessary to determine the local factors causing the exudate.
Exudative pleural effusions
Once identified as exudative, additional evaluation is needed to determine the cause of the excess fluid, and pleural fluid amylase, glucose, and cell counts are obtained. The fluid is also sent for Gram staining and culture, and, if suspicious for tuberculosis, examination for TB markers (adenosine deaminase > 45 IU/L, interferon gamma > 140 pg/mL, or positive polymerase chain reaction (PCR) for tuberculous DNA).
Pleural fluid amylase is elevated in cases of esophageal rupture, pancreatic pleural effusion, or cancer. Glucose is decreased with cancer, bacterial infections, or rheumatoid pleuritis. If cancer is suspected, the pleural fluid is sent for cytology. If cytology is negative, and cancer is still suspected, either a thoracoscopy, or needle biopsy of the pleura may be performed.
Chest X-Ray
-
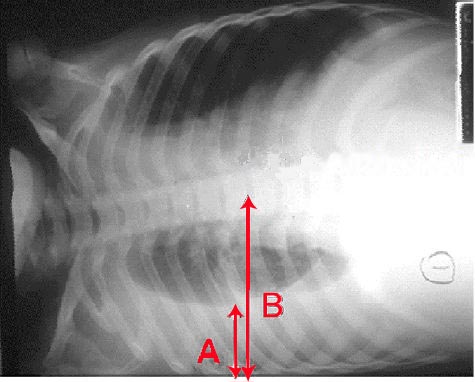
Pleural effusion Chest x-ray of a pleural effusion. The arrow A shows fluid layering in the right pleural cavity. The B arrow shows the normal width of the lung in the cavity
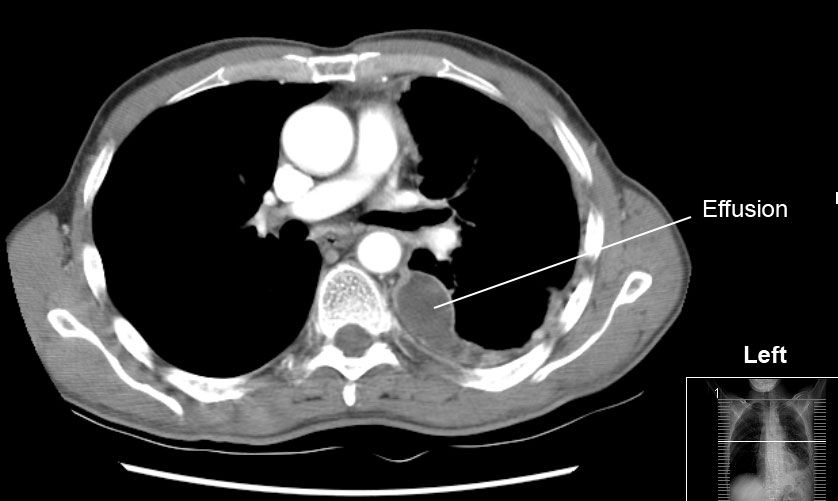
Multi Sliced CT
Causes
The most common causes of transudative pleural effusions in the United States are left ventricular failure, pulmonary embolism, and cirrhosis (causing hepatic hydrothorax), while the most common causes of exudative pleural effusions are bacterial pneumonia, cancer (with lung cancer, breast cancer, and lymphoma causing approximately 75% of all malignant pleural effusions), viral infection, and pulmonary embolism. Although pulmonary embolism can produce either transudative or exudative pleural effusions, the latter is more common.
Other causes of pleural effusion include, tuberculosis (though pleural fluid smears are rarely positive for AFB, this is the most common cause of pleural effusion in some developing countries), autoimmune disease such as systemic lupus erythematosus, bleeding (often due to chest trauma), chylothorax (most commonly caused by trauma), and accidental infusion of fluids. Less common causes include, esophageal rupture or pancreatic disease, intraabdominal abscess, rheumatoid arthritis, asbestos pleural effusion, Meig's syndrome (ascites and pleural effusion due to a benign ovarian tumor), and ovarian hyperstimulation syndrome.
Pleural effusions may also occur through medical/surgical interventions, including the use of medications (pleural fluid is usually eosinophilic), coronary artery bypass surgery, abdominal surgery, endoscopic variceal sclerotherapy, radiation therapy, liver or lung transplantation, and intra- or extravascular insertion of central lines.
Treatment
Treatment depends on the underlying cause of the pleural effusion. Therapeutic aspiration may be sufficient; larger effusions may require insertion of an intercostal drain (either pigtail or surgical). Repeated effusions may require chemical (talc, bleomycin, tetracycline/doxycycline) or surgical pleurodesis, in which the two pleural surfaces are attached to each other so that no fluid can accumulate between them.
References
- ↑ Heffner J, Brown L, Barbieri C (1997). "Diagnostic value of tests that discriminate between exudative and transudative pleural effusions. Primary Study Investigators". Chest. 111 (4): 970–80. PMID 9106577.
- ↑ Light R, Macgregor M, Luchsinger P, Ball W (1972). "Pleural effusions: the diagnostic separation of transudates and exudates". Ann Intern Med. 77 (4): 507–13. PMID 4642731.
See also
External links
- Medline Plus Article on Pleural Effusion
- Pleural Effusion Virtual Cancer Centre
Additional Readings
- Light RW (2001). Pleural Diseases (4th ed. ed.). New York: Lippincott Williams & Wilkins. ISBN 0-7817-2777-4
- Light RW (2008). Fauci A, Braunwald E, Kasper DL, Hauser S, Longo D, Jameson JL, Loscalzo J., ed. Disorders of the pleura, mediastinum, diaphragm, and chest wall in Harrison's Principles of Internal Medicine (17th ed. ed.). New York, NY: McGraw-Hill Professional. ISBN 978-0071466332
- Dowdeswell IRG (1998). "Chapter 64: Pleural Diseases". In Stein JH. Internal Medicine (5th ed. ed.). New York: C.V.Mosby. ISBN 0-8151-8698-3