Papilledema
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Papilledema (or papilloedema) is optic disc swelling that is caused by increased intracranial pressure. The swelling is usually bilateral and can occur over a period of hours to weeks. Papilledema occurs in approximately 50% of those with a brain tumour.
Pathophysiology
As the optic nerve sheath is continuous with the subarachnoid space of the brain (and is regarded as an extension of the central nervous system), increased pressure is transmitted through to the optic nerve. The brain itself is relatively spared from pathological consequences of high pressure.
However, the anterior end of the optic nerve stops abruptly at the eye. Hence the pressure is asymmetrical and this causes a pinching and protrusion of the optic nerve at its head.
The fibers of the retinal ganglion cells of the optic disc become engorged and bulge anteriorly. Persistent and extensive optic nerve head swelling, or optic disc edema, can lead to loss of these fibers and permanent visual impairment.
Differential diagnosis of causes of papilledema
Most common
Organ system based
| Cardiovascular | No underlying causes |
| Chemical / poisoning | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | No underlying causes |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal / Ortho | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal / Electrolyte | No underlying causes |
| Rheum / Immune / Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Dental | No underlying causes |
| Miscellaneous | No underlying causes |
In alphabetical order
[1] [2]
- Arachnoid cyst
- Arnold chiari malformation
- Atypical optic neuritis
- Brain cyst
- Brain tumor
- Cavernous sinus thrombosis
- Central retinal vein occlusion
- Cerebral abscess
- Chondroma
- Cisplatin
- Corticosteroids
- Crouzon's disease
- Cushing's syndrome
- Diabetic papillopathy
- Eclampsia
- Epidural hematoma
- Extradural abscess
- Foster Kennedy's syndrome
- Grave's opthalmopathy
- Head trauma
- Hypercapnia
- Hyperparathyroidism
- Hypertensive encephalopathy
- Hypocalcemic tetany
- Idiopathic intracranial hypertension
- Intracranial hemorrhage
- Infectious endocarditis
- Lithium
- Hydrocephalus
- Malignant hypertension
- Meningitis
- Meningoencephalitis
- Neuropappilitis
- Optic disc vasculitis
- Orbital lesions
- Orbital optic nerve tumors
- Osteoma
- Paget's disease
- Papillitis
- Psuedopapilledema
- Sarcoidosis
- Subarachnoid hemorrhage
- Subdural empyema
- Subdural hematoma
- Syphillis
- Systemic lupus erythematosus
- Tetracyclines
- Thyrotoxicosis
- Uveitis
Diagnosis
Checking the eyes for signs of papilledema should be carried out whenever there is a clinical suspicion of raised intracranial pressure. Because of the (rare) possibility of a brain tumor, pseudotumor cerebri or cerebral venous sinus thrombosis, all of which can increase intracranial pressure, this examination has become common for patients suffering from headaches.
Physical Examination
Eyes
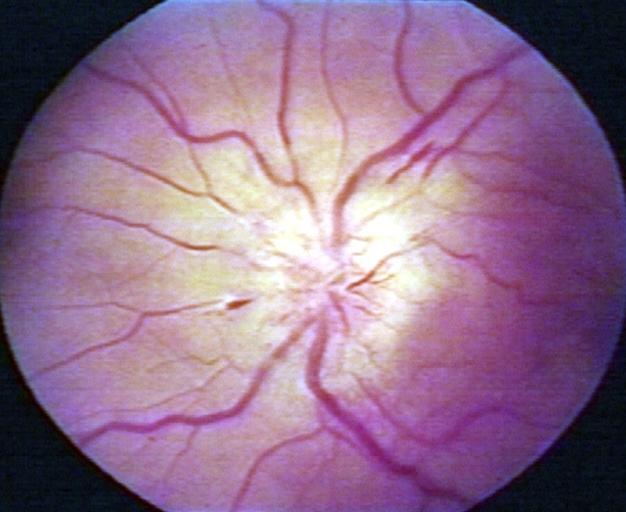
-
Papilledema.
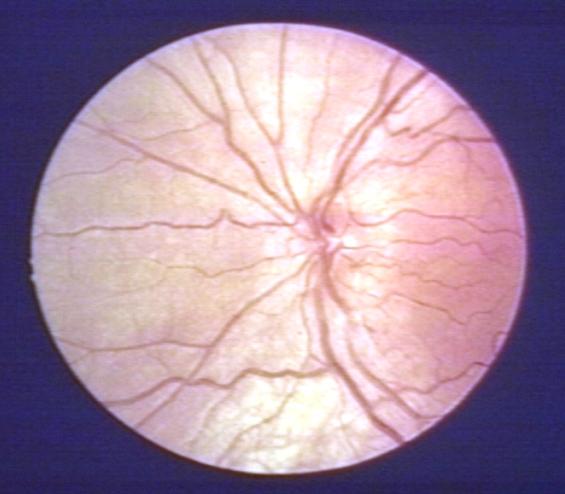
-
Pseudopapilledema.
Presentation
There are 10 hallmarks of papilledema:
- blurring of the disc margins
- filling in of the optic disc cup
- anterior bulging of the nerve head
- edema of the nerve fiber layer
- retinal or choroidal folds
- congestion of retinal veins
- peripapillary hemorrhages
- hyperemia of the optic nerve head
- nerve fiber layer infarcts
- hard exudates of the optic disc