Non-bacterial thrombotic endocarditis pathophysiology: Difference between revisions
Aisha Adigun (talk | contribs) |
Aisha Adigun (talk | contribs) |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 4: | Line 4: | ||
{{CMG}}; {{AE}}{{Aisha}} | {{CMG}}; {{AE}}{{Aisha}} | ||
==Overview== | ==Overview== | ||
Although the exact [[pathogenesis]] of [[non-bacterial thrombotic endocarditis]] is not completely understood, [[Endothelial dysfunction|endothelial injury]] correlated with a [[hypercoagulable state]] has been implicated. Pathogenesis can be sub-sectioned into four factors thought to be involved in instigating NBTE. These include; [[Immune complexes]][[Hypoxia|, Hypoxia]] , [[Hypercoagulability]], and[[Carcinomatosis]]. Conditions associated with nonbacterial thrombotic endocarditis include; [[Malignancies]], [[Systemic autoimmune diseases]] ([[Systemic lupus erythematosus|SLE]] is the most common,[[Hypercoagulable states]], Chronic inflammatory states, [[Heart failure]] with [[Valve dysfunction|valvulopathy]], e.t.c. | |||
[ | |||
[ | |||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 36: | Line 11: | ||
*Although the exact [[pathogenesis]] of [[non-bacterial thrombotic endocarditis]] is not completely understood<ref name="urlNon-bacterial Thrombotic Endocarditis | IntechOpen">{{cite web |url=https://www.intechopen.com/books/infective-endocarditis/non-bacterial-thrombotic-endocarditis |title=Non-bacterial Thrombotic Endocarditis | IntechOpen |format= |work= |accessdate=}}</ref>, [[Endothelial dysfunction|endothelial injury]] correlated with a [[hypercoagulable state]] has been implicated. | *Although the exact [[pathogenesis]] of [[non-bacterial thrombotic endocarditis]] is not completely understood<ref name="urlNon-bacterial Thrombotic Endocarditis | IntechOpen">{{cite web |url=https://www.intechopen.com/books/infective-endocarditis/non-bacterial-thrombotic-endocarditis |title=Non-bacterial Thrombotic Endocarditis | IntechOpen |format= |work= |accessdate=}}</ref>, [[Endothelial dysfunction|endothelial injury]] correlated with a [[hypercoagulable state]] has been implicated. | ||
*The main culprit that has been identified is damage to the [[endothelium]] and consequent exposure of sub[[endothelial]] [[connective tissue]] to [[Platelet|circulating platelets]], platelet deposition and the formation of initial thrombi by the migration of inflammatory mononuclear cells<ref name="pmid27501336">{{cite journal |vauthors=Liu J, Frishman WH |title=Nonbacterial Thrombotic Endocarditis: Pathogenesis, Diagnosis, and Management |journal=Cardiol Rev |volume=24 |issue=5 |pages=244–7 |date=2016 |pmid=27501336 |doi=10.1097/CRD.0000000000000106 |url=}}</ref>. | *The main culprit that has been identified is damage to the [[endothelium]] and consequent exposure of sub[[endothelial]] [[connective tissue]] to [[Platelet|circulating platelets]], platelet deposition and the formation of initial thrombi by the migration of inflammatory mononuclear cells<ref name="pmid27501336">{{cite journal |vauthors=Liu J, Frishman WH |title=Nonbacterial Thrombotic Endocarditis: Pathogenesis, Diagnosis, and Management |journal=Cardiol Rev |volume=24 |issue=5 |pages=244–7 |date=2016 |pmid=27501336 |doi=10.1097/CRD.0000000000000106 |url=}}</ref>. | ||
*Deposited vegetation may be microscopic or large, and may have a wart-like appearance (verrucae)<ref name="urlAn Echocardiographic Study of Valvular Heart Disease Associated with Systemic Lupus Erythematosus | NEJM">{{cite web |url=https://www.nejm.org/doi/full/10.1056/NEJM199611073351903 |title=An Echocardiographic Study of Valvular Heart Disease Associated with Systemic Lupus Erythematosus | NEJM |format= |work= |accessdate=}}</ref>. | |||
*Depositions are more common in left-sided heart valves<ref name="urlNon-infectious aortic and mitral valve vegetations in a patient with eosinophilic granulomatosis with polyangiitis | BMJ Case Reports">{{cite web |url=http://dx.doi.org/10.1136/bcr-2018-225947 |title=Non-infectious aortic and mitral valve vegetations in a patient with eosinophilic granulomatosis with polyangiitis | BMJ Case Reports |format= |work= |accessdate=}}</ref> and do not require prior damage to the valve ( although they NBTE can also arise in preexisting valvular disease)<ref name="urlNONBACTERIAL THROMBOTIC ENDOCARDITIS AS A CAUSE OF CEREBRAL AND MYOCARDIAL INFARCTION">{{cite web |url=https://doi.org/10.1253/jcj.48.1000 |title=NONBACTERIAL THROMBOTIC ENDOCARDITIS AS A CAUSE OF CEREBRAL AND MYOCARDIAL INFARCTION |format= |work= |accessdate=}}</ref>. | |||
*Pathogenesis can be sub-sectioned into four factors thought to be involved in instigating NBTE. These include<ref name="pmid32">{{cite journal |vauthors=Beck ML, Freihaut B, Henry R, Pierce S, Bayer WL, Hendrickson WA, Ward KB, Wolf P, Feller K, Femmer K, Mohn GR |title=A serum haemagglutinating property dependent upon polycarboxyl groups |journal=Br. J. Haematol. |volume=29 |issue=1 |pages=149–56 |date=January 1975 |pmid=32 |doi=10.1111/j.1365-2141.1975.tb01808.x |url=}}</ref>; | *Pathogenesis can be sub-sectioned into four factors thought to be involved in instigating NBTE. These include<ref name="pmid32">{{cite journal |vauthors=Beck ML, Freihaut B, Henry R, Pierce S, Bayer WL, Hendrickson WA, Ward KB, Wolf P, Feller K, Femmer K, Mohn GR |title=A serum haemagglutinating property dependent upon polycarboxyl groups |journal=Br. J. Haematol. |volume=29 |issue=1 |pages=149–56 |date=January 1975 |pmid=32 |doi=10.1111/j.1365-2141.1975.tb01808.x |url=}}</ref>; | ||
#[[Immune complexes]]<ref>Williams R.C.Jr.. Immune complexes in clinical and experimental medicine, 19801st ed. p. 12</ref> | #[[Immune complexes]]<ref>Williams R.C.Jr.. Immune complexes in clinical and experimental medicine, 19801st ed. p. 12</ref> | ||
| Line 43: | Line 20: | ||
====Immune Complexes==== | ====Immune Complexes==== | ||
*Circulating [[immune complexes]] | *Circulating [[immune complexes]] was first identified in the formation of [[Nonbacterial thrombotic endocarditis|NBTE]] by Williams in 1980<ref>Williams R.C.Jr.. Immune complexes in clinical and experimental medicine, 19801st ed. p. 12</ref>. | ||
*Since that time, [[Immunohistochemistry|immunohistochemical techniques]] have been used to identify [[immunoglobulin]] and [[complement]] deposits within vessel walls in the zone of [[neovascularization]] of [[Verrucae|verrucose]] valvular lesions.<ref name="pmid339850">{{cite journal |vauthors=Shapiro RF, Gamble CN, Wiesner KB, Castles JJ, Wolf AW, Hurley EJ, Salel AF |title=Immunopathogenesis of Libman-Sacks endocarditis. Assessment by light and immunofluorescent microscopy in two patients |journal=Ann. Rheum. Dis. |volume=36 |issue=6 |pages=508–16 |date=December 1977 |pmid=339850 |pmc=1000155 |doi=10.1136/ard.36.6.508 |url=}}</ref> | *Since that time, [[Immunohistochemistry|immunohistochemical techniques]] have been used to identify [[immunoglobulin]] and [[complement]] deposits within vessel walls in the zone of [[neovascularization]] of [[Verrucae|verrucose]] valvular lesions.<ref name="pmid339850">{{cite journal |vauthors=Shapiro RF, Gamble CN, Wiesner KB, Castles JJ, Wolf AW, Hurley EJ, Salel AF |title=Immunopathogenesis of Libman-Sacks endocarditis. Assessment by light and immunofluorescent microscopy in two patients |journal=Ann. Rheum. Dis. |volume=36 |issue=6 |pages=508–16 |date=December 1977 |pmid=339850 |pmc=1000155 |doi=10.1136/ard.36.6.508 |url=}}</ref> | ||
*These findings are especially found in patients with [[systemic lupus erythematosus]] (SLE)<ref name="pmid4847246">{{cite journal |vauthors=Nydegger UE, Lambert PH, Gerber H, Miescher PA |title=Circulating immune complexes in the serum in systemic lupus erythematosus and in carriers of hepatitis B antigen. Quantitation by binding to radiolabeled C1q |journal=J. Clin. Invest. |volume=54 |issue=2 |pages=297–309 |date=August 1974 |pmid=4847246 |pmc=301557 |doi=10.1172/JCI107765 |url=}}</ref>. | *These findings are especially found in patients with [[systemic lupus erythematosus]] (SLE)<ref name="pmid4847246">{{cite journal |vauthors=Nydegger UE, Lambert PH, Gerber H, Miescher PA |title=Circulating immune complexes in the serum in systemic lupus erythematosus and in carriers of hepatitis B antigen. Quantitation by binding to radiolabeled C1q |journal=J. Clin. Invest. |volume=54 |issue=2 |pages=297–309 |date=August 1974 |pmid=4847246 |pmc=301557 |doi=10.1172/JCI107765 |url=}}</ref>. | ||
| Line 59: | Line 36: | ||
*The relationship between [[carcinomatosis]] and NBTE has been vastly studied and established<ref>Sanjay Asopa, Anish Patel, Omar A. Khan, Rajan Sharma, Sunil K. Ohri, Non-bacterial thrombotic endocarditis, European Journal of Cardio-Thoracic Surgery, Volume 32, Issue 5, November 2007, Pages 696–701, https://doi.org/10.1016/j.ejcts.2007.07.029</ref>. | *The relationship between [[carcinomatosis]] and NBTE has been vastly studied and established<ref>Sanjay Asopa, Anish Patel, Omar A. Khan, Rajan Sharma, Sunil K. Ohri, Non-bacterial thrombotic endocarditis, European Journal of Cardio-Thoracic Surgery, Volume 32, Issue 5, November 2007, Pages 696–701, https://doi.org/10.1016/j.ejcts.2007.07.029</ref>. | ||
*50% of malignancies associated with NBTEs are [[Adenocarcinoma|adenocarcinomas]] of the [[Adenocarcinoma of the lung|lung]] and [[Ovarian cancer|ovary]]<ref name="pmid15919332">{{cite journal |vauthors=Borowski A, Ghodsizad A, Cohnen M, Gams E |title=Recurrent embolism in the course of marantic endocarditis |journal=Ann. Thorac. Surg. |volume=79 |issue=6 |pages=2145–7 |date=June 2005 |pmid=15919332 |doi=10.1016/j.athoracsur.2003.12.024 |url=}}</ref><ref name="pmid12365726">{{cite journal |vauthors=Suzuki S, Tanaka K, Nogawa S, Umezawa A, Hata J, Fukuuchi Y |title=Expression of interleukin-6 in cerebral neurons and ovarian cancer tissue in Trousseau syndrome |journal=Clin. Neuropathol. |volume=21 |issue=5 |pages=232–5 |date=2002 |pmid=12365726 |doi= |url=}}</ref>. | *50% of malignancies associated with NBTEs are [[Adenocarcinoma|adenocarcinomas]] of the [[Adenocarcinoma of the lung|lung]] and [[Ovarian cancer|ovary]]<ref name="pmid15919332">{{cite journal |vauthors=Borowski A, Ghodsizad A, Cohnen M, Gams E |title=Recurrent embolism in the course of marantic endocarditis |journal=Ann. Thorac. Surg. |volume=79 |issue=6 |pages=2145–7 |date=June 2005 |pmid=15919332 |doi=10.1016/j.athoracsur.2003.12.024 |url=}}</ref><ref name="pmid12365726">{{cite journal |vauthors=Suzuki S, Tanaka K, Nogawa S, Umezawa A, Hata J, Fukuuchi Y |title=Expression of interleukin-6 in cerebral neurons and ovarian cancer tissue in Trousseau syndrome |journal=Clin. Neuropathol. |volume=21 |issue=5 |pages=232–5 |date=2002 |pmid=12365726 |doi= |url=}}</ref>. | ||
*It has been established that [[malignancies]] place patients in a hypercoagulable state which can then predispose them to valvular damage, clot formation, and NBTE<ref name="urlwww.cancertherapyadvisor.com">{{cite web |url=https://www.cancertherapyadvisor.com/home/cancer-topics/general-oncology/nonbacterial-thrombotic-endocarditis-and-malignancy/ |title=www.cancertherapyadvisor.com |format= |work= |accessdate=}}</ref>.<br> | *It has been established that [[malignancies]] place patients in a [[hypercoagulable state]] which can then predispose them to valvular damage, clot formation, and NBTE<ref name="urlwww.cancertherapyadvisor.com">{{cite web |url=https://www.cancertherapyadvisor.com/home/cancer-topics/general-oncology/nonbacterial-thrombotic-endocarditis-and-malignancy/ |title=www.cancertherapyadvisor.com |format= |work= |accessdate=}}</ref>.<br> | ||
*The [[mitral valve]] is most commonly affected in NBTE, followed by the [[aortic valve]] and less frequently, the [[tricuspid valve]]<ref name="pmid32308583">{{cite journal |vauthors=Zakka K, Zakka P, Davarpanah A, Koshkelashvili N, Bilen MA, Owonikoko T, El-Rayes B, Akce M |title=Nonbacterial Thrombotic Endocarditis and Widespread Skin Necrosis in Newly Diagnosed Lung Adenocarcinoma |journal=Case Rep Oncol |volume=13 |issue=1 |pages=239–244 |date=2020 |pmid=32308583 |pmc=7154248 |doi=10.1159/000506453 |url=}}</ref>. | *The [[mitral valve]] is most commonly affected in NBTE, followed by the [[aortic valve]] and less frequently, the [[tricuspid valve]]<ref name="pmid32308583">{{cite journal |vauthors=Zakka K, Zakka P, Davarpanah A, Koshkelashvili N, Bilen MA, Owonikoko T, El-Rayes B, Akce M |title=Nonbacterial Thrombotic Endocarditis and Widespread Skin Necrosis in Newly Diagnosed Lung Adenocarcinoma |journal=Case Rep Oncol |volume=13 |issue=1 |pages=239–244 |date=2020 |pmid=32308583 |pmc=7154248 |doi=10.1159/000506453 |url=}}</ref>. | ||
*The vegetations in | *The vegetations in NTBE are formed from the strands consisting of [[fibrin]], [[Immune complex|immune complexes]], [[neutrophils]], [[lymphocytes]], and [[histiocytes]]<ref name="pmid11761501">{{cite journal |vauthors=Eiken PW, Edwards WD, Tazelaar HD, McBane RD, Zehr KJ |title=Surgical pathology of nonbacterial thrombotic endocarditis in 30 patients, 1985-2000 |journal=Mayo Clin. Proc. |volume=76 |issue=12 |pages=1204–12 |date=December 2001 |pmid=11761501 |doi=10.4065/76.12.1204 |url=}}</ref>. | ||
*As there is some inflammatory reaction at the site of attachment of vegetation, they can easily dislodge, embolize and cause serious infarctions<ref name="pmid24029368">{{cite journal |vauthors=Roldan CA, Sibbitt WL, Qualls CR, Jung RE, Greene ER, Gasparovic CM, Hayek RA, Charlton GA, Crookston K |title=Libman-Sacks endocarditis and embolic cerebrovascular disease |journal=JACC Cardiovasc Imaging |volume=6 |issue=9 |pages=973–83 |date=September 2013 |pmid=24029368 |pmc=3941465 |doi=10.1016/j.jcmg.2013.04.012 |url=}}</ref>. | *As there is some [[Inflammation|inflammatory reaction]] at the site of attachment of [[Vegetation (pathology)|vegetation]], they can easily dislodge, [[Embolism|embolize]] and cause serious [[Infarction|infarctions]]<ref name="pmid24029368">{{cite journal |vauthors=Roldan CA, Sibbitt WL, Qualls CR, Jung RE, Greene ER, Gasparovic CM, Hayek RA, Charlton GA, Crookston K |title=Libman-Sacks endocarditis and embolic cerebrovascular disease |journal=JACC Cardiovasc Imaging |volume=6 |issue=9 |pages=973–83 |date=September 2013 |pmid=24029368 |pmc=3941465 |doi=10.1016/j.jcmg.2013.04.012 |url=}}</ref>. | ||
==Associated Conditions== | ==Associated Conditions== | ||
Conditions associated with | Conditions associated with nonbacterial thrombotic endocarditis include<ref name="urlNon-bacterial Thrombotic Endocarditis | IntechOpen">{{cite web |url=https://www.intechopen.com/books/infective-endocarditis/non-bacterial-thrombotic-endocarditis |title=Non-bacterial Thrombotic Endocarditis | IntechOpen |format= |work= |accessdate=}}</ref><ref name="urlNonbacterial Thrombotic Endocarditis: Clinicopathologic Study of a Necropsy Series | Revista Española de Cardiología (English Edition)">{{cite web |url=https://www.revespcardiol.org/en-nonbacterial-thrombotic-endocarditis-clinicopathologic-study-articulo-13106392 |title=Nonbacterial Thrombotic Endocarditis: Clinicopathologic Study of a Necropsy Series | Revista Española de Cardiología (English Edition) |format= |work= |accessdate=}}</ref>: | ||
*[[Malignancies]] | |||
*[ | *[[Systemic autoimmune diseases]] ([[Systemic lupus erythematosus|SLE]] is the most common) | ||
*[ | *[[Hypercoagulable states]] | ||
*[ | *Chronic inflammatory states | ||
*[[Heart failure]] with [[Valve dysfunction|valvulopathy]] | |||
==Gross Pathology== | ==Gross Pathology== | ||
*On gross pathology, small (1-5mm) and sterile vegetations that occur on normal cardiac valves, and are composed of platelets and fibrin are characteristic findings in NBTE<ref name="urlCvs ie-csbrp">{{cite web |url=https://www.slideshare.net/csbrprasad/cvs-iecsbrp |title=Cvs ie-csbrp |format= |work= |accessdate=}}</ref>. | *On gross pathology, small (1-5mm) and sterile vegetations that occur on normal cardiac valves, and are composed of platelets and fibrin are characteristic findings in NBTE<ref name="urlCvs ie-csbrp">{{cite web |url=https://www.slideshare.net/csbrprasad/cvs-iecsbrp |title=Cvs ie-csbrp |format= |work= |accessdate=}}</ref>. | ||
==Microscopic Pathology== | ==Microscopic Pathology/Histology== | ||
On microscopic histopathological analysis, [ | *On microscopic histopathological analysis, degenerating platelets interwoven with fibrin strands, granulomatous tissue, and fibrotic foci,<ref name="urlRedirecting">{{cite web |url=https://doi.org/10.1016/S1885-5857(07)60190-X |title=Redirecting |format= |work= |accessdate=}}</ref> are characteristic findings of NBTE. | ||
*The evolution of vegetation in NBTE has been described in three stages; | |||
**[[Stages of human development|Stage]] 1 ([[Active Living|active]] [[verrucae]]); Consists of [[fibrin]] clumps on and within the [[valvular]] leaflet [[tissue]] (focally [[necrotic]]), along with [[plasma cells]] and [[lymphocytes]]. | |||
**[[Stages of human development|Stage]] 2 ([[Combination reaction|Combined]] [[Active Living|active]] and [[Healing|healed]] [[lesions]]); Contains [[fibrous]], [[Vascularity|vascularized]] [[tissue]] adjacent to [[necrotic]] and [[fibrinous]] [[Area|areas]]. | |||
**[[Stages of human development|Stage]] 3 ([[Healing|Healed]] [[lesions]]); Consists of [[dense]], [[fibrous]], and [[Vascularity|vascularized]] [[tissue]]. | |||
{| | |||
| | |||
[[File:Cr534e-g004.jpg|thumb|200px|none|Pathology slide of mitral valve vegetation. Lots of necrosis: 10 cm circumference vegetation. Mitral valve tissue shows focal necrosis. No bacterial or fungal organisms were present. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
[[File:Cr534e-g005.jpg|thumb|200px|none|R lung, high power: emboli and large necrotic infarcted tissue. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
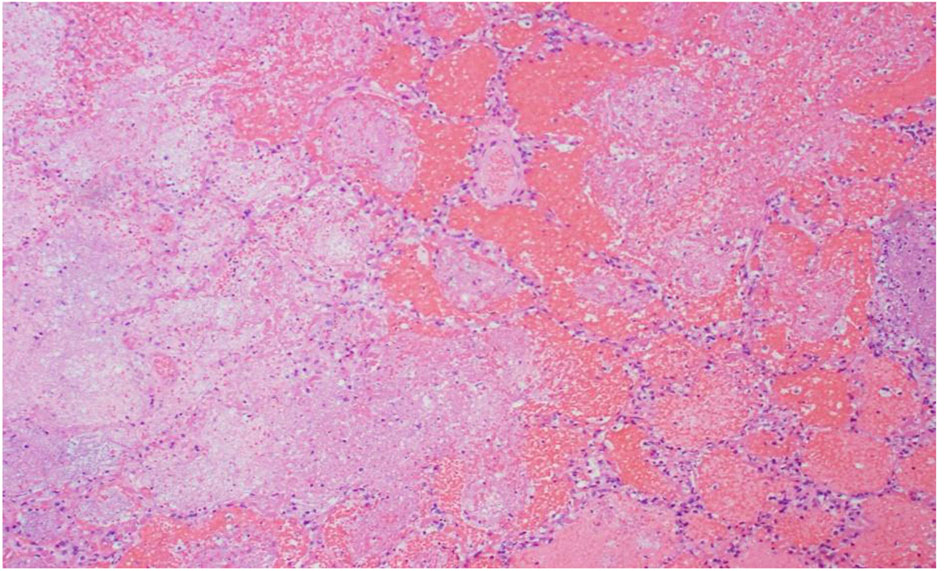
[[File:Cr534e-g006.jpg|thumb|200px|none|Low power of the liver: lots of steatosis and congestion, necrosis. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
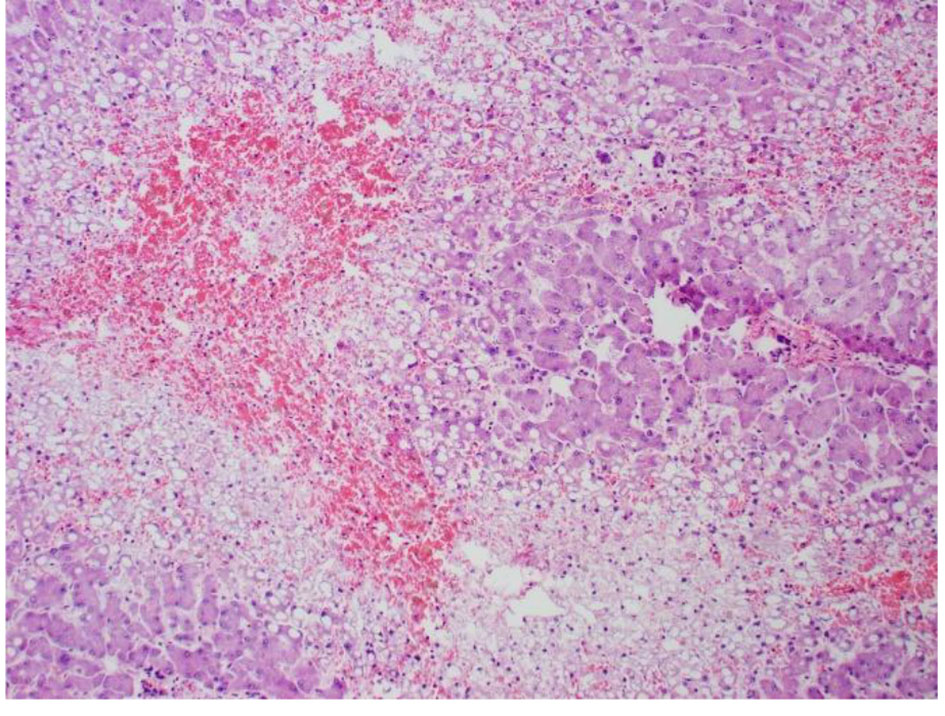
| | |||
[[File:Cr534e-g007.jpg|thumb|200px|none|High power pathology slide of the liver showing lots of steatosis, congestion, and necrosis. [https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
| | |||
[[File:Cr534e-g008.jpg|thumb|200px|none|Low power pathology slide of the lung showing emboli and necrotic tissue.[https://cardiologyres.org/index.php/Cardiologyres/article/view/551/592 Source: Ghulam Murtaza. et al, Department of Internal Medicine, Advocate Christ Medical Center, Oak Lawn, IL, USA]]] | |||
|} | |||
==References== | ==References== | ||
Latest revision as of 15:24, 25 August 2020
|
non-bacterial thrombotic endocarditis |
|
Differentiating non-bacterial thrombotic endocarditis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Non-bacterial thrombotic endocarditis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Non-bacterial thrombotic endocarditis pathophysiology |
|
FDA on Non-bacterial thrombotic endocarditis pathophysiology |
|
CDC on Non-bacterial thrombotic endocarditis pathophysiology |
|
Non-bacterial thrombotic endocarditis pathophysiology in the news |
|
Blogs on Non-bacterial thrombotic endocarditis pathophysiology |
|
Risk calculators and risk factors for Non-bacterial thrombotic endocarditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aisha Adigun, B.Sc., M.D.[2]
Overview
Although the exact pathogenesis of non-bacterial thrombotic endocarditis is not completely understood, endothelial injury correlated with a hypercoagulable state has been implicated. Pathogenesis can be sub-sectioned into four factors thought to be involved in instigating NBTE. These include; Immune complexes, Hypoxia , Hypercoagulability, andCarcinomatosis. Conditions associated with nonbacterial thrombotic endocarditis include; Malignancies, Systemic autoimmune diseases (SLE is the most common,Hypercoagulable states, Chronic inflammatory states, Heart failure with valvulopathy, e.t.c.
Pathophysiology
Pathogenesis
- Although the exact pathogenesis of non-bacterial thrombotic endocarditis is not completely understood[1], endothelial injury correlated with a hypercoagulable state has been implicated.
- The main culprit that has been identified is damage to the endothelium and consequent exposure of subendothelial connective tissue to circulating platelets, platelet deposition and the formation of initial thrombi by the migration of inflammatory mononuclear cells[2].
- Deposited vegetation may be microscopic or large, and may have a wart-like appearance (verrucae)[3].
- Depositions are more common in left-sided heart valves[4] and do not require prior damage to the valve ( although they NBTE can also arise in preexisting valvular disease)[5].
- Pathogenesis can be sub-sectioned into four factors thought to be involved in instigating NBTE. These include[6];
Immune Complexes
- Circulating immune complexes was first identified in the formation of NBTE by Williams in 1980[12].
- Since that time, immunohistochemical techniques have been used to identify immunoglobulin and complement deposits within vessel walls in the zone of neovascularization of verrucose valvular lesions.[13]
- These findings are especially found in patients with systemic lupus erythematosus (SLE)[14].
Hypoxia
- Several studies have associated hypoxia with NBTE[15][16][17].
- These studies were conducted in both human[16][15] and animal[17] models and they found that, increased or persistent exposure to hypoxic insult can lead to an increase in circulating tissue factor.
- Tissue factor has been found to lead to a hypercoagulable state, which may have predisposed the studied patient populations to NBTE[15].
Hypercoagulability
- The association between thrombosis and malignancy was first described by Trousseau in 1866[18].
- In 1956 Robbins and MacDonald[19] hypothesized that valvular degeneration and hypercoagulable state played significant roles in the origin/formation of NBTE.
Carcinomatosis
- The relationship between carcinomatosis and NBTE has been vastly studied and established[20].
- 50% of malignancies associated with NBTEs are adenocarcinomas of the lung and ovary[21][22].
- It has been established that malignancies place patients in a hypercoagulable state which can then predispose them to valvular damage, clot formation, and NBTE[23].
- The mitral valve is most commonly affected in NBTE, followed by the aortic valve and less frequently, the tricuspid valve[24].
- The vegetations in NTBE are formed from the strands consisting of fibrin, immune complexes, neutrophils, lymphocytes, and histiocytes[25].
- As there is some inflammatory reaction at the site of attachment of vegetation, they can easily dislodge, embolize and cause serious infarctions[26].
Associated Conditions
Conditions associated with nonbacterial thrombotic endocarditis include[1][27]:
- Malignancies
- Systemic autoimmune diseases (SLE is the most common)
- Hypercoagulable states
- Chronic inflammatory states
- Heart failure with valvulopathy
Gross Pathology
- On gross pathology, small (1-5mm) and sterile vegetations that occur on normal cardiac valves, and are composed of platelets and fibrin are characteristic findings in NBTE[28].
Microscopic Pathology/Histology
- On microscopic histopathological analysis, degenerating platelets interwoven with fibrin strands, granulomatous tissue, and fibrotic foci,[29] are characteristic findings of NBTE.
- The evolution of vegetation in NBTE has been described in three stages;
- Stage 1 (active verrucae); Consists of fibrin clumps on and within the valvular leaflet tissue (focally necrotic), along with plasma cells and lymphocytes.
- Stage 2 (Combined active and healed lesions); Contains fibrous, vascularized tissue adjacent to necrotic and fibrinous areas.
- Stage 3 (Healed lesions); Consists of dense, fibrous, and vascularized tissue.
References
- ↑ 1.0 1.1 "Non-bacterial Thrombotic Endocarditis | IntechOpen".
- ↑ Liu J, Frishman WH (2016). "Nonbacterial Thrombotic Endocarditis: Pathogenesis, Diagnosis, and Management". Cardiol Rev. 24 (5): 244–7. doi:10.1097/CRD.0000000000000106. PMID 27501336.
- ↑ "An Echocardiographic Study of Valvular Heart Disease Associated with Systemic Lupus Erythematosus | NEJM".
- ↑ "Non-infectious aortic and mitral valve vegetations in a patient with eosinophilic granulomatosis with polyangiitis | BMJ Case Reports".
- ↑ "NONBACTERIAL THROMBOTIC ENDOCARDITIS AS A CAUSE OF CEREBRAL AND MYOCARDIAL INFARCTION".
- ↑ Beck ML, Freihaut B, Henry R, Pierce S, Bayer WL, Hendrickson WA, Ward KB, Wolf P, Feller K, Femmer K, Mohn GR (January 1975). "A serum haemagglutinating property dependent upon polycarboxyl groups". Br. J. Haematol. 29 (1): 149–56. doi:10.1111/j.1365-2141.1975.tb01808.x. PMID 32.
- ↑ Williams R.C.Jr.. Immune complexes in clinical and experimental medicine, 19801st ed. p. 12
- ↑ Nakanishi K., Tajima F., Nakata Y., Osada H., Ogata K., Kawai T., Torikata C., Suga T., Takishima K., Aurues T., Ikeda T.. Tissue factor is associated with the nonbacterial thrombotic endocarditis induced by a hypobaric hypoxic environment in rats, Virchows Arch, 1998, vol. 433 (pg. 375-379)
- ↑ Dutta T., Karas M.G., Segal A.Z., Kizer J.R.. Yield of transesophageal echocardiography for nonbacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia, Am J Cardiol, 2006, vol. 97 6(pg. 894-898)
- ↑ MacDonald R.A., Robbins S.L.. The significance of nonbacterial thrombotic endocarditis: an autopsy and clinical study of 78 cases, Am Intern Med, 1957, vol. 46 (pg. 255-273)
- ↑ "Nonbacterial thrombotic endocarditis in cancer patients: Comparison of characteristics of patients with and without concomitant disseminated intravascular coagulation - Bedikian - 1978 - Medical and Pediatric Oncology - Wiley Online Library".
- ↑ Williams R.C.Jr.. Immune complexes in clinical and experimental medicine, 19801st ed. p. 12
- ↑ Shapiro RF, Gamble CN, Wiesner KB, Castles JJ, Wolf AW, Hurley EJ, Salel AF (December 1977). "Immunopathogenesis of Libman-Sacks endocarditis. Assessment by light and immunofluorescent microscopy in two patients". Ann. Rheum. Dis. 36 (6): 508–16. doi:10.1136/ard.36.6.508. PMC 1000155. PMID 339850.
- ↑ Nydegger UE, Lambert PH, Gerber H, Miescher PA (August 1974). "Circulating immune complexes in the serum in systemic lupus erythematosus and in carriers of hepatitis B antigen. Quantitation by binding to radiolabeled C1q". J. Clin. Invest. 54 (2): 297–309. doi:10.1172/JCI107765. PMC 301557. PMID 4847246.
- ↑ 15.0 15.1 15.2 Dutta T, Karas MG, Segal AZ, Kizer JR (March 2006). "Yield of transesophageal echocardiography for nonbacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia". Am. J. Cardiol. 97 (6): 894–8. doi:10.1016/j.amjcard.2005.09.140. PMID 16516597.
- ↑ 16.0 16.1 Truskinovsky AM, Hutchins GM (April 2001). "Association between nonbacterial thrombotic endocarditis and hypoxigenic pulmonary diseases". Virchows Arch. 438 (4): 357–61. doi:10.1007/s004280000372. PMID 11355169.
- ↑ 17.0 17.1 Nakanishi K, Tajima F, Nakata Y, Osada H, Ogata K, Kawai T, Torikata C, Suga T, Takishima K, Aurues T, Ikeda T (October 1998). "Tissue factor is associated with the nonbacterial thrombotic endocarditis induced by a hypobaric hypoxic environment in rats". Virchows Arch. 433 (4): 375–9. doi:10.1007/s004280050262. PMID 9808440.
- ↑ Metharom P, Falasca M, Berndt MC (January 2019). "The History of Armand Trousseau and Cancer-Associated Thrombosis". Cancers (Basel). 11 (2). doi:10.3390/cancers11020158. PMC 6406548. PMID 30708967.
- ↑ "THE SIGNIFICANCE OF NONBACTERIAL THROMBOTIC ENDOCARDITIS: AN AUTOPSY AND CLINICAL STUDY OF 78 CASES | Annals of Internal Medicine".
- ↑ Sanjay Asopa, Anish Patel, Omar A. Khan, Rajan Sharma, Sunil K. Ohri, Non-bacterial thrombotic endocarditis, European Journal of Cardio-Thoracic Surgery, Volume 32, Issue 5, November 2007, Pages 696–701, https://doi.org/10.1016/j.ejcts.2007.07.029
- ↑ Borowski A, Ghodsizad A, Cohnen M, Gams E (June 2005). "Recurrent embolism in the course of marantic endocarditis". Ann. Thorac. Surg. 79 (6): 2145–7. doi:10.1016/j.athoracsur.2003.12.024. PMID 15919332.
- ↑ Suzuki S, Tanaka K, Nogawa S, Umezawa A, Hata J, Fukuuchi Y (2002). "Expression of interleukin-6 in cerebral neurons and ovarian cancer tissue in Trousseau syndrome". Clin. Neuropathol. 21 (5): 232–5. PMID 12365726.
- ↑ "www.cancertherapyadvisor.com".
- ↑ Zakka K, Zakka P, Davarpanah A, Koshkelashvili N, Bilen MA, Owonikoko T, El-Rayes B, Akce M (2020). "Nonbacterial Thrombotic Endocarditis and Widespread Skin Necrosis in Newly Diagnosed Lung Adenocarcinoma". Case Rep Oncol. 13 (1): 239–244. doi:10.1159/000506453. PMC 7154248 Check
|pmc=value (help). PMID 32308583 Check|pmid=value (help). - ↑ Eiken PW, Edwards WD, Tazelaar HD, McBane RD, Zehr KJ (December 2001). "Surgical pathology of nonbacterial thrombotic endocarditis in 30 patients, 1985-2000". Mayo Clin. Proc. 76 (12): 1204–12. doi:10.4065/76.12.1204. PMID 11761501.
- ↑ Roldan CA, Sibbitt WL, Qualls CR, Jung RE, Greene ER, Gasparovic CM, Hayek RA, Charlton GA, Crookston K (September 2013). "Libman-Sacks endocarditis and embolic cerebrovascular disease". JACC Cardiovasc Imaging. 6 (9): 973–83. doi:10.1016/j.jcmg.2013.04.012. PMC 3941465. PMID 24029368.
- ↑ "Nonbacterial Thrombotic Endocarditis: Clinicopathologic Study of a Necropsy Series | Revista Española de Cardiología (English Edition)".
- ↑ "Cvs ie-csbrp".
- ↑ "Redirecting".