Niacin (tablet): Difference between revisions
Kiran Singh (talk | contribs) No edit summary |
m (Protected "Niacin (tablet)": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (16 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
{{DrugProjectFormSinglePage | {{DrugProjectFormSinglePage | ||
|authorTag={{KS}} | |authorTag={{KS}} | ||
|aOrAn= | |genericName=niacin | ||
|aOrAn=an | |||
|drugClass=antihyperlipedemic agent | |||
|indicationType=treatment | |indicationType=treatment | ||
|adverseReactions= | |indication=[[hypertriglyceredemia]], [[hypercholesterolemia|primary hypercholesterolemia]], [[hyperlipidemia]] | ||
|adverseReactions=[[dyspepsia]], [[vomiting]], [[diarrhea]], [[jaundice]], [[pruritus]], [[hyperpigmentation]], [[acanthosis nigricans]], [[dry skin]] and [[headache]] | |||
|blackBoxWarningTitle=<span style="color:#FF0000;">ConditionName: </span> | |blackBoxWarningTitle=<span style="color:#FF0000;">ConditionName: </span> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | |blackBoxWarningBody=<i><span style="color:#FF0000;">ConditionName: </span></i> | ||
| Line 14: | Line 17: | ||
|fdaLIADAdult===Indications== | |fdaLIADAdult===Indications== | ||
* Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in individuals at significantly increased risk for atherosclerotic vascular disease due to | * Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in those individuals at significantly increased risk for atherosclerotic vascular disease due to [[hypercholesterolemia]]. Nicotinic acid, alone or in combination with a bile-acid binding resin, is indicated as an adjunct to diet for the reduction of elevated total and LDL cholesterol levels in patients with [[hypercholesterolemia|primary hypercholesterolemia]] (Types IIa and IIb)†, when the response to a diet restricted in saturated fat and cholesterol and other nonpharmacologic measures alone has been inadequate (see also the NCEP treatment guidelines6). Prior to initiating therapy with nicotinic acid, secondary causes for [[hypercholesterolemia]] (e.g., poorly controlled [[diabetes mellitus]], [[hypothyroidism]], [[nephrotic syndrome]], [[dysproteinemias]], obstructive liver disease, other drug therapy, alcoholism) should be excluded, and a lipid profile performed to measure total [[cholesterol]], [[HDL]] [[cholesterol]], and [[triglycerides]]. | ||
* | * Nicotinic acid is also indicated as adjunctive therapy for the treatment of adult patients with very high serum [[triglyceride]] levels (Types IV and V [[hyperlipidemia]])† who present a risk of [[pancreatitis]] and who do not respond adequately to a determined dietary effort to control them. Such patients typically have serum triglyceride levels over 2000 mg/dL and have elevations of VLDL cholesterol as well as fasting chylomicrons (Type V hyperlipidemia)†. Subjects who consistently have total serum or plasma [[triglycerides]] below 1000 mg/dL are unlikely to develop [[pancreatitis]]. Therapy with nicotinic acid may be considered for those subjects with triglyceride elevations between 1000 and 2000 mg/dL who have a history of [[pancreatitis]] or of recurrent [[abdominal pain]] typical of [[pancreatitis]]. Some Type IV patients with triglycerides under 1000 mg/dL may, through dietary or alcoholic indiscretion, convert to a Type V pattern with massive [[triglyceride]] elevations accompanying fasting chylomicronemia, but the influence of nicotinic acid therapy on the risk of [[pancreatitis]] in such situations has not been adequately studied. Drug therapy is not indicated for patients with Type I [[hyperlipoproteinemia]], who have elevations of chylomicrons and plasma [[triglycerides]], but who have normal levels of VLDL. Inspection of plasma refrigerated for 14 hours is helpful in distinguishing Types I, IV, and V hyperlipoproteinemia7. | ||
[[File:Niacor classification.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
==Dosage== | ==Dosage== | ||
* The usual adult dosage of nicotinic acid is 1 to 2 grams two or three times a day. Doses should be individualized according to the patient's response. Start with one-half tablet (250 mg) as a single daily dose following the evening meal. The frequency of dosing and total daily dose can be increased every four to seven days until the desired LDL cholesterol and/or triglyceride level is achieved or the first-level therapeutic dose of 1.5 to 2 grams/day is reached. If the patient's hyperlipidemia is not adequately controlled after 2 months at this level, the dosage can then be increased at two to four week intervals to 3 grams/day (1 gram three times per day). In patients with marked lipid abnormalities, a higher dose is occasionally required, but generally should not exceed 6 grams/day. | |||
[[ | * [[Flushing]] of the skin appears frequently and can be minimized by pretreatment with aspirin or non-steroidal anti-inflammatory drugs. Tolerance to this [[flushing]] develops rapidly over the course of several weeks. [[Flushing]], [[pruritus]], and gastrointestinal distress are also greatly reduced by slowly increasing the dose of nicotinic acid and avoiding administration on an empty stomach. | ||
* Sustained-release (modified-release, timed-release) nicotinic acid preparations should not be substituted for equivalent doses of immediate-release (crystalline) nicotinic acid. | |||
* | |||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | ||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | |offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in adult patients. | ||
<!-- | <!--FDA-Labeled Indications and Dosage (Pediatric)--> | ||
|fdaLIADPed=There is limited information regarding <i>FDA-Labeled Use</i> of {{PAGENAME}} in pediatric patients. | |||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | |offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | ||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | |offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of {{PAGENAME}} in pediatric patients. | ||
|contraindications=* | |contraindications=* Nicotinic acid is contraindicated in patients with a known [[hypersensitivity]] to any component of this medication; significant or unexplained [[hepatic dysfunction]]; active [[peptic ulcer]] disease; or arterial bleeding. | ||
|warnings='''Liver Dysfunction''' | |||
* Cases of severe hepatic toxicity, including [[fulminant hepatic necrosis]] have occurred in patients who have substituted sustained-release (modified-release, timed-release) nicotinic acid products for immediate-release (crystalline) nicotinic acid at equivalent doses. | |||
* Liver function tests should be performed on all patients during therapy with nicotinic acid. Serum transaminase levels, including ALT (SGPT), should be monitored before treatment begins, every six weeks to twelve weeks for the first year, and periodically thereafter (e.g., at approximately 6 month intervals). Special attention should be paid to patients who develop elevated serum transaminase levels, and in these patients, measurements should be repeated promptly and then performed more frequently. If the transaminase levels show evidence of progression, particularly if they rise to three times the upper limit of normal and are persistent, the drug should be discontinued. Liver biopsy should be considered if elevations persist beyond discontinuation of the drug. | |||
* | * Nicotinic acid should be used with caution in patients who consume substantial quantities of alcohol and/or have a past history of liver disease. Active liver diseases or unexplained transaminase elevations are contraindications to the use of nicotinic acid. | ||
'''Skeletal Muscle''' | '''Skeletal Muscle''' | ||
* | * Rare cases of [[rhabdomyolysis]] have been associated with concomitant administration of lipid-altering doses (≥1 g/day) of nicotinic acid and [[HMG-CoA reductase inhibitors]]. Physicians contemplating combined therapy with [[HMG-CoA reductase inhibitors]] and nicotinic acid should carefully weigh the potential benefits and risks and should carefully monitor patients for any signs and symptoms of muscle pain, tenderness, or weakness, particularly during the initial months of therapy and during any periods of upward dosage titration of either drug. Periodic serum creatine phosphokinase (CPK) and potassium determinations should be considered in such situations, but there is no assurance that such monitoring will prevent the occurrence of severe [[myopathy]]. | ||
|clinicalTrials=* '''Cardiovascular''' : [[Atrial fibrillation]] and other [[cardiac arrhythmias]], [[orthostasis]], [[hypotension]]. | |||
|clinicalTrials=* | |||
''' | |||
''' | * '''Gastrointestinal''' : [[Dyspepsia]], [[vomiting]], [[diarrhea]], [[peptic ulceration]], [[jaundice]], [[abnormal liver function tests]]. | ||
* | * '''Skin''' : Mild to severe cutaneous [[flushing]], [[pruritus]], [[hyperpigmentation]], [[acanthosis nigricans]], [[dry skin]]. | ||
''' | * '''Metabolic''' : Decreased glucose tolerance, [[hyperuricemia]], [[gout]]. | ||
* | * '''Eye''' : Toxic [[amblyopia]], cystoid macular [[edema]]. | ||
''' | * '''Nervous System''' / '''Psychiatric''' : [[Headache]]. | ||
|postmarketing=There is limited information regarding <i>Postmarketing Experience</i> of {{PAGENAME}} in the drug label. | |||
|drugInteractions='''HMG-CoA Reductase Inhibitors''': | |||
'''Antihypertensive Therapy''' : Nicotinic acid may potentiate the effects of ganglionic blocking agents and vasoactive drugs resulting in postural [[hypotension]]. | |||
''' | '''Aspirin''' : Concomitant aspirin may decrease the metabolic clearance of nicotinic acid. The clinical relevance of this finding is unclear. | ||
'''Other''': Concomitant alcohol or hot drinks may increase the side effects of [[flushing]] and [[pruritus]] and should be avoided at the time of drug ingestion. | |||
|useInPregnancyFDA='''Pregnancy Category C'''. | |useInPregnancyFDA='''Pregnancy Category C'''. | ||
* Animal reproduction studies have not been conducted with | * Animal reproduction studies have not been conducted with nicotinic acid. It is also not known whether nicotinic acid at doses typically used for lipid disorders can cause fetal harm when administered to pregnant women or whether it can affect reproductive capacity. If a woman receiving nicotinic acid for primary hypercholesterolemia (Types IIa or IIb) becomes pregnant, the drug should be discontinued. If a woman being treated with nicotinic acid for [[hypertriglyceridemia]] (Types IV or V) conceives, the benefits and risks of continued drug therapy should be assessed on an individual basis. | ||
|useInPregnancyAUS=There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | |||
|useInPregnancyAUS= | |||
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of {{PAGENAME}} in women who are pregnant. | |||
|useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | |useInLaborDelivery=There is no FDA guidance on use of {{PAGENAME}} during labor and delivery. | ||
|useInNursing=* | |useInNursing=* It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from lipid-altering doses of nicotinic acid, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. | ||
|useInPed=* Safety and effectiveness | |useInPed=* Safety and effectiveness in children and adolescents have not been established. | ||
|useInGeri= | |useInGeri=There is no FDA guidance on the use of {{PAGENAME}} with respect to geriatric patients. | ||
|useInGender= | |useInGender=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific gender populations. | ||
|useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | |useInRace=There is no FDA guidance on the use of {{PAGENAME}} with respect to specific racial populations. | ||
|useInRenalImpair= | |useInRenalImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with renal impairment. | ||
|useInHepaticImpair= | |useInHepaticImpair=There is no FDA guidance on the use of {{PAGENAME}} in patients with hepatic impairment. | ||
|useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | |useInReproPotential=There is no FDA guidance on the use of {{PAGENAME}} in women of reproductive potentials and males. | ||
|useInImmunocomp=There is no FDA guidance one the use of {{PAGENAME}} in patients who are immunocompromised. | |useInImmunocomp=There is no FDA guidance one the use of {{PAGENAME}} in patients who are immunocompromised. | ||
|administration=* Oral | |administration=* Oral | ||
|monitoring=There is limited information regarding <i>Monitoring</i> of {{PAGENAME}} in the drug label. | |monitoring=There is limited information regarding <i>Monitoring</i> of {{PAGENAME}} in the drug label. | ||
|IVCompat=There is limited information regarding <i>IV Compatibility</i> of {{PAGENAME}} in the drug label. | |IVCompat=There is limited information regarding <i>IV Compatibility</i> of {{PAGENAME}} in the drug label. | ||
|overdose=* Supportive measures should be undertaken in the event of an overdose. | |overdose=* Supportive measures should be undertaken in the event of an overdose. | ||
|drugBox=< | |drugBox=[[File:Niacin wikipedia.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
| | |mechAction=There is limited information regarding <i>Mechanism of action</i> of {{PAGENAME}} in the drug label. | ||
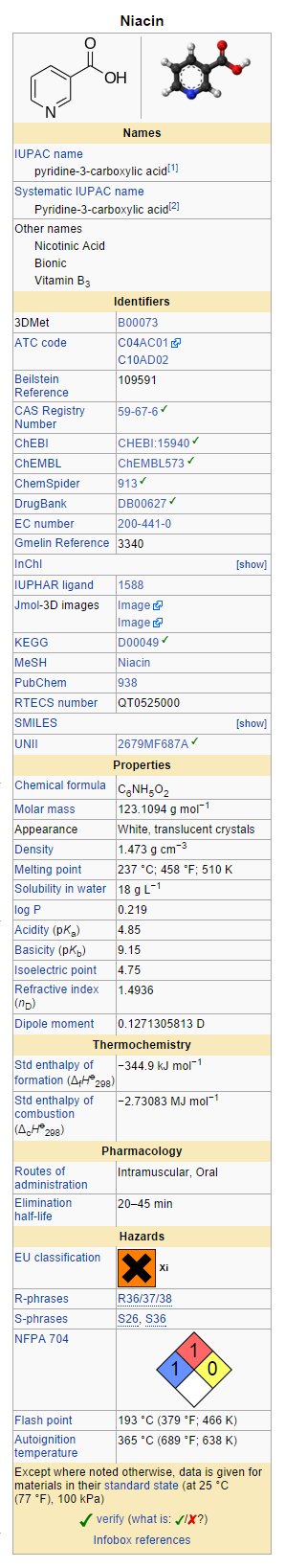
|structure=* Niacin or nicotinic acid, a water-soluble B-complex vitamin and antihyperlipidemic agent, is 3-pyridinecarboxylic acid. It is a white, crystalline powder, sparingly soluble in water. It has the following structural formula: | |||
[[File:Niacor structure.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
| | |||
* Each NIACOR® Tablet, for oral administration, contains 500 mg of nicotinic acid. In addition, each tablet contains the following inactive ingredients: croscarmellose sodium, hydrogenated vegetable oil, magnesium stearate and microcrystalline cellulose. | |||
|PD=There is limited information regarding <i>Pharmacodynamics</i> of {{PAGENAME}} in the drug label. | |PD=There is limited information regarding <i>Pharmacodynamics</i> of {{PAGENAME}} in the drug label. | ||
|PK=* Following an oral dose, the pharmacokinetic profile of nicotinic acid is characterized by rapid absorption from the gastrointestinal tract and a short plasma elimination half-life. At a 1 gram dose, peak plasma concentrations of 15 to 30 μg/mL are reached within 30 to 60 minutes. Approximately 88% of an oral pharmacologic dose is eliminated by the kidneys as unchanged drug and nicotinuric acid, its primary metabolite. The plasma elimination half-life of nicotinic acid ranges from 20 to 45 minutes. | |||
|nonClinToxic='''Carcinogenesis, Mutagenesis, Impairment of Fertility''' | |||
* Nicotinic acid administered to mice for a lifetime as a 1% solution in drinking water was not carcinogenic. The mice in this study received approximately 6-8 times a human dose of 3000 milligrams/day as determined on a milligram/square meter basis. Nicotinic acid was negative for mutagenicity in the Ames test. No studies on impairment of fertility have been performed. | |||
|clinicalStudies=There is limited information regarding <i>Clinical Studies</i> of {{PAGENAME}} in the drug label. | |||
|howSupplied='''NIACOR®(Niacin Tablets, USP) 500 mg'''. | |||
* | |||
|clinicalStudies= | |||
''' | |||
* Each tablet is a white, capsule-shaped, scored, uncoated tablet, debossed “US” to the left and “67” to the right of the score, with “500” strength on the unscored side. | |||
* NIACOR® is available in bottles of 100 tablets (NDC 0245-0067-11). | |||
[[File: | * Dispense in a tight container as defined in the USP, with a child-resistant closure. | ||
|storage=* Store at controlled room temperature, 15-30°C (59-86°F). | |||
|packLabel=[[File:Niacor image.jpg|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
[[File:Niacor ingredients and appearance.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | |||
[[File: | |||
|fdaPatientInfo=There is limited information regarding <i>Patient Counseling Information</i> of {{PAGENAME}} in the drug label. | |fdaPatientInfo=There is limited information regarding <i>Patient Counseling Information</i> of {{PAGENAME}} in the drug label. | ||
|alcohol=* Alcohol-{{PAGENAME}} interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=* Alcohol-{{PAGENAME}} interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
|brandNames=* NIACOR ®<ref>{{Cite web | title =niacin tablet| url =http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=ce739d68-d89c-437c-90fb-3c0c45140f22 }}</ref> | |||
|brandNames=* ®<ref>{{Cite web | title = | |||
|lookAlike=* A® — B®<ref name="www.ismp.org">{{Cite web | last = | first = | title = http://www.ismp.org | url = http://www.ismp.org | publisher = | date = }}</ref> | |lookAlike=* A® — B®<ref name="www.ismp.org">{{Cite web | last = | first = | title = http://www.ismp.org | url = http://www.ismp.org | publisher = | date = }}</ref> | ||
|drugShortage= | |drugShortage= | ||
}} | }} | ||
Latest revision as of 16:47, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Niacin (tablet) is an antihyperlipedemic agent that is FDA approved for the treatment of hypertriglyceredemia, primary hypercholesterolemia, hyperlipidemia. Common adverse reactions include dyspepsia, vomiting, diarrhea, jaundice, pruritus, hyperpigmentation, acanthosis nigricans, dry skin and headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in those individuals at significantly increased risk for atherosclerotic vascular disease due to hypercholesterolemia. Nicotinic acid, alone or in combination with a bile-acid binding resin, is indicated as an adjunct to diet for the reduction of elevated total and LDL cholesterol levels in patients with primary hypercholesterolemia (Types IIa and IIb)†, when the response to a diet restricted in saturated fat and cholesterol and other nonpharmacologic measures alone has been inadequate (see also the NCEP treatment guidelines6). Prior to initiating therapy with nicotinic acid, secondary causes for hypercholesterolemia (e.g., poorly controlled diabetes mellitus, hypothyroidism, nephrotic syndrome, dysproteinemias, obstructive liver disease, other drug therapy, alcoholism) should be excluded, and a lipid profile performed to measure total cholesterol, HDL cholesterol, and triglycerides.
- Nicotinic acid is also indicated as adjunctive therapy for the treatment of adult patients with very high serum triglyceride levels (Types IV and V hyperlipidemia)† who present a risk of pancreatitis and who do not respond adequately to a determined dietary effort to control them. Such patients typically have serum triglyceride levels over 2000 mg/dL and have elevations of VLDL cholesterol as well as fasting chylomicrons (Type V hyperlipidemia)†. Subjects who consistently have total serum or plasma triglycerides below 1000 mg/dL are unlikely to develop pancreatitis. Therapy with nicotinic acid may be considered for those subjects with triglyceride elevations between 1000 and 2000 mg/dL who have a history of pancreatitis or of recurrent abdominal pain typical of pancreatitis. Some Type IV patients with triglycerides under 1000 mg/dL may, through dietary or alcoholic indiscretion, convert to a Type V pattern with massive triglyceride elevations accompanying fasting chylomicronemia, but the influence of nicotinic acid therapy on the risk of pancreatitis in such situations has not been adequately studied. Drug therapy is not indicated for patients with Type I hyperlipoproteinemia, who have elevations of chylomicrons and plasma triglycerides, but who have normal levels of VLDL. Inspection of plasma refrigerated for 14 hours is helpful in distinguishing Types I, IV, and V hyperlipoproteinemia7.

Dosage
- The usual adult dosage of nicotinic acid is 1 to 2 grams two or three times a day. Doses should be individualized according to the patient's response. Start with one-half tablet (250 mg) as a single daily dose following the evening meal. The frequency of dosing and total daily dose can be increased every four to seven days until the desired LDL cholesterol and/or triglyceride level is achieved or the first-level therapeutic dose of 1.5 to 2 grams/day is reached. If the patient's hyperlipidemia is not adequately controlled after 2 months at this level, the dosage can then be increased at two to four week intervals to 3 grams/day (1 gram three times per day). In patients with marked lipid abnormalities, a higher dose is occasionally required, but generally should not exceed 6 grams/day.
- Flushing of the skin appears frequently and can be minimized by pretreatment with aspirin or non-steroidal anti-inflammatory drugs. Tolerance to this flushing develops rapidly over the course of several weeks. Flushing, pruritus, and gastrointestinal distress are also greatly reduced by slowly increasing the dose of nicotinic acid and avoiding administration on an empty stomach.
- Sustained-release (modified-release, timed-release) nicotinic acid preparations should not be substituted for equivalent doses of immediate-release (crystalline) nicotinic acid.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Niacin (tablet) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Niacin (tablet) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Niacin (tablet) in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Niacin (tablet) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Niacin (tablet) in pediatric patients.
Contraindications
- Nicotinic acid is contraindicated in patients with a known hypersensitivity to any component of this medication; significant or unexplained hepatic dysfunction; active peptic ulcer disease; or arterial bleeding.
Warnings
Liver Dysfunction
- Cases of severe hepatic toxicity, including fulminant hepatic necrosis have occurred in patients who have substituted sustained-release (modified-release, timed-release) nicotinic acid products for immediate-release (crystalline) nicotinic acid at equivalent doses.
- Liver function tests should be performed on all patients during therapy with nicotinic acid. Serum transaminase levels, including ALT (SGPT), should be monitored before treatment begins, every six weeks to twelve weeks for the first year, and periodically thereafter (e.g., at approximately 6 month intervals). Special attention should be paid to patients who develop elevated serum transaminase levels, and in these patients, measurements should be repeated promptly and then performed more frequently. If the transaminase levels show evidence of progression, particularly if they rise to three times the upper limit of normal and are persistent, the drug should be discontinued. Liver biopsy should be considered if elevations persist beyond discontinuation of the drug.
- Nicotinic acid should be used with caution in patients who consume substantial quantities of alcohol and/or have a past history of liver disease. Active liver diseases or unexplained transaminase elevations are contraindications to the use of nicotinic acid.
Skeletal Muscle
- Rare cases of rhabdomyolysis have been associated with concomitant administration of lipid-altering doses (≥1 g/day) of nicotinic acid and HMG-CoA reductase inhibitors. Physicians contemplating combined therapy with HMG-CoA reductase inhibitors and nicotinic acid should carefully weigh the potential benefits and risks and should carefully monitor patients for any signs and symptoms of muscle pain, tenderness, or weakness, particularly during the initial months of therapy and during any periods of upward dosage titration of either drug. Periodic serum creatine phosphokinase (CPK) and potassium determinations should be considered in such situations, but there is no assurance that such monitoring will prevent the occurrence of severe myopathy.
Adverse Reactions
Clinical Trials Experience
- Cardiovascular : Atrial fibrillation and other cardiac arrhythmias, orthostasis, hypotension.
- Gastrointestinal : Dyspepsia, vomiting, diarrhea, peptic ulceration, jaundice, abnormal liver function tests.
- Skin : Mild to severe cutaneous flushing, pruritus, hyperpigmentation, acanthosis nigricans, dry skin.
- Metabolic : Decreased glucose tolerance, hyperuricemia, gout.
- Nervous System / Psychiatric : Headache.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Niacin (tablet) in the drug label.
Drug Interactions
HMG-CoA Reductase Inhibitors:
Antihypertensive Therapy : Nicotinic acid may potentiate the effects of ganglionic blocking agents and vasoactive drugs resulting in postural hypotension.
Aspirin : Concomitant aspirin may decrease the metabolic clearance of nicotinic acid. The clinical relevance of this finding is unclear.
Other: Concomitant alcohol or hot drinks may increase the side effects of flushing and pruritus and should be avoided at the time of drug ingestion.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Pregnancy Category C.
- Animal reproduction studies have not been conducted with nicotinic acid. It is also not known whether nicotinic acid at doses typically used for lipid disorders can cause fetal harm when administered to pregnant women or whether it can affect reproductive capacity. If a woman receiving nicotinic acid for primary hypercholesterolemia (Types IIa or IIb) becomes pregnant, the drug should be discontinued. If a woman being treated with nicotinic acid for hypertriglyceridemia (Types IV or V) conceives, the benefits and risks of continued drug therapy should be assessed on an individual basis.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Niacin (tablet) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Niacin (tablet) during labor and delivery.
Nursing Mothers
- It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from lipid-altering doses of nicotinic acid, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness in children and adolescents have not been established.
Geriatic Use
There is no FDA guidance on the use of Niacin (tablet) with respect to geriatric patients.
Gender
There is no FDA guidance on the use of Niacin (tablet) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Niacin (tablet) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Niacin (tablet) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Niacin (tablet) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Niacin (tablet) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Niacin (tablet) in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Niacin (tablet) in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Niacin (tablet) in the drug label.
Overdosage
- Supportive measures should be undertaken in the event of an overdose.
Pharmacology
Mechanism of Action
There is limited information regarding Mechanism of action of Niacin (tablet) in the drug label.
Structure
- Niacin or nicotinic acid, a water-soluble B-complex vitamin and antihyperlipidemic agent, is 3-pyridinecarboxylic acid. It is a white, crystalline powder, sparingly soluble in water. It has the following structural formula:

- Each NIACOR® Tablet, for oral administration, contains 500 mg of nicotinic acid. In addition, each tablet contains the following inactive ingredients: croscarmellose sodium, hydrogenated vegetable oil, magnesium stearate and microcrystalline cellulose.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Niacin (tablet) in the drug label.
Pharmacokinetics
- Following an oral dose, the pharmacokinetic profile of nicotinic acid is characterized by rapid absorption from the gastrointestinal tract and a short plasma elimination half-life. At a 1 gram dose, peak plasma concentrations of 15 to 30 μg/mL are reached within 30 to 60 minutes. Approximately 88% of an oral pharmacologic dose is eliminated by the kidneys as unchanged drug and nicotinuric acid, its primary metabolite. The plasma elimination half-life of nicotinic acid ranges from 20 to 45 minutes.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Nicotinic acid administered to mice for a lifetime as a 1% solution in drinking water was not carcinogenic. The mice in this study received approximately 6-8 times a human dose of 3000 milligrams/day as determined on a milligram/square meter basis. Nicotinic acid was negative for mutagenicity in the Ames test. No studies on impairment of fertility have been performed.
Clinical Studies
There is limited information regarding Clinical Studies of Niacin (tablet) in the drug label.
How Supplied
NIACOR®(Niacin Tablets, USP) 500 mg.
- Each tablet is a white, capsule-shaped, scored, uncoated tablet, debossed “US” to the left and “67” to the right of the score, with “500” strength on the unscored side.
- NIACOR® is available in bottles of 100 tablets (NDC 0245-0067-11).
- Dispense in a tight container as defined in the USP, with a child-resistant closure.
Storage
- Store at controlled room temperature, 15-30°C (59-86°F).
Images
Drug Images
{{#ask: Page Name::Niacin (tablet) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


{{#ask: Label Page::Niacin (tablet) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Niacin (tablet) in the drug label.
Precautions with Alcohol
- Alcohol-Niacin (tablet) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- NIACOR ®[1]
Look-Alike Drug Names
- A® — B®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "niacin tablet".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Niacin (tablet)
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Niacin (tablet) |Label Name=Niacin (tablet)11.png
}}
{{#subobject:
|Label Page=Niacin (tablet) |Label Name=Niacin (tablet)11.png
}}