Mitral stenosis resident survival guide: Difference between revisions
Amr Marawan (talk | contribs) |
Amr Marawan (talk | contribs) |
||
| Line 241: | Line 241: | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree/end}} | {{familytree/end}} | ||
===Summary of Recommendations for Mitral Stenosis Surgery=== | |||
* [[PMBV|PMBC]] is recommended for symptomatic patients with sever [[mitral stenosis]] (MVA ≤ 1.5 cm², stage D) and favorabale valve morphology in the absence of contraindications ([[ACC AHA guidelines classification scheme|Class I, level of evidence A]]) <br> | |||
* Mitral valve surgery is indicated in severely symptomatic patients (NYHA class III/IV) with severe [[mitral stenosis]] (MVA ≤ 1.5 cm², stage D) who are not high risk for surgery and who are not candidates for or failed previous [[PMBV|PMBC]] ([[ACC AHA guidelines classification scheme|Class I, level of evidence B]])<br> | |||
* Concomitant mitral valve surgery is indicated for patients with severe [[mitral stenosis]] (MVA ≤ 1.5 cm², stage C or D) undergoing other cardiac surgery ([[ACC AHA guidelines classification scheme|Class I, level of evidence C]]) <br> | |||
* [[PMBV|PMBC]] is reasonable for asymptomatic patients with very severe [[mitral stenosis]] (MVA ≤ 1 cm², stage C) and favourable valve morphology in the absence of contraindications ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence C]]) <br> | |||
* Mitral valve surgery is reasonable for severely symptomatic patients with severe [[mitral stenosis]] (MVA ≤ 1.5 cm², stage D) provided that there is other operative indications ([[ACC AHA guidelines classification scheme|Class IIa, level of evidence C]])<br> | |||
* [[PMBV|PMBC]] may be considered for asymptomatic patients with [[mitral stenosis]] (MVA ≤ 1.5 cm², stage C) and favourable valve morphology who have new onset of [[atrial fibrillation]] in the absence of contraindications ([[ACC AHA guidelines classification scheme|Class IIb, level of evidence C]])<br> | |||
* [[PMBV|PMBC]] may be considered for symptomatic patients with MVA > 1.5 cm² if there is evidence of hemodynamically significant [[mitral stenosis]] during exercise ([[ACC AHA guidelines classification scheme|Class IIb, level of evidence C]]) <br> | |||
* [[PMBV|PMBC]] may be considered for severely symptomatic patients (NYHA III/IV) with severe [[mitral stenosis]] (MVA ≤ 1.5 cm², stage D) who have suboptimal valve anatomy and aren't candidates for surgery or at high risk for surgery ([[ACC AHA guidelines classification scheme|Class IIb, level of evidence C]]) <br> | |||
* Concomitant mitral valve surgery may be considered for patients with moderate [[mitral stenosis]] (MVA 1.6 - 2.0 cm²) undergoing other cardiac surgery ([[ACC AHA guidelines classification scheme|Class IIb, level of evidence C]]) <br> | |||
* Mitral valve surgery and excision of the left atrial appendage may be considered for patients with severe [[mitral stenosis]] (MVA ≤ 1.5 cm², stage C and D) who have recurrent embolic events while receiving adequate anticoagulation ([[ACC AHA guidelines classification scheme|Class IIb, level of evidence C]]) | |||
==Rheumatic Fever Prophylaxis== | ==Rheumatic Fever Prophylaxis== | ||
Revision as of 17:15, 22 April 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Twinkle Singh, M.B.B.S. [2]; Mohamed Moubarak, M.D. [3]
| Mitral Stenosis Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Rheumatic Fever Prophylaxis |
| Do's |
Overview
Mitral stenosis refers to abnormal narrowing of mitral orifice, which leads to obstruction of blood flow from left atrium to left ventricle. The most common presentations of mitral stenosis are dyspnea, orthopnea, paroxysmal nocturnal dyspnea, and peripheral edema. Mitral stenosis has a characteristic low-pitched, rumbling diastolic murmur, heard best at the apex during physical examination. The definitive therapy for mitral stenosis include percutaneous balloon valvotomy, surgical mitral valve repair, or mitral valve replacement.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in the salmon color signify that an urgent management is needed.
Identify cardinal findings that increase the pretest probability of mitral stenosis ❑ Mid diastolic murmur
| |||||||||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings of decompensated mitral stenosis that require urgent management? ❑ Tachycardia ❑ Hypotension ❑ Severe dyspnea ❑ Loss of consciousness ❑ Chest pain | |||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||
What is the complication of mitral stenosis that is causing decompensation? | |||||||||||||||||||||||||||||||||||||||||||||
❑ Suspect in case of:
| ❑ Suspect in case of palpitations ❑ Order an ECG immediately looking for | ❑ Suspect in case of:
| Pulmonary hypertension ± right sided heart failure ❑ Suspect in case of severe dyspnea ❑ Increased jugular venous pressure immediately ❑ Hepatomegaly ± pulsatile liver | ||||||||||||||||||||||||||||||||||||||||||
❑ Treat the complications of mitral stenosis that lead to decompensation ❑ Order a TTE to evaluate the severity of the mitral stenosis | |||||||||||||||||||||||||||||||||||||||||||||
When to consider intervention in mitral stenosis ? | |||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[2].
Abbreviations: AF: Atrial fibrillation; PMBC: Percutaneous mitral ballon commissurotomy; TR: Tricuspid regurgitation; S1: First heart sound; P2: Pulmonary component of second heart sound; EKG: Electrocardiogram; TTE: Transthoracic echocardiography; MS: Mitral stenosis
Characterize the symptoms: ❑ History of rheumatic fever | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vital signs ❑ Pulse
Neck: Chest examination: Auscultation
{{#ev:youtube|HW2pk1icYdM|250}} | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Order tests:
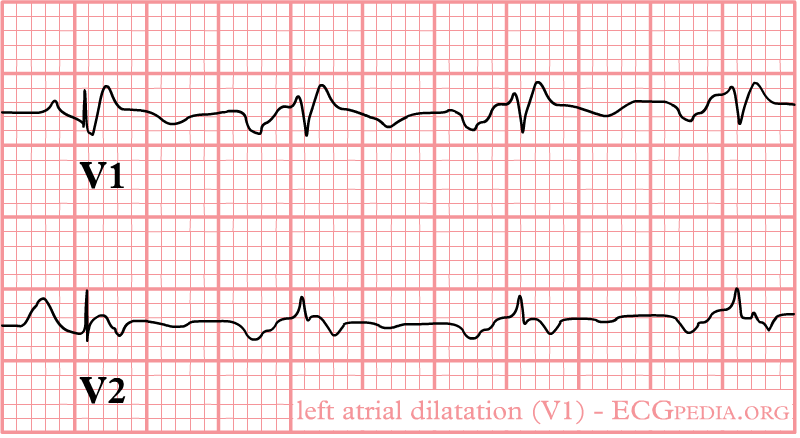
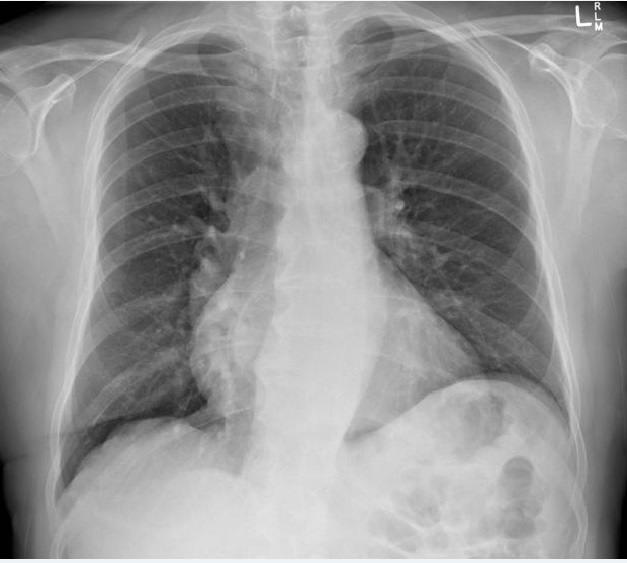
❑ Perform EKG
❑ Perform chest X-ray
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Consider alternative diagnosis: ❑ Myxoma
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Shown below is an algorithm summarizing the management of rheumatic mitral stenosis according to 2014 AHA/ACC guidelines for management of valvular heart disease.[2]
MVA: Mitral valve area; PMBC: Percutaneous mitral ballon commissurotomy; PCWP: Pulmonary capillary wedge pressure; ms: milliseconds; NYHA: New York Heart Association; AF: Atrial fibrillation
The filling of the left ventricle depends upon the diastole time which is limited by mitral stenosis. Therefore, slowing the heart rate is crucial in the initial management of mitral stenosis in order to improve the diastole time and consequently improve the filling of the left ventricle.
Medical therapy ❑ Consider heart rate control in MS patients with:
❑ Consider anticoagulation therapy in MS patients with:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Assess the presence of symptoms | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Symptomatic | Asymptomatic | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Assess the severity of mitral stenosis | ❑ Assess the severity of mitral stenosis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Progressive ❑ MVA > 1.5 cm2 ❑ Pressure half time < 150 ms | Progressive ❑ MVA > 1.5 cm2 Pressure half time < 150 ms | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess if valve morphology is favorable for PMBC | ❑ Perform exercise testing | ❑ Assess if valve morphology is favorable for PMBC | ❑ Assess if the new onset AF is present | ❑ Monitor patient periodically | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ❑ Assess PCWP on exercise | Yes | No | No | Yes | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Proceed with PMBC | If patient is severely symptomatic (NYHA III/IV): ❑ Assess the surgical risk of patient | ❑ Proceed with PMBC | ❑ Monitor patient periodically | ❑ Assess if the valve morphology is favorable for PMBC | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Proceed with PMBC | ❑ Proceed with mitral valve surgery | ❑ Proceed with PMBC | ❑ Monitor patient periodically | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Summary of Recommendations for Mitral Stenosis Surgery
- PMBC is recommended for symptomatic patients with sever mitral stenosis (MVA ≤ 1.5 cm², stage D) and favorabale valve morphology in the absence of contraindications (Class I, level of evidence A)
- Mitral valve surgery is indicated in severely symptomatic patients (NYHA class III/IV) with severe mitral stenosis (MVA ≤ 1.5 cm², stage D) who are not high risk for surgery and who are not candidates for or failed previous PMBC (Class I, level of evidence B)
- Concomitant mitral valve surgery is indicated for patients with severe mitral stenosis (MVA ≤ 1.5 cm², stage C or D) undergoing other cardiac surgery (Class I, level of evidence C)
- PMBC is reasonable for asymptomatic patients with very severe mitral stenosis (MVA ≤ 1 cm², stage C) and favourable valve morphology in the absence of contraindications (Class IIa, level of evidence C)
- Mitral valve surgery is reasonable for severely symptomatic patients with severe mitral stenosis (MVA ≤ 1.5 cm², stage D) provided that there is other operative indications (Class IIa, level of evidence C)
- PMBC may be considered for asymptomatic patients with mitral stenosis (MVA ≤ 1.5 cm², stage C) and favourable valve morphology who have new onset of atrial fibrillation in the absence of contraindications (Class IIb, level of evidence C)
- PMBC may be considered for symptomatic patients with MVA > 1.5 cm² if there is evidence of hemodynamically significant mitral stenosis during exercise (Class IIb, level of evidence C)
- PMBC may be considered for severely symptomatic patients (NYHA III/IV) with severe mitral stenosis (MVA ≤ 1.5 cm², stage D) who have suboptimal valve anatomy and aren't candidates for surgery or at high risk for surgery (Class IIb, level of evidence C)
- Concomitant mitral valve surgery may be considered for patients with moderate mitral stenosis (MVA 1.6 - 2.0 cm²) undergoing other cardiac surgery (Class IIb, level of evidence C)
- Mitral valve surgery and excision of the left atrial appendage may be considered for patients with severe mitral stenosis (MVA ≤ 1.5 cm², stage C and D) who have recurrent embolic events while receiving adequate anticoagulation (Class IIb, level of evidence C)
Rheumatic Fever Prophylaxis
Shown below is the table depicting the secondary prophylaxis of rheumatic fever according to the 2014 AHA/ACC guideline for the management of valvular heart disease.[3]
| ||||||||||
| Indications | Duration of prophylaxis |
| ▸ Rheumatic fever with carditis and persistent valvular heart disease | ▸ 10 years or until the patient is 40 years (whichever is longer) |
| ▸ Rheumatic fever with carditis but no valvular heart disease | ▸ 10 years or until the patient is 21 years (whichever is longer) |
| ▸ Rheumatic fever without carditis | ▸ 5 years or until the patient is 21 years (whichever is longer) |
Do's
- Perform transesophageal echocardiography (TEE) in patients considered for PMBC to rule out left atrial thrombus and to determine mitral regurgitation severity.
- Perform exercise testing or invasive hemodynamic testing, when clinical signs and symptoms don't co-relate with echocardiographic findings.
- Perform mitral valve surgery in stage C and stage D mitral stenosis, if patient is undergoing cardiac surgery for some other indication.
- Perform mitral valve surgery in moderate mitral stenosis (mitral valve area: 1.6 - 2 cm2) if the patient is undergoing cardiac surgery for other indications.
- Perform mitral valve surgery with excision of left atrial appendage in stage C and stage D mitral stenosis patients who have had recurrent embolic events despite being on anticoagulation therapy.
- Perform TTE every 3-5 years in asymptomatic stage B MS patients and every 1-2 years in asymptomatic stage C MS patients who have mitral valve area 1-1.5 cm2 .
- Perform TTE once every year in asymptomatic stage C MS patients who have mitral valve area < 1 cm2.
- In cases of senile calcific mitral stenosis, intervention is done only when symptoms are severe and cannot be controlled with heart rate control and diuretics.
References
- ↑ Tadele, H.; Mekonnen, W.; Tefera, E. (2013). "Rheumatic mitral stenosis in Children: more accelerated course in sub-Saharan Patients". BMC Cardiovasc Disord. 13 (1): 95. doi:10.1186/1471-2261-13-95. PMID 24180350. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000031. PMID 24589853.