Mitral regurgitation resident survival guide: Difference between revisions
| Line 39: | Line 39: | ||
: ❑ [[Tachycardia]]<br> | : ❑ [[Tachycardia]]<br> | ||
: ❑ [[Hypotension]] (due to [[cardiogenic shock]]) | : ❑ [[Hypotension]] (due to [[cardiogenic shock]]) | ||
: ❑ [[Irregularly irregular pulse | : ❑ [[Irregularly irregular pulse]] (with onset of [[AF]])<br> | ||
: ❑ [[Pulse]] is reduced in volume<br> | : ❑ [[Pulse]] is reduced in volume<br> | ||
'''Neck''':<br> | '''Neck''':<br> | ||
❑ [[Jugular venous distension]]<br> | ❑ [[Jugular venous distension]]<br> | ||
Revision as of 16:40, 12 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Overview
Mitral regurgitation refers to the disruption of mitral valve apparatus causing inability of the valve to close properly during systole. This leads to leakage of blood flow from left ventricle to left atrium during systole and reduction in cardiac output.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Dilated cardiomyopathy
- Infective endocarditis
- Ischemic heart disease
- Marfan's syndrome
- Mitral annular calcification[1]
- Myxomatous degeneration
- Rheumatic fever
Diagnosis
Shown below is an algorithm summarizing the approach to the initial evaluation of mitral regurgitation according to 2014 AHA/ACC guidelines for management of valvular heart disease.[2].
AF: Atrial fibrillation; PMBC: Percutaneous mitral ballon commissurotomy; TR: Tricuspid regurgitation; S1: First heart sound; P2: Pulmonary component of second heart sound; EKG: Electrocardiogram; TTE: Transthoracic echocardiography; MS: Mitral stenosis
Characterize the symptoms: Acute MR: | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient:
Neck: Chest:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Medical therapy ❑ Consider heart rate control in MS patients with:
❑ Consider anticoagulation therapy in MS patients with:
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Diagnosis
Symptoms
- Acute mitral regurgitation causes the following symptoms:
- Chronic mitral regurgitation may have a prolonged asymptomatic interval phase until the heart decompensates and the symptoms of low cardiac output and pulmonary congestion start. By the time the symptoms develop, left ventricular dysfunction may have already occurred.
Physical Examination
- S3 and S4 may be heard on auscultation.
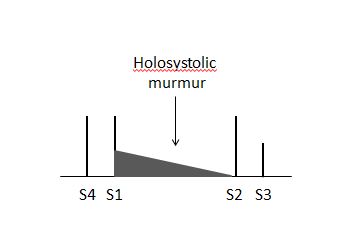
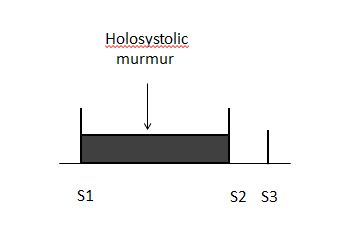
- A holosystolic murmur is heard in the apical region of the heart. MR murmur radiates to the axillary region. It may be soft, short and even absent. 70% of the cases of papillary muscle rupture have no murmur.
 |
 |
Imaging
Transthoracic echocardiography
Echocardiographic findings indicating the presence of severe mitral regurgitation include:
- Regurgitant volume >60 ml
- Regurgitant fraction >55%
- Effective regurgitant orifice (ERO) (ratio of regurgitant flow volume to the velocity of the mitral insufficiency jet: ERO = Flow / Velocity) >0.4 cm2
- If the left ventricular and left atrial sizes are normal on echocardiography, mitral regurgitation is not severe.
- Central jets indicate the presence of a fairly normal mitral valve and therefore the mitral regurgitation is not severe.
- Wide eccentric jets indicate that the regurgitation is severe.
- Echocardiographic findings must match the symptoms, if they do not, perform transesophageal echocardiography (TEE) or cardiac catheterization. TTE can underestimate the magnitude of mitral regurgitation in patients with clinical signs of severe MR.
Treatment
Acute Severe Mitral Regurgitation
- Treatment of acute severe mitral regurgitation depends on the stability of the patient.If the patient is clinically stable, the treatment options are:
- IV vasodilators, diuretics, antibiotics, anti-ischemic agents
- Surgery is preferred in the following cases:
- Endocarditis with progressive congestive heart failure
- No response to antibiotics
- Abscess formation
- Recurrent embolization
- If the patient is clinically unstable , the treatment options are:
- IV nitroprusside is used to maintain blood pressure. Ionotropes are added when needed.
- If medical therapy is not effective, an intra aortic balloon pump can be inserted to maintain hemodynamic stability.
- Surgical treatment is usually indicated.
- Knowledge of the etiology of the mitral regurgitation is important to know if the valve can be repaired or replaced.
Chronic Mitral Regurgitation
Why the Mitral valve is replaced Before Symptoms in Patients with Chronic Mitral Regurgitation
- Mitral regurgitation is a syndrome of pure volume overload whereas aortic regurgitation is a combination of both volume and pressure overload.
- Both syndromes are associated with an increase in preload.
- in mitral regurgitation, the afterload is reduced whereas in aortic regurgitation the afterload is increased. This is very important because when the mitral valve is repaired, there is no longer a reduction afterload and the left ventricle may fail due to an abrupt rise in the afterload. In aortic regurgitation, because the afterload is already increased chronically, replacement of the valve is not as likely to precipitate acute left ventricular failure due to an abrupt rise in afterload.
- By the time symptoms develop, there is already left ventricular dysfunction.
- Because of the low pressure system into which the blood is ejected into through the mitral valve, the ejection fraction is always high in mitral regurgitation. If the ejection fraction appears to be "normal", there is already decline in left ventricular function.
- There is no indication for vasodilator therapy in the absence of systemic hypertension in asymptomatic patients with preserved left ventricular function.
Indications for Surgery in Chronic Mitral Regurgitation
The indications for surgery in chronic mitral regurgitation are:
- Any symptoms - this is unlike mitral stenosis where surgeons operate on the heart when patients have class III or IV symptoms.
- Severe organic MR.
- Left ventricular dysfunction - ejection fraction <60% and end systolic diameter >40 mm2.
- Surgery can be considered in asymptomatic patients in the following cases:
- Truly severe MR
- Low operative mortality
- High chance of successful repair (e.g: posterior leaflet - MVP)
- Pre-operative ejection fraction has a prognostic impact in patients who undergo mitral valve repair or replacement. The lower the ejection fraction is, the higher the mortality is.
References
- ↑ Otto CM (2001). "Clinical practice. Evaluation and management of chronic mitral regurgitation". N Engl J Med. 345 (10): 740–6. doi:10.1056/NEJMcp003331. PMID 11547744.
- ↑ Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. doi:10.1161/CIR.0000000000000029. PMID 24589852.