Melanoma natural history, complications and prognosis
|
Melanoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Melanoma natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Melanoma natural history, complications and prognosis |
|
FDA on Melanoma natural history, complications and prognosis |
|
CDC on Melanoma natural history, complications and prognosis |
|
Melanoma natural history, complications and prognosis in the news |
|
Blogs on Melanoma natural history, complications and prognosis |
|
Risk calculators and risk factors for Melanoma natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Features that affect prognosis are tumor thickness in millimeters (Breslow's depth), depth related to skin structures (Clark level), type of melanoma, presence of ulceration, presence of lymphatic/perineural invasion, presence of tumor infiltrating lymphocytes (if present, prognosis is better), location of lesion, presence of satellite lesions, and presence of regional or distant metastasis.[1] Between 2004 and 2010, the 5-year relative survival of patients with melanoma was 92.9%.[2]
Complications
- Bone metastases
- Cerebral metastases
- Cutaneous metastasis
- Lung metastases
- Renal metastases
Prognosis
- Features that affect prognosis include tumor thickness in millimeters (Breslow's depth), depth related to skin structures (Clark level), type of melanoma, presence of ulceration, presence of lymphatic/perineural invasion, presence of tumor infiltrating lymphocytes (if present, prognosis is better), location of lesion, presence of satellite lesions, and presence of regional or distant metastasis.[3]
- The TNM staging classification summarizes most of these findings. Using the TNM classification, prognosis can be determined based on the stage of the disease as follows:
- Stage 0: Melanoma in Situ, 100% Survival
- Stage I: Invasive Melanoma, 85-95% Survival
- Stage II: High Risk Melanoma, 40-85% Survival
- Stage III: Regional Metastasis, 25-60% Survival
- Stage IV: Distant Metastasis, 9-15% Survival
Please check the staging page for more details about the staging scheme and the TNM classification.
- The Breslow's depth is independent of other features of the tumor, and has been demonstrated to predict 5-year survival:
| Breslow's Depth | 5-year survival |
|---|---|
| < 0.76 mm | 95% to 100% |
| 0.76-1.5 mm | 80% to 96% |
| 1.5-4 mm | 60% to 75% |
| > 4 mm | 37% to 50% |
- Extent of malignancy within a node is also important; micro-metastases in which malignancy is only microscopic have a more favorable prognosis than macrometastases.
- In some cases micrometastases may only be detected by special staining, and if malignancy is only detectable by a rarely-employed test known as polymerase chain reaction (PCR), the prognosis is better.
- Macrometastases in which malignancy is clinically apparent (in some cases cancer completely replaces a node) have a far worse prognosis, and if nodes are matted or if there is extracapsular extension, the prognosis is still worse.
- Metastases to skin and lungs have a better prognosis than metastases to the brain, bone and liver, which are associated with a worse prognosis.
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with melanoma was 92.9%.[2]
- When stratified by age, the 5-year relative survival of patients with melanoma was 92.7% and 88.2% for patients <65 and ≥ 65 years of age respectively.[2]
- When there is distant metastasis, the cancer is generally considered incurable. The five year survival rate is less than 10%.[4]
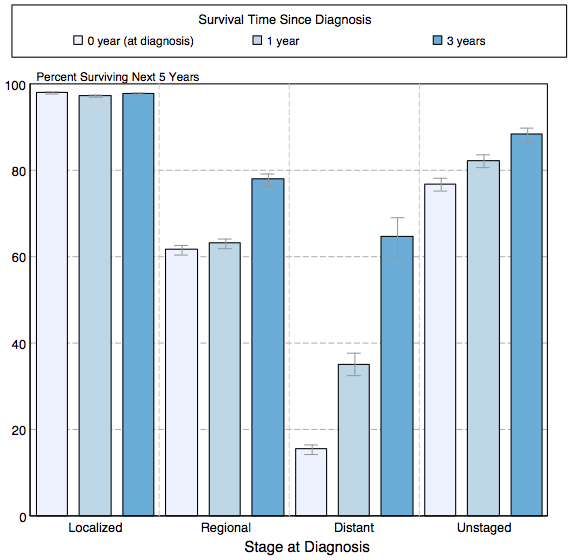
- The survival of patients with melanoma varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of melanoma:[2]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 91.3% |
| Localized | 98.1% |
| Regional | s62.6% |
| Distant | 16.1% |
| Unstaged | 78.4% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of melanoma by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[2]
References
- ↑ Homsi J, Kashani-Sabet M, Messina J, Daud A (2005). "Cutaneous melanoma: prognostic factors". Cancer Control. 12 (4): 223–9. PMID 16258493.Full text (PDF)
- ↑ 2.0 2.1 2.2 2.3 2.4 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
- ↑ Homsi J, Kashani-Sabet M, Messina J, Daud A (2005). "Cutaneous melanoma: prognostic factors". Cancer Control. 12 (4): 223–9. PMID 16258493.Full text (PDF)
- ↑ Balch C, Buzaid A, Soong S, Atkins M, Cascinelli N, Coit D, Fleming I, Gershenwald J, Houghton A, Kirkwood J, McMasters K, Mihm M, Morton D, Reintgen D, Ross M, Sober A, Thompson J, Thompson J (2001). "Final version of the American Joint Committee on Cancer staging system for cutaneous melanoma". J Clin Oncol. 19 (16): 3635–48. PMID 11504745.Full text