Melanoma natural history, complications and prognosis: Difference between revisions
YazanDaaboul (talk | contribs) |
YazanDaaboul (talk | contribs) |
||
| Line 15: | Line 15: | ||
*Bone | *Bone | ||
*Brain | *Brain | ||
*Liver | |||
*Kidney | |||
*Skin (distant site) | *Skin (distant site) | ||
==Prognosis== | ==Prognosis== | ||
Revision as of 03:48, 22 August 2015
|
Melanoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Melanoma natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Melanoma natural history, complications and prognosis |
|
FDA on Melanoma natural history, complications and prognosis |
|
CDC on Melanoma natural history, complications and prognosis |
|
Melanoma natural history, complications and prognosis in the news |
|
Blogs on Melanoma natural history, complications and prognosis |
|
Risk calculators and risk factors for Melanoma natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Serge Korjian M.D.; Yazan Daaboul, M.D.
Overview
If left untreated, melanoma progression occurs horizontally (radial growth plate) and vertically (vertical growth plate) and is then followed by dermal invasion and distant metastasis. Melanoma is an aggressive tumor characterized by early metastasis. Common sites of metastasis include bones, brain, kidneys, lungs, liver and skin (distant site). Complications of melanoma are usually related to the site of metastasis. The 5-year relative survival of patients with melanoma is approximately 93%.[1] Features associated with worse prognosis are tumor thickness (Breslow thickness), depth related to skin structures (Clark level), type of melanoma, presence of ulceration, presence of lymphatic/perineural invasion, location of lesion, presence of satellite lesions, and presence of regional or distant metastasis.[2]
Natural History
- If left untreated, melanocytes first proliferate randomly with an aberrant growth within an existing nevus.
- More advanced stages are characterized by a radial growth phase with intraepidermal growth and penetration into the papillary dermis.
- Final stages demonstrate a vertical growth phase with dermal invasion and widening of the papillary dermis before cancerous cells finally metastasize to other parts of the skin and other organs.
Complications
Complications of melanoma are usually due to distant metastasis. The most common sites of metastasis are shown below:
- Bone
- Brain
- Liver
- Kidney
- Skin (distant site)
Prognosis
Determinants of Prognosis
- Tumor thickness in millimeters (Breslow's depth)
- Depth related to skin structures (Clark level)
- Type of melanoma
- Presence of ulceration
- Presence of lymphatic/perineural invasion
- Presence of tumor infiltrating lymphocytes (if present, prognosis is better)
- Location of lesion
- Presence of satellite lesions
- Presence of regional or distant metastasis
TNM Staging
- The TNM staging classification summarizes most of these findings. Using the TNM classification, prognosis can be determined based on the stage of the disease as follows:
- Stage 0: Melanoma in Situ, 100% Survival
- Stage I: Invasive Melanoma, 85-95% Survival
- Stage II: High Risk Melanoma, 40-85% Survival
- Stage III: Regional Metastasis, 25-60% Survival
- Stage IV: Distant Metastasis, 9-15% Survival
Please check the staging page for more details about the staging scheme and the TNM classification.
Breslow's Depth
- The Breslow's depth is independent of other features of the tumor, and has been demonstrated to predict 5-year survival:
| Breslow's Depth | 5-year survival |
|---|---|
| < 0.76 mm | 95% to 100% |
| 0.76-1.5 mm | 80% to 96% |
| 1.5-4 mm | 60% to 75% |
| > 4 mm | 37% to 50% |
Micrometastasis vs. Macrometastasis
- Extent of malignancy within a node is also important; micro-metastases in which malignancy is only microscopic have a more favorable prognosis than macrometastases.
- In some cases, micrometastases may only be detected by special staining, and if malignancy is only detectable polymerase chain reaction (PCR), the prognosis is better.
- Macrometastases in which malignancy is clinically apparent (in some cases cancer completely replaces a node) have a far worse prognosis, and if nodes are matted or if there is extracapsular extension, the prognosis is still worse.
5-Year Survival
- Between 2004 and 2010, the 5-year relative survival of patients with melanoma was 92.9%.[1]
- When stratified by age, the 5-year relative survival of patients with melanoma was 92.7% and 88.2% for patients <65 and ≥ 65 years of age respectively.[1]
- When there is distant metastasis, the cancer is generally considered incurable. The five year survival rate is less than 10%.[4]
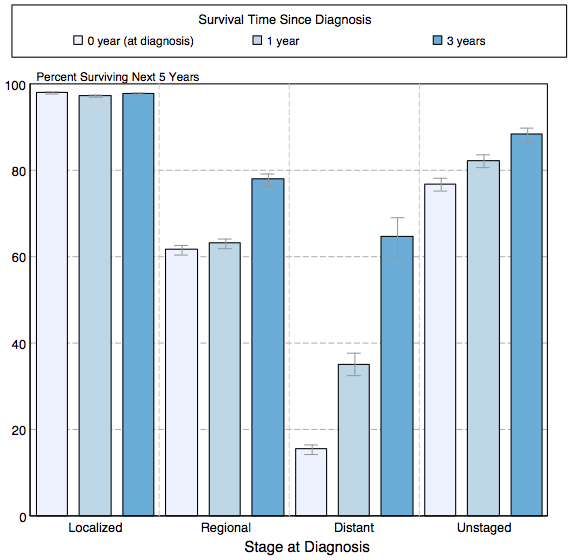
- The survival of patients with melanoma varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of melanoma:[1]
| Stage | 5-year relative survival (%), 2004-2010 |
|---|---|
| All stages | 91.3% |
| Localized | 98.1% |
| Regional | 62.6% |
| Distant | 16.1% |
| Unstaged | 78.4% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of melanoma by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[1]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
- ↑ Homsi J, Kashani-Sabet M, Messina J, Daud A (2005). "Cutaneous melanoma: prognostic factors". Cancer Control. 12 (4): 223–9. PMID 16258493.Full text (PDF)
- ↑ Homsi J, Kashani-Sabet M, Messina J, Daud A (2005). "Cutaneous melanoma: prognostic factors". Cancer Control. 12 (4): 223–9. PMID 16258493.Full text (PDF)
- ↑ Balch C, Buzaid A, Soong S, Atkins M, Cascinelli N, Coit D, Fleming I, Gershenwald J, Houghton A, Kirkwood J, McMasters K, Mihm M, Morton D, Reintgen D, Ross M, Sober A, Thompson J, Thompson J (2001). "Final version of the American Joint Committee on Cancer staging system for cutaneous melanoma". J Clin Oncol. 19 (16): 3635–48. PMID 11504745.Full text