Mastitis pathophysiology: Difference between revisions
Megan Merlo (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (23 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Most clinically significant cases of non-puerperal mastitis start as [[inflammation]] of the ductal and lobular system | Most clinically significant cases of non-puerperal mastitis start as [[inflammation]] of the ductal and [[lobular]] system and possibly the immediate surrounding [[tissue]]. Development of non-puerperal mastitis is the result of secretory [[stasis]] whereas puerperal mastitis occurs when [[bacteria]], often from the patient's [[skin]] or the baby's [[mouth]]/[[nostrils]],<ref>{{cite journal | title=A case-control study of mastitis: nasal carriage of ''Staphylococcus aureus'' | author=Amir LH, Garland SM, Lumley J. | journal=BMC Family Practice. | year=2006 | volume=7 | pages=57 | doi=10.1186/1471-2296-7-57}}</ref> enters a [[milk]] [[duct]] through a crack in the [[nipple]]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Anatomy of the breast=== | |||
The images below show a general overview of [[breast]] [[anatomy]]. | |||
[[Image:Breast.png|thumb|center|Cross-section of the breast - By Original author: Patrick J. Lynch. Reworked by Morgoth666 to add numbered legend arrows. - Patrick J. Lynch, medical illustrator, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=2676813]] | |||
1) Chest wall <br>2) Pectoralis muscles <br>3) Lobules <br>4) Nipple <br>5) Areola <br>6) Milk duct <br>7) Fatty tissue <br>8) Skin | |||
'''Surface anatomy of the breast''' | |||
[[Image:Breast1.jpg|thumb|center|Surface anatomy of the breast - By Original: Ralf RoletschekDerivative: علاء نجار - Derivative from this file, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=46044299]] | |||
===Pathogenesis=== | |||
====Non-puerperal Mastitis==== | |||
[[ | Most clinically significant cases of non-puerperal mastitis start as [[inflammation]] of the ductal and [[lobular]] system and possibly the immediate surrounding [[tissue]]. | ||
Development of non-puerperal mastitis is the result of secretory [[stasis]] in about 80% of cases. The retained [[secretions]] can get infected or lead to [[inflammation]] by causing mechanical [[injury]] leading to leakage of the [[lactiferous duct|lactiferous ducts]]. [[Autoimmune]] reaction to the [[secretion|secretions]] may also be a factor. | |||
====Puerperal Mastitis==== | |||
=== | Development of puerperal mastitis occurs when [[bacteria]], often from patients [[skin]] or the baby's [[mouth]]/[[nostrils]],<ref>{{cite journal | title=A case-control study of mastitis: nasal carriage of ''Staphylococcus aureus'' | author=Amir LH, Garland SM, Lumley J. | journal=BMC Family Practice. | year=2006 | volume=7 | pages=57 | doi=10.1186/1471-2296-7-57 }}</ref> enters a [[milk]] [[duct]] through a crack in the [[nipple]]. | ||
Several mechanisms, listed below, are thought to lead to the pathogenesis of mastitis: | |||
* Secretory disease or [[galactorrhea]] | |||
* Changes in [[permeability]] of [[lactiferous duct]]s (retention syndrome) | |||
* Blockage of [[lactiferous duct]]s, for example duct plugging caused by [[squamous metaplasia]] of [[lactiferous duct]]s | |||
* [[Trauma]] or [[injury]] | |||
* Mechanical irritation caused by [[retention syndrome]] or [[Fibrocystic Disease|fibrocystic]] condition | |||
* [[Infection]] | |||
* [[Autoimmune]] reaction to [[luminal]] [[fluid]] | |||
Approximately a quarter of patients may be [[hyperprolactinemia|hyperprolactinemic]]. There has been a strong association with [[fibrocystic breast disease|fibrocystic condition]] and [[thyroid]] conditions. Up to 50% of patients may experience transient [[hyperprolactinemia]] possibly caused by [[inflammation]] or treatment and a significant number of patients may have abnormally high [[prolactin]] reserve.<ref name="pmid2918655">{{cite journal| author=Peters F, Schuth W| title=Hyperprolactinemia and nonpuerperal mastitis (duct ectasia). | journal=JAMA | year= 1989 | volume= 261 | issue= 11 | pages= 1618-20 | pmid=2918655 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2918655}}</ref><ref name="pmid26179543">{{cite journal| author=Kutsuna S, Mezaki K, Nagamatsu M, Kunimatsu J, Yamamoto K, Fujiya Y et al.| title=Two Cases of Granulomatous Mastitis Caused by Corynebacterium kroppenstedtii Infection in Nulliparous Young Women with Hyperprolactinemia. | journal=Intern Med | year= 2015 | volume= 54 | issue= 14 | pages= 1815-8 | pmid=26179543 | doi=10.2169/internalmedicine.54.4254 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26179543}}</ref> | |||
[[TSH]], [[prolactin]], and [[IGF-1]] are important systemic factors in [[galactopoiesis]]. The significance of these factors in secretory [[disease]] is not well documented but it has been asserted that the mechanisms of secretory disease and [[galactopoiesis]] are closely related. | |||
[[Alveolar]] and ductal [[epithelia]] [[permeability]] is mostly controlled by [[tight junction]] regulation and is closely linked to [[galactopoiesis]] and secretory disease. The [[tight junctions]] are regulated by a multitude of systemic ([[prolactin]], [[progesterone]], [[glucocorticoid]]s) and local (intramammary pressure, [[TGF-beta]], [[osmotic]] balance) factors. | |||
[[Acromegaly]] may present with symptoms of non-puerperal mastitis. | |||
===Microscopic pathology=== | |||
[[Histopathology]] of [[granulomatous]] mastitis shows characteristic distribution of [[granulomatous]] [[inflammation]] which remains the gold standard for diagnosis.<ref name="pmid20030652">{{cite journal| author=Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K| title=Granulomatous mastitis: clinical, pathological features, and management. | journal=Breast J | year= 2010 | volume= 16 | issue= 2 | pages= 176-82 | pmid=20030652 | doi=10.1111/j.1524-4741.2009.00879.x | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20030652}}</ref> | |||
Histologically, [[lupus]] mastitis is seen as [[lymphocytic]] [[lobular]] [[panniculitis]] and [[hyaline]] [[sclerosis]] of the [[adipose tissue]]. This histologic finding is required to make an accurate diagnosis.<ref name="pmid19098467">{{cite journal| author=Summers TA, Lehman MB, Barner R, Royer MC| title=Lupus mastitis: a clinicopathologic review and addition of a case. | journal=Adv Anat Pathol | year= 2009 | volume= 16 | issue= 1 | pages= 56-61 | pmid=19098467 | doi=10.1097/PAP.0b013e3181915ff7 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19098467}}</ref> | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WS}} | |||
{{WH}} | |||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
[[Category:Needs overview]] | |||
[[Category:Emergency mdicine]] | |||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
[[Category: | [[Category:Gynecology]] | ||
[[Category: | [[Category:Surgery]] | ||
Latest revision as of 22:39, 29 July 2020
|
Mastitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mastitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Mastitis pathophysiology |
|
Risk calculators and risk factors for Mastitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Prince Tano Djan, BSc, MBChB [2]
Overview
Most clinically significant cases of non-puerperal mastitis start as inflammation of the ductal and lobular system and possibly the immediate surrounding tissue. Development of non-puerperal mastitis is the result of secretory stasis whereas puerperal mastitis occurs when bacteria, often from the patient's skin or the baby's mouth/nostrils,[1] enters a milk duct through a crack in the nipple.
Pathophysiology
Anatomy of the breast
The images below show a general overview of breast anatomy.
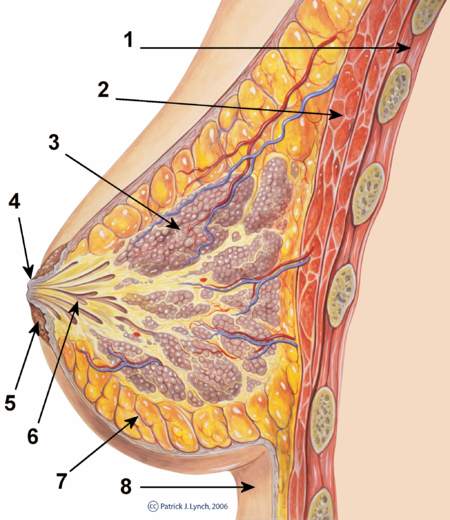
1) Chest wall
2) Pectoralis muscles
3) Lobules
4) Nipple
5) Areola
6) Milk duct
7) Fatty tissue
8) Skin
Surface anatomy of the breast
Pathogenesis
Non-puerperal Mastitis
Most clinically significant cases of non-puerperal mastitis start as inflammation of the ductal and lobular system and possibly the immediate surrounding tissue.
Development of non-puerperal mastitis is the result of secretory stasis in about 80% of cases. The retained secretions can get infected or lead to inflammation by causing mechanical injury leading to leakage of the lactiferous ducts. Autoimmune reaction to the secretions may also be a factor.
Puerperal Mastitis
Development of puerperal mastitis occurs when bacteria, often from patients skin or the baby's mouth/nostrils,[2] enters a milk duct through a crack in the nipple.
Several mechanisms, listed below, are thought to lead to the pathogenesis of mastitis:
- Secretory disease or galactorrhea
- Changes in permeability of lactiferous ducts (retention syndrome)
- Blockage of lactiferous ducts, for example duct plugging caused by squamous metaplasia of lactiferous ducts
- Trauma or injury
- Mechanical irritation caused by retention syndrome or fibrocystic condition
- Infection
- Autoimmune reaction to luminal fluid
Approximately a quarter of patients may be hyperprolactinemic. There has been a strong association with fibrocystic condition and thyroid conditions. Up to 50% of patients may experience transient hyperprolactinemia possibly caused by inflammation or treatment and a significant number of patients may have abnormally high prolactin reserve.[3][4]
TSH, prolactin, and IGF-1 are important systemic factors in galactopoiesis. The significance of these factors in secretory disease is not well documented but it has been asserted that the mechanisms of secretory disease and galactopoiesis are closely related.
Alveolar and ductal epithelia permeability is mostly controlled by tight junction regulation and is closely linked to galactopoiesis and secretory disease. The tight junctions are regulated by a multitude of systemic (prolactin, progesterone, glucocorticoids) and local (intramammary pressure, TGF-beta, osmotic balance) factors.
Acromegaly may present with symptoms of non-puerperal mastitis.
Microscopic pathology
Histopathology of granulomatous mastitis shows characteristic distribution of granulomatous inflammation which remains the gold standard for diagnosis.[5]
Histologically, lupus mastitis is seen as lymphocytic lobular panniculitis and hyaline sclerosis of the adipose tissue. This histologic finding is required to make an accurate diagnosis.[6]
References
- ↑ Amir LH, Garland SM, Lumley J. (2006). "A case-control study of mastitis: nasal carriage of Staphylococcus aureus". BMC Family Practice. 7: 57. doi:10.1186/1471-2296-7-57.
- ↑ Amir LH, Garland SM, Lumley J. (2006). "A case-control study of mastitis: nasal carriage of Staphylococcus aureus". BMC Family Practice. 7: 57. doi:10.1186/1471-2296-7-57.
- ↑ Peters F, Schuth W (1989). "Hyperprolactinemia and nonpuerperal mastitis (duct ectasia)". JAMA. 261 (11): 1618–20. PMID 2918655.
- ↑ Kutsuna S, Mezaki K, Nagamatsu M, Kunimatsu J, Yamamoto K, Fujiya Y; et al. (2015). "Two Cases of Granulomatous Mastitis Caused by Corynebacterium kroppenstedtii Infection in Nulliparous Young Women with Hyperprolactinemia". Intern Med. 54 (14): 1815–8. doi:10.2169/internalmedicine.54.4254. PMID 26179543.
- ↑ Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K (2010). "Granulomatous mastitis: clinical, pathological features, and management". Breast J. 16 (2): 176–82. doi:10.1111/j.1524-4741.2009.00879.x. PMID 20030652.
- ↑ Summers TA, Lehman MB, Barner R, Royer MC (2009). "Lupus mastitis: a clinicopathologic review and addition of a case". Adv Anat Pathol. 16 (1): 56–61. doi:10.1097/PAP.0b013e3181915ff7. PMID 19098467.