Gonadoblastoma pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{Sahar}} | {{CMG}}; {{AE}} {{Sahar}} | ||
==Overview== | ==Overview== | ||
The exact [[pathogenesis]] of gonadoblastoma is not fully understood. Gonadal development starts at 5 weeks of [[gestation]] and continues according to [[sex chromosomes]]. Any defects in this complicated process leads to defective gonadal development and [[gonadal dysgenesis]] and subsequently, it may be converted to gonadoblastoma in 20% to 30% of the cases. | The exact [[pathogenesis]] of gonadoblastoma is not fully understood. [[Gonadal]] development starts at 5 weeks of [[gestation]] and continues according to [[sex chromosomes]]. Any [[defects]] in this complicated process leads to defective [[gonadal]] development and [[gonadal dysgenesis]] and subsequently, it may be converted to gonadoblastoma in 20% to 30% of the cases. | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Physiology=== | ===Physiology=== | ||
Gonadal development starts at 5 weeks of [[gestation]] and continues according to [[sex chromosomes]]. Any defects in this complicated process lead to defective gonadal development and [[gonadal dysgenesis]].<ref>{{cite book | last = Carcangiu | first = M. L. | title = WHO Classification of Tumours of Female Reproductive Organs | publisher = International Agency for Research on Cancer | location = Lyon | year = 2014 | isbn = 978-9283224358 }}</ref><ref name="pmid16608895">{{cite journal |vauthors=Cools M, Stoop H, Kersemaekers AM, Drop SL, Wolffenbuttel KP, Bourguignon JP, Slowikowska-Hilczer J, Kula K, Faradz SM, Oosterhuis JW, Looijenga LH |title=Gonadoblastoma arising in undifferentiated gonadal tissue within dysgenetic gonads |journal=J. Clin. Endocrinol. Metab. |volume=91 |issue=6 |pages=2404–13 |date=June 2006 |pmid=16608895 |doi=10.1210/jc.2005-2554 |url=}}</ref> | [[Gonad|Gonadal]] development starts at 5 weeks of [[gestation]] and continues according to [[sex chromosomes]]. Any defects in this complicated process lead to defective [[gonadal]] development and [[gonadal dysgenesis]].<ref>{{cite book | last = Carcangiu | first = M. L. | title = WHO Classification of Tumours of Female Reproductive Organs | publisher = International Agency for Research on Cancer | location = Lyon | year = 2014 | isbn = 978-9283224358 }}</ref><ref name="pmid16608895">{{cite journal |vauthors=Cools M, Stoop H, Kersemaekers AM, Drop SL, Wolffenbuttel KP, Bourguignon JP, Slowikowska-Hilczer J, Kula K, Faradz SM, Oosterhuis JW, Looijenga LH |title=Gonadoblastoma arising in undifferentiated gonadal tissue within dysgenetic gonads |journal=J. Clin. Endocrinol. Metab. |volume=91 |issue=6 |pages=2404–13 |date=June 2006 |pmid=16608895 |doi=10.1210/jc.2005-2554 |url=}}</ref> | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
| Line 14: | Line 14: | ||
*The GBY gene locus, localized near the [[centromere]] of the [[Y chromosome]], is hypothesized to be the culprit [[gene]] [[locus]] in the [[pathogenesis]] of gonadoblastoma. | *The GBY gene locus, localized near the [[centromere]] of the [[Y chromosome]], is hypothesized to be the culprit [[gene]] [[locus]] in the [[pathogenesis]] of gonadoblastoma. | ||
*TSPY [[gene]], one of the genes belonging to GBY [[locus]], is observed to be over-expressed in the gonadoblastoma and other [[germ cell tumors]], although its exact role is still unclear. | *TSPY [[gene]], one of the genes belonging to GBY [[locus]], is observed to be over-expressed in the gonadoblastoma and other [[germ cell tumors]], although its exact role is still unclear. | ||
*There are case reports of genotypically normal women individuals with gonadoblastoma that suggests the existence of other mechanisms involving in the [[pathogenesis]] of gonadoblastoma.<ref name="pmid3809670">{{cite journal |vauthors=Bousquet G, Argenson C, Godeneche JL, Cisterne JP, Gazielly DF, Girardin P, Debiesse JL |title=[Recovery after aseptic loosening of cemented total hip arthroplasties with Bousquet's cementless prosthesis. Apropos of 136 cases] |language=French |journal=Rev Chir Orthop Reparatrice Appar Mot |volume=72 Suppl 2 |issue= |pages=70–4 |date=1986 |pmid=3809670 |doi= |url=}}</ref><ref name="pmid27721289">{{cite journal |vauthors=Kulkarni MM, Sinai Khandeparkar SG, Joshi AR, Bhayekar PV |title=Unilateral gonadoblastoma with dysgerminoma in normal fertile woman having a child: Extremely rare occurrence with characteristic immunohistomorphology |journal=Indian J Pathol Microbiol |volume=59 |issue=4 |pages=527–529 |date=2016 |pmid=27721289 |doi=10.4103/0377-4929.191815 |url=}}</ref> | *There are case reports of [[Genotype|genotypically]] normal women individuals with gonadoblastoma that suggests the existence of other mechanisms involving in the [[pathogenesis]] of gonadoblastoma.<ref name="pmid3809670">{{cite journal |vauthors=Bousquet G, Argenson C, Godeneche JL, Cisterne JP, Gazielly DF, Girardin P, Debiesse JL |title=[Recovery after aseptic loosening of cemented total hip arthroplasties with Bousquet's cementless prosthesis. Apropos of 136 cases] |language=French |journal=Rev Chir Orthop Reparatrice Appar Mot |volume=72 Suppl 2 |issue= |pages=70–4 |date=1986 |pmid=3809670 |doi= |url=}}</ref><ref name="pmid27721289">{{cite journal |vauthors=Kulkarni MM, Sinai Khandeparkar SG, Joshi AR, Bhayekar PV |title=Unilateral gonadoblastoma with dysgerminoma in normal fertile woman having a child: Extremely rare occurrence with characteristic immunohistomorphology |journal=Indian J Pathol Microbiol |volume=59 |issue=4 |pages=527–529 |date=2016 |pmid=27721289 |doi=10.4103/0377-4929.191815 |url=}}</ref> | ||
*It is hypothesized that the genotypically normal female individuals may have the TSPY putative [[gene]] on their [[X chromosomes]] or [[autosomes]].<ref name="pmid27721289">{{cite journal |vauthors=Kulkarni MM, Sinai Khandeparkar SG, Joshi AR, Bhayekar PV |title=Unilateral gonadoblastoma with dysgerminoma in normal fertile woman having a child: Extremely rare occurrence with characteristic immunohistomorphology |journal=Indian J Pathol Microbiol |volume=59 |issue=4 |pages=527–529 |date=2016 |pmid=27721289 |doi=10.4103/0377-4929.191815 |url=}}</ref> | *It is hypothesized that the [[Genotype|genotypically]] normal [[female]] individuals may have the TSPY putative [[gene]] on their [[X chromosomes]] or [[autosomes]].<ref name="pmid27721289">{{cite journal |vauthors=Kulkarni MM, Sinai Khandeparkar SG, Joshi AR, Bhayekar PV |title=Unilateral gonadoblastoma with dysgerminoma in normal fertile woman having a child: Extremely rare occurrence with characteristic immunohistomorphology |journal=Indian J Pathol Microbiol |volume=59 |issue=4 |pages=527–529 |date=2016 |pmid=27721289 |doi=10.4103/0377-4929.191815 |url=}}</ref> | ||
==Genetics== | ==Genetics== | ||
Genes involved in the [[pathogenesis]] of gonadoblastoma include:<ref name="pmid8533770">{{cite journal |vauthors=Tsuchiya K, Reijo R, Page DC, Disteche CM |title=Gonadoblastoma: molecular definition of the susceptibility region on the Y chromosome |journal=Am. J. Hum. Genet. |volume=57 |issue=6 |pages=1400–7 |date=December 1995 |pmid=8533770 |pmc=1801429 |doi= |url=}}</ref> | [[Genes]] involved in the [[pathogenesis]] of gonadoblastoma include:<ref name="pmid8533770">{{cite journal |vauthors=Tsuchiya K, Reijo R, Page DC, Disteche CM |title=Gonadoblastoma: molecular definition of the susceptibility region on the Y chromosome |journal=Am. J. Hum. Genet. |volume=57 |issue=6 |pages=1400–7 |date=December 1995 |pmid=8533770 |pmc=1801429 |doi= |url=}}</ref> | ||
*TSPY | *TSPY | ||
| Line 45: | Line 45: | ||
*Another kind of [[stromal cells]] ([[Leydig cell|Leydig cells]] or [[lutein]]-like cells) may also exist, but their presence is not essential for the [[diagnosis]]. They tend to be present greatly after [[puberty]]. | *Another kind of [[stromal cells]] ([[Leydig cell|Leydig cells]] or [[lutein]]-like cells) may also exist, but their presence is not essential for the [[diagnosis]]. They tend to be present greatly after [[puberty]]. | ||
The two essential type of cells forms a nest-like space in which, immature [[germ cells]] surrounded by sex-cord stromal cells. This nested arrangement is characteristic of gonadoblastoma. | The two essential type of cells forms a nest-like space in which, immature [[germ cells]] surrounded by sex-cord stromal cells. This nested arrangement is characteristic of gonadoblastoma. | ||
*The nest is encircled by a [[basement membrane]] which can be [[Hyaline|hyalin]]<nowiki/>ized or even calcified. | *The nest is encircled by a [[basement membrane]] which can be [[Hyaline|hyalin]]<nowiki/>[[Hyaline|ized]] or even calcified. | ||
*[[Calcification]] can be focal or extensive. | *[[Calcification]] can be focal or extensive. | ||
* Focal [[calcification]] is found in more than 80% of the individuals. | * Focal [[calcification]] is found in more than 80% of the individuals. | ||
| Line 52: | Line 52: | ||
*Classical form as described above. | *Classical form as described above. | ||
*Burnt-out form, in which the cells regress and the remnant is calcified and forms a mulberry-shaped [[calcification]]. | *Burnt-out form, in which the cells regress and the remnant is calcified and forms a mulberry-shaped [[calcification]]. | ||
*Dissecting form, which has an infiltrative and cord like pattern rather than a nested arrangement. The clinical relevance of this [[pathological]] feature is that, it should be differentiated from [[germinoma]].<ref name="KaoIdrees2016">{{cite journal|last1=Kao|first1=Chia-Sui|last2=Idrees|first2=Muhammad T.|last3=Young|first3=Robert H.|last4=Ulbright|first4=Thomas M.|title=“Dissecting Gonadoblastoma” of Scully|journal=The American Journal of Surgical Pathology|volume=40|issue=10|year=2016|pages=1417–1423|issn=0147-5185|doi=10.1097/PAS.0000000000000704}}</ref> | *Dissecting form, which has an [[Infiltration (medical)|infiltrative]] and cord like pattern rather than a nested arrangement. The [[Clinical|clinical relevance]] of this [[pathological]] feature is that, it should be differentiated from [[germinoma]].<ref name="KaoIdrees2016">{{cite journal|last1=Kao|first1=Chia-Sui|last2=Idrees|first2=Muhammad T.|last3=Young|first3=Robert H.|last4=Ulbright|first4=Thomas M.|title=“Dissecting Gonadoblastoma” of Scully|journal=The American Journal of Surgical Pathology|volume=40|issue=10|year=2016|pages=1417–1423|issn=0147-5185|doi=10.1097/PAS.0000000000000704}}</ref> | ||
===Immunohistochemistry=== | ===Immunohistochemistry=== | ||
Gonadoblastoma has no specific laboratory feature, however, some immunohistochemistry staining can be positive including:<ref name="978-1-4557-4858-7">{{cite book | last = Sperling | first = M | title = Pediatric endocrinology | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2014 | isbn = 978-1-4557-4858-7 }}</ref><ref name="KaoUlbright2014">{{cite journal|last1=Kao|first1=Chia-Sui|last2=Ulbright|first2=Thomas M|last3=Idrees|first3=Muhammad T|title=Gonadoblastoma: an immunohistochemical study and comparison to Sertoli cell nodule with intratubular germ cell neoplasia, with pathogenetic implications|journal=Histopathology|volume=65|issue=6|year=2014|pages=861–867|issn=03090167|doi=10.1111/his.12444}}</ref> | Gonadoblastoma has no specific [[laboratory]] feature, however, some [[immunohistochemistry]] [[staining]] can be positive including:<ref name="978-1-4557-4858-7">{{cite book | last = Sperling | first = M | title = Pediatric endocrinology | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2014 | isbn = 978-1-4557-4858-7 }}</ref><ref name="KaoUlbright2014">{{cite journal|last1=Kao|first1=Chia-Sui|last2=Ulbright|first2=Thomas M|last3=Idrees|first3=Muhammad T|title=Gonadoblastoma: an immunohistochemical study and comparison to Sertoli cell nodule with intratubular germ cell neoplasia, with pathogenetic implications|journal=Histopathology|volume=65|issue=6|year=2014|pages=861–867|issn=03090167|doi=10.1111/his.12444}}</ref> | ||
*TSPY | *TSPY | ||
Revision as of 15:26, 20 February 2019
|
Gonadoblastoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Gonadoblastoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Gonadoblastoma pathophysiology |
|
Risk calculators and risk factors for Gonadoblastoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sahar Memar Montazerin, M.D.[2]
Overview
The exact pathogenesis of gonadoblastoma is not fully understood. Gonadal development starts at 5 weeks of gestation and continues according to sex chromosomes. Any defects in this complicated process leads to defective gonadal development and gonadal dysgenesis and subsequently, it may be converted to gonadoblastoma in 20% to 30% of the cases.
Pathophysiology
Physiology
Gonadal development starts at 5 weeks of gestation and continues according to sex chromosomes. Any defects in this complicated process lead to defective gonadal development and gonadal dysgenesis.[1][2]
Pathogenesis
- The exact pathogenesis of gonadoblastoma is not completely understood.[3]
- Gonadoblastoma develop almost exclusively in dysgenetic gonads containing the Y chromosomal contents.
- The GBY gene locus, localized near the centromere of the Y chromosome, is hypothesized to be the culprit gene locus in the pathogenesis of gonadoblastoma.
- TSPY gene, one of the genes belonging to GBY locus, is observed to be over-expressed in the gonadoblastoma and other germ cell tumors, although its exact role is still unclear.
- There are case reports of genotypically normal women individuals with gonadoblastoma that suggests the existence of other mechanisms involving in the pathogenesis of gonadoblastoma.[4][5]
- It is hypothesized that the genotypically normal female individuals may have the TSPY putative gene on their X chromosomes or autosomes.[5]
Genetics
Genes involved in the pathogenesis of gonadoblastoma include:[6]
- TSPY
Associated Conditions
The following disorders are associated with the development of gonadoblastoma:
- XY gonadal dysgenesis[7]
- Frasier syndrome[8]
- WAGR syndrome[9]
- Swyer syndrome[10]
- 9p partial monosomy[11]
Gross Pathology
- Gross pathology of tumor greatly depends on the degree of germ cells overgrowth and calcification.[12]
- The tumor is firm and cartilaginous with a yellow to a brown-grey color.
- It may be calcified partly or almost completely.
- It may be very large, especially when accompanied by a dysgerminoma.
- Sometimes, it is hardly detectable in gross examination.
Microscopic Pathology
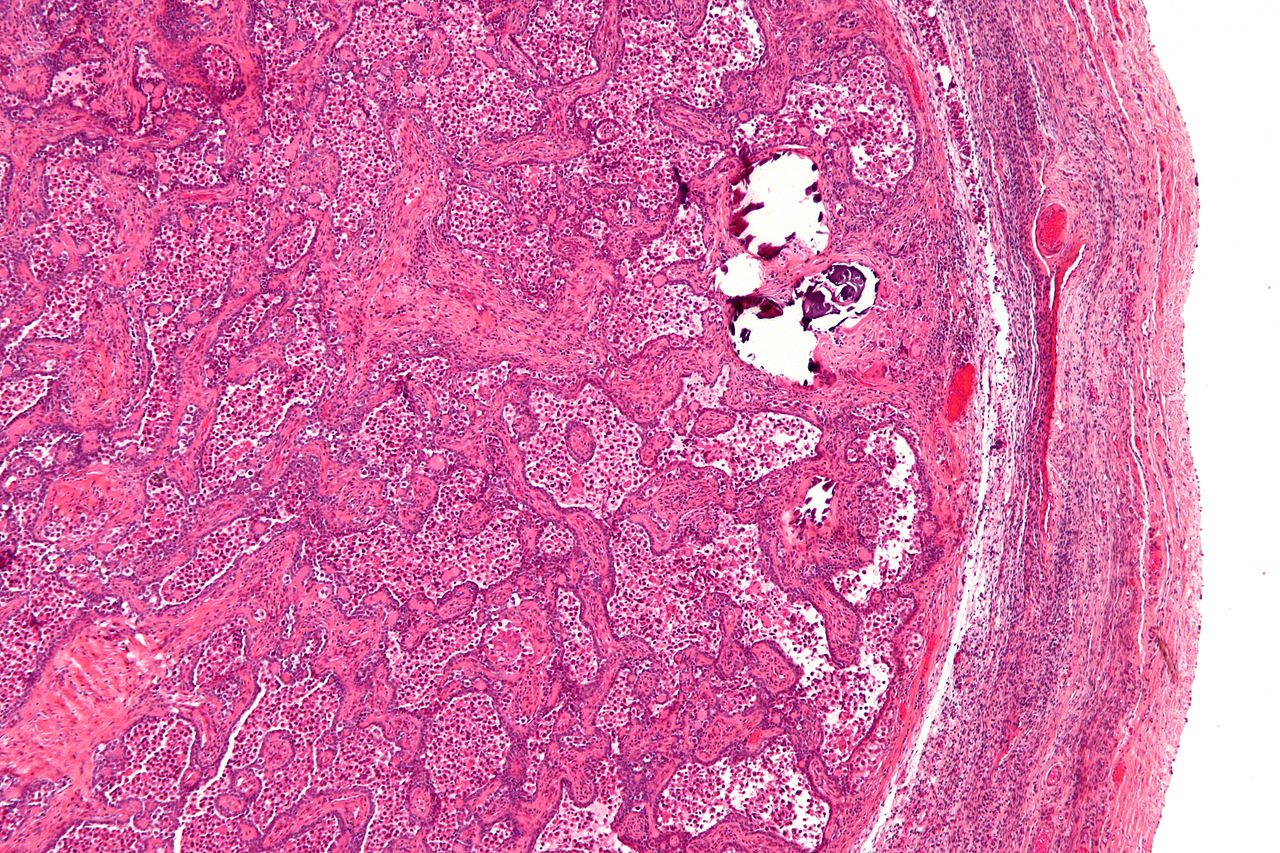 |
Gonadoblastoma is formed from two different types of cells:[13]
- Larger cells resembling immature germ cells with varied degrees of atypia must be differentiated from the simultaneous invasive germ cell tumor.
- Smaller cells resembling the sex-cord stroma (granulosa or sertoli-like cells).
- Another kind of stromal cells (Leydig cells or lutein-like cells) may also exist, but their presence is not essential for the diagnosis. They tend to be present greatly after puberty.
The two essential type of cells forms a nest-like space in which, immature germ cells surrounded by sex-cord stromal cells. This nested arrangement is characteristic of gonadoblastoma.
- The nest is encircled by a basement membrane which can be hyalinized or even calcified.
- Calcification can be focal or extensive.
- Focal calcification is found in more than 80% of the individuals.
- The nodular pattern of hyalinized basement membrane encircled by stromal cells can also be present.
Gonadoblastoma may be classified pathologically into three forms:[12][14]
- Classical form as described above.
- Burnt-out form, in which the cells regress and the remnant is calcified and forms a mulberry-shaped calcification.
- Dissecting form, which has an infiltrative and cord like pattern rather than a nested arrangement. The clinical relevance of this pathological feature is that, it should be differentiated from germinoma.[15]
Immunohistochemistry
Gonadoblastoma has no specific laboratory feature, however, some immunohistochemistry staining can be positive including:[16][17]
- TSPY
- OCT3/4
- FoxL
- SF-1
- Sox9
References
- ↑ Carcangiu, M. L. (2014). WHO Classification of Tumours of Female Reproductive Organs. Lyon: International Agency for Research on Cancer. ISBN 978-9283224358.
- ↑ Cools M, Stoop H, Kersemaekers AM, Drop SL, Wolffenbuttel KP, Bourguignon JP, Slowikowska-Hilczer J, Kula K, Faradz SM, Oosterhuis JW, Looijenga LH (June 2006). "Gonadoblastoma arising in undifferentiated gonadal tissue within dysgenetic gonads". J. Clin. Endocrinol. Metab. 91 (6): 2404–13. doi:10.1210/jc.2005-2554. PMID 16608895.
- ↑ Kido, Tatsuo; Lau, Yun-Fai Chris (2008). "The human Y-encoded testis-specific protein interacts functionally with eukaryotic translation elongation factor eEF1A, a putative oncoprotein". International Journal of Cancer. 123 (7): 1573–1585. doi:10.1002/ijc.23697. ISSN 0020-7136.
- ↑ Bousquet G, Argenson C, Godeneche JL, Cisterne JP, Gazielly DF, Girardin P, Debiesse JL (1986). "[Recovery after aseptic loosening of cemented total hip arthroplasties with Bousquet's cementless prosthesis. Apropos of 136 cases]". Rev Chir Orthop Reparatrice Appar Mot (in French). 72 Suppl 2: 70–4. PMID 3809670.
- ↑ 5.0 5.1 Kulkarni MM, Sinai Khandeparkar SG, Joshi AR, Bhayekar PV (2016). "Unilateral gonadoblastoma with dysgerminoma in normal fertile woman having a child: Extremely rare occurrence with characteristic immunohistomorphology". Indian J Pathol Microbiol. 59 (4): 527–529. doi:10.4103/0377-4929.191815. PMID 27721289.
- ↑ Tsuchiya K, Reijo R, Page DC, Disteche CM (December 1995). "Gonadoblastoma: molecular definition of the susceptibility region on the Y chromosome". Am. J. Hum. Genet. 57 (6): 1400–7. PMC 1801429. PMID 8533770.
- ↑ "Yen & Jaffe's Reproductive Endocrinology | ScienceDirect".
- ↑ "Emery and Rimoin's Principles and Practice of Medical Genetics and Genomics: Clinical Principles and Applications by Reed E. Pyeritz M.D., Ph.D., FACP, FACMG | | NOOK Book (eBook) | Barnes & Noble®".
- ↑ Patel, Payal R.; Pappas, John; Arva, Nicoleta C.; Franklin, Bonita; Brar, Preneet Cheema (2013). "Early presentation of bilateral gonadoblastomas in a Denys-Drash syndrome patient: a cautionary tale for prophylactic gonadectomy". Journal of Pediatric Endocrinology and Metabolism. 26 (9–10). doi:10.1515/jpem-2012-0409. ISSN 2191-0251.
- ↑ Milewicz, Tomasz; Mrozińska, Sandra; Szczepański, Wojciech; Białas, Magdalena; Kiałka, Marta; Doroszewska, Katarzyna; Kabzińska-Turek, Monika; Wojtyś, Andrzej; Ludwin, Artur; Chmura, Łukasz (2016). "Dysgerminoma and gonadoblastoma in the course of Swyer syndrome". Polish Journal of Pathology. 4: 411–414. doi:10.5114/pjp.2016.65876. ISSN 1233-9687.
- ↑ Quinonez, Shane C.; Park, John M.; Rabah, Raja; Owens, Kailey M.; Yashar, Beverly M.; Glover, Thomas W.; Keegan, Catherine E. (2013). "9p partial monosomy and disorders of sex development: Review and postulation of a pathogenetic mechanism". American Journal of Medical Genetics Part A. 161 (8): 1882–1896. doi:10.1002/ajmg.a.36018. ISSN 1552-4825.
- ↑ 12.0 12.1 Scully RE (1970). "Gonadoblastoma. A review of 74 cases". Cancer. 25 (6): 1340–56. PMID 4193741.
- ↑ Cools, Martine; Stoop, Hans; Kersemaekers, Anne-Marie F.; Drop, Stenvert L. S.; Wolffenbuttel, Katja P.; Bourguignon, Jean-Pierre; Slowikowska-Hilczer, Jolanta; Kula, Krzysztof; Faradz, Sultana M. H.; Oosterhuis, J. Wolter; Looijenga, Leendert H. J. (2006). "Gonadoblastoma Arising in Undifferentiated Gonadal Tissue within Dysgenetic Gonads". The Journal of Clinical Endocrinology & Metabolism. 91 (6): 2404–2413. doi:10.1210/jc.2005-2554. ISSN 0021-972X.
- ↑ Ulbright, Thomas M.; Young, Robert H. (2014). "Gonadoblastoma and selected other aspects of gonadal pathology in young patients with disorders of sex development". Seminars in Diagnostic Pathology. 31 (5): 427–440. doi:10.1053/j.semdp.2014.07.001. ISSN 0740-2570.
- ↑ Kao, Chia-Sui; Idrees, Muhammad T.; Young, Robert H.; Ulbright, Thomas M. (2016). ""Dissecting Gonadoblastoma" of Scully". The American Journal of Surgical Pathology. 40 (10): 1417–1423. doi:10.1097/PAS.0000000000000704. ISSN 0147-5185.
- ↑ Sperling, M (2014). Pediatric endocrinology. Philadelphia, PA: Elsevier/Saunders. ISBN 978-1-4557-4858-7.
- ↑ Kao, Chia-Sui; Ulbright, Thomas M; Idrees, Muhammad T (2014). "Gonadoblastoma: an immunohistochemical study and comparison to Sertoli cell nodule with intratubular germ cell neoplasia, with pathogenetic implications". Histopathology. 65 (6): 861–867. doi:10.1111/his.12444. ISSN 0309-0167.