Gestational trophoblastic neoplasia pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| (66 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Gestational trophoblastic neoplasia}} | ||
{{CMG}}{{AE}}{{ | {{CMG}}{{AE}}{{Sab}} | ||
==Overview== | |||
[[Pregnancy]] occurs when an [[Ovum|egg]], which is released from the [[ovary]] during [[ovulation]], is fertilized by a [[sperm]]. Human [[pregnancy]] takes approximately 40 weeks. Gestational trophoblastic neoplasia arises from the [[trophoblast]]ic tissue, which provides nutrients to the [[embryo]] and develops into a large part of the [[placenta]]. Invasive mole is basically a [[benign]] [[tumor]] which arises from the invasion of the [[myometrium]] of a [[hydatidiform mole]]. Choriocarcinoma is a [[malignant]] [[tumor]] of the [[Trophoblast|trophoblastic]] [[epithelium]]. Placental-site trophoblastic tumor (PSTT), a rare [[tumor]], arises from the [[implantation]] site of [[placenta]]. Epithelioid trophoblastic tumor (ETT) is basically a rare variant of placental-site trophoblastic tumor (PSTT) which arises from the [[malignant]] transformation of [[Chorion|chorionic]]-type intermediate [[Trophoblast|trophoblastic]] [[Cell (biology)|cells]]. Invasive mole is usually [[Ploidy|diploid]] but can also be [[Aneuploidy|aneuploid]] in [[karyotype|karyotype.]] Choriocarcinoma has an [[Aneuploidy|aneuploid]] [[karyotype]] and majority of the cases have a [[Y chromosome]]. | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Physiology=== | |||
The normal physiology of [[pregnancy]] can be understood as follows: | |||
* [[Pregnancy]] occurs when an [[Ovum|egg]], which is released from the [[ovary]] during [[ovulation]], is fertilized by a [[sperm]]. | |||
* ' | * After [[ejaculation]], the released [[sperm]] must spend some time in the female reproductive tract and undergo [[capacitation]], which is basically the acquisition of [[fertilization]] capability.<ref name="pmid14882325">{{cite journal |vauthors=CHANG MC |title=Fertilizing capacity of spermatozoa deposited into the fallopian tubes |journal=Nature |volume=168 |issue=4277 |pages=697–8 |date=October 1951 |pmid=14882325 |doi= |url=}}</ref><ref name="pmid14895481">{{cite journal |vauthors=AUSTIN CR |title=Observations on the penetration of the sperm in the mammalian egg |journal=Aust J Sci Res B |volume=4 |issue=4 |pages=581–96 |date=November 1951 |pmid=14895481 |doi= |url=}}</ref><ref name="pmid12993150">{{cite journal |vauthors=AUSTIN CR |title=The capacitation of the mammalian sperm |journal=Nature |volume=170 |issue=4321 |pages=326 |date=August 1952 |pmid=12993150 |doi= |url=}}</ref> | ||
*The [[sperm]] then penetrates the [[Ovum|egg]] after the acrosomal reaction and initiates the process of [[fertilization]] in the [[fallopian tube]].<ref>{{cite book | last = Moore | first = Keith | title = Essentials of human embryology | publisher = B.C. Decker C.V. Mosby Co. distributor | location = Toronto Philadelphia Saint Louis, Mo | year = 1988 | isbn = 9780941158978 }}</ref> | |||
*The [[sperm]] breaks through the [[Oocyte|oocyte's]] [[Cell membrane|plasma membrane]] and releases its [[Ploidy|haploid]] [[Cell nucleus|nucleus]] into the [[oocyte]].<ref>{{cite book | last = Moore | first = Keith | title = Essentials of human embryology | publisher = B.C. Decker C.V. Mosby Co. distributor | location = Toronto Philadelphia Saint Louis, Mo | year = 1988 | isbn = 9780941158978 }}</ref> | |||
* [[ | * Cortical reaction (changes in the [[oocyte]] [[Cell membrane|membrane]]) prevents any further penetration by another [[sperm]]. | ||
* Unification of the two [[Ploidy|haploid]] [[Cell nucleus|nuclei]] (one each from the [[sperm]] and [[Ovum|egg]]) marks the completion of [[Fertilization\|fertilization]], resulting in the formation of a [[Ploidy|diploid]] [[zygote]]. | |||
* | * The [[zygote]] undergoes multiple divisions called [[Cleavage (embryo)|cleavage]] before its migration to the [[uterus]].<ref name="pmid28698706">{{cite journal |vauthors=Miklavcic JJ, Flaman P |title=Personhood status of the human zygote, embryo, fetus |journal=Linacre Q |volume=84 |issue=2 |pages=130–144 |date=May 2017 |pmid=28698706 |pmc=5499222 |doi=10.1080/00243639.2017.1299896 |url=}}</ref> | ||
* Human [[pregnancy]] takes approximately 40 weeks. | |||
'''Placental Trophoblast and Pregnancy''' | |||
*[[Trophoblast]] (outer layer of the [[blastocyst]]) is composed of [[cytotrophoblast]], [[syncytiotrophoblast]], and intermediate [[trophoblast]].<ref>{{cite book | last = Moore | first = Keith | title = The developing human : clinically oriented embryology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 9780323313384 }}</ref> | |||
*[[Syncytiotrophoblast]] invades the [[Endometrium|endometrial]] stroma and produces [[Human chorionic gonadotropin|human chorionic gonadotropin (hCG)]].<ref>{{cite book | last = Moore | first = Keith | title = The developing human : clinically oriented embryology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 9780323313384 }}</ref> | |||
*[[Cytotrophoblast]] supplies the syncitium with [[Cell (biology)|cells]] and also forms the outpouchings that later become the [[chorionic villi]].<ref>{{cite book | last = Moore | first = Keith | title = The developing human : clinically oriented embryology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 9780323313384 }}</ref> | |||
*Intermediate [[trophoblast]] is situated in the [[Chorionic villi|chroionic villi]], the [[implantation]] site, and the [[Chorion|chorionic sac]].<ref>{{cite book | last = Moore | first = Keith | title = The developing human : clinically oriented embryology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 9780323313384 }}</ref> | |||
For more information on [[fertilization]], click [[Fertilization|here]].<br>For more information on [[pregnancy]], click [[Pregnancy|here]]. | |||
===Pathogenesis=== | |||
[[Pathogenesis]] of each sub-type of gestational trophoblastic neoplasia is explained as follows: | |||
====Invasive Mole==== | |||
*Invasive mole is basically a [[benign]] [[tumor]] which arises from the invasion of the [[myometrium]] of a [[hydatidiform mole]].<ref name="Lurain2010">{{cite journal|last1=Lurain|first1=John R.|title=Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole|journal=American Journal of Obstetrics and Gynecology|volume=203|issue=6|year=2010|pages=531–539|issn=00029378|doi=10.1016/j.ajog.2010.06.073}}</ref> | |||
*It may be preceded by a [[Hydatidiform mole|complete]] or [[Hydatidiform mole|partial molar pregnancy]] and it rarely [[Metastasis|metastasizes]].<ref>https://www.cancer.gov</ref><ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref><ref name="pmid27743739">{{cite journal |vauthors=Brown J, Naumann RW, Seckl MJ, Schink J |title=15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage |journal=Gynecol. Oncol. |volume=144 |issue=1 |pages=200–207 |date=January 2017 |pmid=27743739 |doi=10.1016/j.ygyno.2016.08.330 |url=}}</ref> | |||
*Invasive moles are more aggressive than [[Hydatidiform mole|complete]] or [[Hydatidiform mole|partial hydatidiform moles]].<ref>https://www.cancer.gov</ref> | |||
*Although rarely [[Metastasis|metastatic]], it can spread through the [[Blood|hematogenous]] route to the following organs: | |||
** [[Lung|Lungs]] (80% of the time)<ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref><ref name="pmid27743739">{{cite journal |vauthors=Brown J, Naumann RW, Seckl MJ, Schink J |title=15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage |journal=Gynecol. Oncol. |volume=144 |issue=1 |pages=200–207 |date=January 2017 |pmid=27743739 |doi=10.1016/j.ygyno.2016.08.330 |url=}}</ref><ref name="pmid23999759">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Fisher RA, Golfier F, Massuger L, Sessa C |title=Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up |journal=Ann. Oncol. |volume=24 Suppl 6 |issue= |pages=vi39–50 |date=October 2013 |pmid=23999759 |doi=10.1093/annonc/mdt345 |url=}}</ref> | |||
** [[Vagina]] (30%)<ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref><ref name="pmid27743739">{{cite journal |vauthors=Brown J, Naumann RW, Seckl MJ, Schink J |title=15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage |journal=Gynecol. Oncol. |volume=144 |issue=1 |pages=200–207 |date=January 2017 |pmid=27743739 |doi=10.1016/j.ygyno.2016.08.330 |url=}}</ref><ref name="pmid23999759">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Fisher RA, Golfier F, Massuger L, Sessa C |title=Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up |journal=Ann. Oncol. |volume=24 Suppl 6 |issue= |pages=vi39–50 |date=October 2013 |pmid=23999759 |doi=10.1093/annonc/mdt345 |url=}}</ref> | |||
** [[Pelvis]] (20%)<ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref><ref name="pmid27743739">{{cite journal |vauthors=Brown J, Naumann RW, Seckl MJ, Schink J |title=15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage |journal=Gynecol. Oncol. |volume=144 |issue=1 |pages=200–207 |date=January 2017 |pmid=27743739 |doi=10.1016/j.ygyno.2016.08.330 |url=}}</ref><ref name="pmid23999759">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Fisher RA, Golfier F, Massuger L, Sessa C |title=Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up |journal=Ann. Oncol. |volume=24 Suppl 6 |issue= |pages=vi39–50 |date=October 2013 |pmid=23999759 |doi=10.1093/annonc/mdt345 |url=}}</ref> | |||
** [[Liver]] (10%)<ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref><ref name="pmid27743739">{{cite journal |vauthors=Brown J, Naumann RW, Seckl MJ, Schink J |title=15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage |journal=Gynecol. Oncol. |volume=144 |issue=1 |pages=200–207 |date=January 2017 |pmid=27743739 |doi=10.1016/j.ygyno.2016.08.330 |url=}}</ref> | |||
** [[Brain]] (10%)<ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref><ref name="pmid27743739">{{cite journal |vauthors=Brown J, Naumann RW, Seckl MJ, Schink J |title=15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage |journal=Gynecol. Oncol. |volume=144 |issue=1 |pages=200–207 |date=January 2017 |pmid=27743739 |doi=10.1016/j.ygyno.2016.08.330 |url=}}</ref> | |||
** Other sites (< 5%)<ref name="pmid20673583">{{cite journal |vauthors=Seckl MJ, Sebire NJ, Berkowitz RS |title=Gestational trophoblastic disease |journal=Lancet |volume=376 |issue=9742 |pages=717–29 |date=August 2010 |pmid=20673583 |doi=10.1016/S0140-6736(10)60280-2 |url=}}</ref> | |||
====Choriocarcinoma==== | |||
*[[Choriocarcinoma]] is a [[malignant]] [[tumor]] of the [[Trophoblast|trophoblastic]] [[epithelium]].<ref>https://www.cancer.gov</ref> | |||
*[[Cytotrophoblast|Cytotrophoblastic]] [[Cell (biology)|cells]], functioning as [[Stem cell|stem cells]], can undergo [[malignant]] transformation.<ref name="pmid30571055">{{cite journal |vauthors=Bishop BN, Edemekong PF |title= |journal= |volume= |issue= |pages= |date= |pmid=30571055 |doi= |url=}}</ref> | |||
*After the [[malignant]] transformation, the [[Cell (biology)|cells]] can differentiate into intermediate [[trophoblast]] and [[syncytiotrophoblast]].<ref name="pmid18059230">{{cite journal |vauthors=Mao TL, Kurman RJ, Huang CC, Lin MC, Shih IeM |title=Immunohistochemistry of choriocarcinoma: an aid in differential diagnosis and in elucidating pathogenesis |journal=Am. J. Surg. Pathol. |volume=31 |issue=11 |pages=1726–32 |date=November 2007 |pmid=18059230 |doi=10.1097/PAS.0b013e318058a529 |url=}}</ref> | |||
*This mixture of [[Cell (biology)|cells]] can mimic normal development of a previllous [[blastocyst]].<ref name="pmid17613426">{{cite journal |vauthors=Shih IeM |title=Gestational trophoblastic neoplasia--pathogenesis and potential therapeutic targets |journal=Lancet Oncol. |volume=8 |issue=7 |pages=642–50 |date=July 2007 |pmid=17613426 |doi=10.1016/S1470-2045(07)70204-8 |url=}}</ref> | |||
*[[Choriocarcinoma]] can invade the [[Uterus|uterine]] [[Tissue (biology)|tissue]] and [[Circulatory system|vasculature]] and spread to distant sites such as [[Lung|lungs]], [[brain]], [[liver]], [[pelvis]], [[vagina]], [[spleen]], [[Intestine|intestines]], and [[kidney]].<ref>https://www.cancer.gov</ref> | |||
*[[Choriocarcinoma]] most commonly follows a [[Hydatidiform mole|molar pregnancy]], [[Miscarriage|spontaneous abortion]], or [[ectopic pregnancy]]. | |||
*Less commonly, choriocarcinoma can also follow a full-term [[pregnancy]]. | |||
====Placental-site Trophoblastic Tumor (PSTT)==== | |||
*Placental-site trophoblastic tumor (PSTT), a rare [[tumor]], arises from the [[implantation]] site of [[placenta]]. | |||
*It can resemble an amplified form of [[Syncytium|syncytial]] [[endometritis]].<ref>https://www.cancer.gov</ref> | |||
*The [[tumor]] represents [[malignant]] transformation of intermediate [[Trophoblast|trophoblastic]] [[Cell (biology)|cells]].<ref name="pmid12063871">{{cite journal |vauthors=Feltmate CM, Genest DR, Goldstein DP, Berkowitz RS |title=Advances in the understanding of placental site trophoblastic tumor |journal=J Reprod Med |volume=47 |issue=5 |pages=337–41 |date=May 2002 |pmid=12063871 |doi= |url=}}</ref> | |||
*It is associated with less [[vascular]] invasion, [[Bleeding|hemorrhage]], and [[necrosis]] compared to choriocarcinoma. | |||
*Placental-site trophoblastic tumor (PSTT) has a tendency for [[Lymphatic system|lymphatic]] [[metastasis]].<ref>https://www.cancer.gov</ref> | |||
*Because of the lower growth rate, the presentation of placental-site trophoblastic tumor (PSTT) can be delayed by months or even years.<ref>https://www.cancer.gov</ref> | |||
*Majority of the cases of placental-site trophoblastic tumor (PSTT) follow [[Pregnancy|non-molar pregnancies]].<ref name="pmid19552948">{{cite journal |vauthors=Schmid P, Nagai Y, Agarwal R, Hancock B, Savage PM, Sebire NJ, Lindsay I, Wells M, Fisher RA, Short D, Newlands ES, Wischnewsky MB, Seckl MJ |title=Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study |journal=Lancet |volume=374 |issue=9683 |pages=48–55 |date=July 2009 |pmid=19552948 |doi=10.1016/S0140-6736(09)60618-8 |url=}}</ref> | |||
*35% of placental-site trophoblastic tumors (PSTT) have distant [[Metastasis|metastases]] at the time of [[diagnosis]].<ref name="pmid12063871">{{cite journal |vauthors=Feltmate CM, Genest DR, Goldstein DP, Berkowitz RS |title=Advances in the understanding of placental site trophoblastic tumor |journal=J Reprod Med |volume=47 |issue=5 |pages=337–41 |date=May 2002 |pmid=12063871 |doi= |url=}}</ref><ref name="pmid19552948">{{cite journal |vauthors=Schmid P, Nagai Y, Agarwal R, Hancock B, Savage PM, Sebire NJ, Lindsay I, Wells M, Fisher RA, Short D, Newlands ES, Wischnewsky MB, Seckl MJ |title=Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study |journal=Lancet |volume=374 |issue=9683 |pages=48–55 |date=July 2009 |pmid=19552948 |doi=10.1016/S0140-6736(09)60618-8 |url=}}</ref> | |||
*Common sites of [[metastasis]] include the [[Lung|lungs]], [[pelvis]], and [[Lymph node|lymph nodes]]. | |||
====Epithelioid Trophoblastic Tumor (ETT)==== | |||
*Epithelioid trophoblastic tumor (ETT) is basically a rare variant of placental-site trophoblastic tumor (PSTT). | |||
*It arises from the [[malignant]] transformation of [[Chorion|chorionic]]-type intermediate [[Trophoblast|trophoblastic]] [[Cell (biology)|cells]].<ref name="pmid9808132">{{cite journal |vauthors=Shih IM, Kurman RJ |title=Epithelioid trophoblastic tumor: a neoplasm distinct from choriocarcinoma and placental site trophoblastic tumor simulating carcinoma |journal=Am. J. Surg. Pathol. |volume=22 |issue=11 |pages=1393–403 |date=November 1998 |pmid=9808132 |doi= |url=}}</ref> | |||
*Epithelioid trophoblastic tumor (ETT) can clinically present as [[benign]] or [[malignant]].<ref>https://www.cancer.gov</ref> | |||
*Majority of the cases of epithelioid trophoblastic tumors (ETT) present years after full-term [[Gestation|gestations]].<ref name="pmid9808132">{{cite journal |vauthors=Shih IM, Kurman RJ |title=Epithelioid trophoblastic tumor: a neoplasm distinct from choriocarcinoma and placental site trophoblastic tumor simulating carcinoma |journal=Am. J. Surg. Pathol. |volume=22 |issue=11 |pages=1393–403 |date=November 1998 |pmid=9808132 |doi= |url=}}</ref><ref name="pmid17149967">{{cite journal |vauthors=Allison KH, Love JE, Garcia RL |title=Epithelioid trophoblastic tumor: review of a rare neoplasm of the chorionic-type intermediate trophoblast |journal=Arch. Pathol. Lab. Med. |volume=130 |issue=12 |pages=1875–7 |date=December 2006 |pmid=17149967 |doi=10.1043/1543-2165(2006)130[1875:ETTROA]2.0.CO;2 |url=}}</ref> | |||
==Genetics== | |||
*Invasive mole is usually [[Ploidy|diploid]] but can also be [[Aneuploidy|aneuploid]] in [[karyotype|karyotype.]]<ref>http://www.cancer.gov</ref> | |||
*[[Choriocarcinoma]] has an [[Aneuploidy|aneuploid]] [[karyotype]] and majority of the cases have a [[Y chromosome]].<ref>http://www.cancer.gov</ref> | |||
*[[Mutation]] in the following [[Gene|genes]] has been associated with recurrent [[hydatidiform mole]], a precursor of and a [[risk factor]] for gestational trophoblastic neoplasia: | |||
** [[NLRP7|NLR family, pyrin domain-containing 7 (NLRP7)]]<ref name="pmid16462743">{{cite journal |vauthors=Murdoch S, Djuric U, Mazhar B, Seoud M, Khan R, Kuick R, Bagga R, Kircheisen R, Ao A, Ratti B, Hanash S, Rouleau GA, Slim R |title=Mutations in NALP7 cause recurrent hydatidiform moles and reproductive wastage in humans |journal=Nat. Genet. |volume=38 |issue=3 |pages=300–2 |date=March 2006 |pmid=16462743 |doi=10.1038/ng1740 |url=}}</ref><ref name="pmid21885028">{{cite journal |vauthors=Parry DA, Logan CV, Hayward BE, Shires M, Landolsi H, Diggle C, Carr I, Rittore C, Touitou I, Philibert L, Fisher RA, Fallahian M, Huntriss JD, Picton HM, Malik S, Taylor GR, Johnson CA, Bonthron DT, Sheridan EG |title=Mutations causing familial biparental hydatidiform mole implicate c6orf221 as a possible regulator of genomic imprinting in the human oocyte |journal=Am. J. Hum. Genet. |volume=89 |issue=3 |pages=451–8 |date=September 2011 |pmid=21885028 |pmc=3169823 |doi=10.1016/j.ajhg.2011.08.002 |url=}}</ref> | |||
** KHDC3-like protein, subcortical maternal complex member (KHDC3L)<ref name="pmid16462743">{{cite journal |vauthors=Murdoch S, Djuric U, Mazhar B, Seoud M, Khan R, Kuick R, Bagga R, Kircheisen R, Ao A, Ratti B, Hanash S, Rouleau GA, Slim R |title=Mutations in NALP7 cause recurrent hydatidiform moles and reproductive wastage in humans |journal=Nat. Genet. |volume=38 |issue=3 |pages=300–2 |date=March 2006 |pmid=16462743 |doi=10.1038/ng1740 |url=}}</ref><ref name="pmid21885028">{{cite journal |vauthors=Parry DA, Logan CV, Hayward BE, Shires M, Landolsi H, Diggle C, Carr I, Rittore C, Touitou I, Philibert L, Fisher RA, Fallahian M, Huntriss JD, Picton HM, Malik S, Taylor GR, Johnson CA, Bonthron DT, Sheridan EG |title=Mutations causing familial biparental hydatidiform mole implicate c6orf221 as a possible regulator of genomic imprinting in the human oocyte |journal=Am. J. Hum. Genet. |volume=89 |issue=3 |pages=451–8 |date=September 2011 |pmid=21885028 |pmc=3169823 |doi=10.1016/j.ajhg.2011.08.002 |url=}}</ref> | |||
== Associated Conditions == | |||
Conditions associated with gestational trophoblastic neoplasia include: | |||
*[[Hyperthyroidism]]<ref name="pmid26050078">{{cite journal |vauthors=von Welser SF, Grube M, Ortmann O |title=Invasive mole in a perimenopausal woman: a case report and systematic review |journal=Arch. Gynecol. Obstet. |volume=292 |issue=6 |pages=1193–9 |date=December 2015 |pmid=26050078 |doi=10.1007/s00404-015-3777-z |url=}}</ref> | |||
*[[Hypertension]]<ref name="pmid26050078">{{cite journal |vauthors=von Welser SF, Grube M, Ortmann O |title=Invasive mole in a perimenopausal woman: a case report and systematic review |journal=Arch. Gynecol. Obstet. |volume=292 |issue=6 |pages=1193–9 |date=December 2015 |pmid=26050078 |doi=10.1007/s00404-015-3777-z |url=}}</ref> | |||
*[[Mature cystic teratoma]]<ref name="pmid30116304">{{cite journal |vauthors=Simes BC, Mbanaso AA, Zapata CA, Okoroji CM |title=Hyperthyroidism in a complete molar pregnancy with a mature cystic ovarian teratoma |journal=Thyroid Res |volume=11 |issue= |pages=12 |date=2018 |pmid=30116304 |pmc=6086074 |doi=10.1186/s13044-018-0056-7 |url=}}</ref> | |||
*Normal [[pregnancy]]<ref name="pmid28800576">{{cite journal |vauthors=Lu D, Tang JJ, Zakashansky K, Berkowitz RS, Kalir T, Liu Y |title=Heterotopic Pregnancy Including Intrauterine Normal Gestation and Tubal Complete Hydatidiform Mole: A Case Report and Review of the Literature |journal=Int. J. Gynecol. Pathol. |volume=36 |issue=5 |pages=428–432 |date=September 2017 |pmid=28800576 |doi=10.1097/PGP.0000000000000347 |url=}}</ref> | |||
==Gross Pathology== | |||
[[Gross pathology|Gross pathological]] findings of the sub-types of gestational trophoblastic neoplasia are as follows: | |||
====Invasive mole==== | |||
*It appears as an erosive [[hemorrhagic]] [[lesion]] | |||
*Hydropic [[Villus|villi]] sticking out from the [[endometrium]] into the [[myometrium]] can also be visible | |||
====Choriocarcinoma==== | |||
*Bulky, destructive mass with [[Bleeding|hemorrhage]] and [[necrosis]]<ref name="OberEdgcomb1971">{{cite journal|last1=Ober|first1=William B.|last2=Edgcomb|first2=John H.|last3=Price|first3=Edward B.|title=THE PATHOLOGY OF CHORIOCARCINOMA|journal=Annals of the New York Academy of Sciences|volume=172|issue=10 Physiology a|year=1971|pages=299–426|issn=0077-8923|doi=10.1111/j.1749-6632.1971.tb34943.x}}</ref><ref name="SmithKohorn2005">{{cite journal|last1=Smith|first1=Harriet O.|last2=Kohorn|first2=Ernest|last3=Cole|first3=Laurence A.|title=Choriocarcinoma and Gestational Trophoblastic Disease|journal=Obstetrics and Gynecology Clinics of North America|volume=32|issue=4|year=2005|pages=661–684|issn=08898545|doi=10.1016/j.ogc.2005.08.001}}</ref> | |||
*Can be associated with deep [[Myometrium|myometrial]] invasion | |||
====Epithelioid Trophoblastic Tumor (ETT)==== | |||
*[[Cyst|Cystic]] or [[Nodule (medicine)|nodular]] [[hemorrhagic]] masses that can compress and infiltrate the structures around it<ref name="pmid9808132">{{cite journal |vauthors=Shih IM, Kurman RJ |title=Epithelioid trophoblastic tumor: a neoplasm distinct from choriocarcinoma and placental site trophoblastic tumor simulating carcinoma |journal=Am. J. Surg. Pathol. |volume=22 |issue=11 |pages=1393–403 |date=November 1998 |pmid=9808132 |doi= |url=}}</ref><ref name="pmid16258513">{{cite journal |vauthors=Fadare O, Parkash V, Carcangiu ML, Hui P |title=Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement |journal=Mod. Pathol. |volume=19 |issue=1 |pages=75–82 |date=January 2006 |pmid=16258513 |doi=10.1038/modpathol.3800485 |url=}}</ref><ref name="MeydanliKucukali2002">{{cite journal|last1=Meydanli|first1=Mutlu M.|last2=Kucukali|first2=Turkan|last3=Usubutun|first3=Alp|last4=Ataoglu|first4=Omur|last5=Kafkasli|first5=Ayse|title=Epithelioid Trophoblastic Tumor of the Endocervix: A Case Report|journal=Gynecologic Oncology|volume=87|issue=2|year=2002|pages=219–224|issn=00908258|doi=10.1006/gyno.2002.6820}}</ref> | |||
*Size of the [[tumor]] ranges from 0.5 - 5 cm.<ref name="pmid9808132">{{cite journal |vauthors=Shih IM, Kurman RJ |title=Epithelioid trophoblastic tumor: a neoplasm distinct from choriocarcinoma and placental site trophoblastic tumor simulating carcinoma |journal=Am. J. Surg. Pathol. |volume=22 |issue=11 |pages=1393–403 |date=November 1998 |pmid=9808132 |doi= |url=}}</ref><ref name="pmid17149967">{{cite journal |vauthors=Allison KH, Love JE, Garcia RL |title=Epithelioid trophoblastic tumor: review of a rare neoplasm of the chorionic-type intermediate trophoblast |journal=Arch. Pathol. Lab. Med. |volume=130 |issue=12 |pages=1875–7 |date=December 2006 |pmid=17149967 |doi=10.1043/1543-2165(2006)130[1875:ETTROA]2.0.CO;2 |url=}}</ref> | |||
*Cut surface can have a tan or white appearance with [[Bleeding|hemorrhage]] and [[necrosis]] | |||
*[[Ulcer|Ulceration]] can be present | |||
*[[Fistula]] formation is common | |||
====Placental-site Trophoblastic Tumor (PSTT)==== | |||
*It can appear as a [[Nodule (medicine)|nodular]], round, solid mass or varying size | |||
*[[Necrosis]] and [[Bleeding|hemorrhage]] is commonly seen<ref name="pmid6200262">{{cite journal |vauthors=Young RH, Scully RE |title=Placental-site trophoblastic tumor: current status |journal=Clin Obstet Gynecol |volume=27 |issue=1 |pages=248–58 |date=March 1984 |pmid=6200262 |doi= |url=}}</ref><ref name="BaergenRutgers2006">{{cite journal|last1=Baergen|first1=Rebecca N.|last2=Rutgers|first2=Joanne L.|last3=Young|first3=Robert H.|last4=Osann|first4=Kathryn|last5=Scully|first5=Robert E.|title=Placental site trophoblastic tumor: A study of 55 cases and review of the literature emphasizing factors of prognostic significance|journal=Gynecologic Oncology|volume=100|issue=3|year=2006|pages=511–520|issn=00908258|doi=10.1016/j.ygyno.2005.08.058}}</ref> | |||
*Can result in [[perforation]] and extend into the [[Broad ligament of the uterus|broad ligament]] and [[adnexa]]<ref name="pmid14501817">{{cite journal |vauthors=Baergen RN, Rutgers J, Young RH |title=Extrauterine lesions of intermediate trophoblast |journal=Int. J. Gynecol. Pathol. |volume=22 |issue=4 |pages=362–7 |date=October 2003 |pmid=14501817 |doi=10.1097/01.pgp.0000092132.88121.d1 |url=}}</ref> | |||
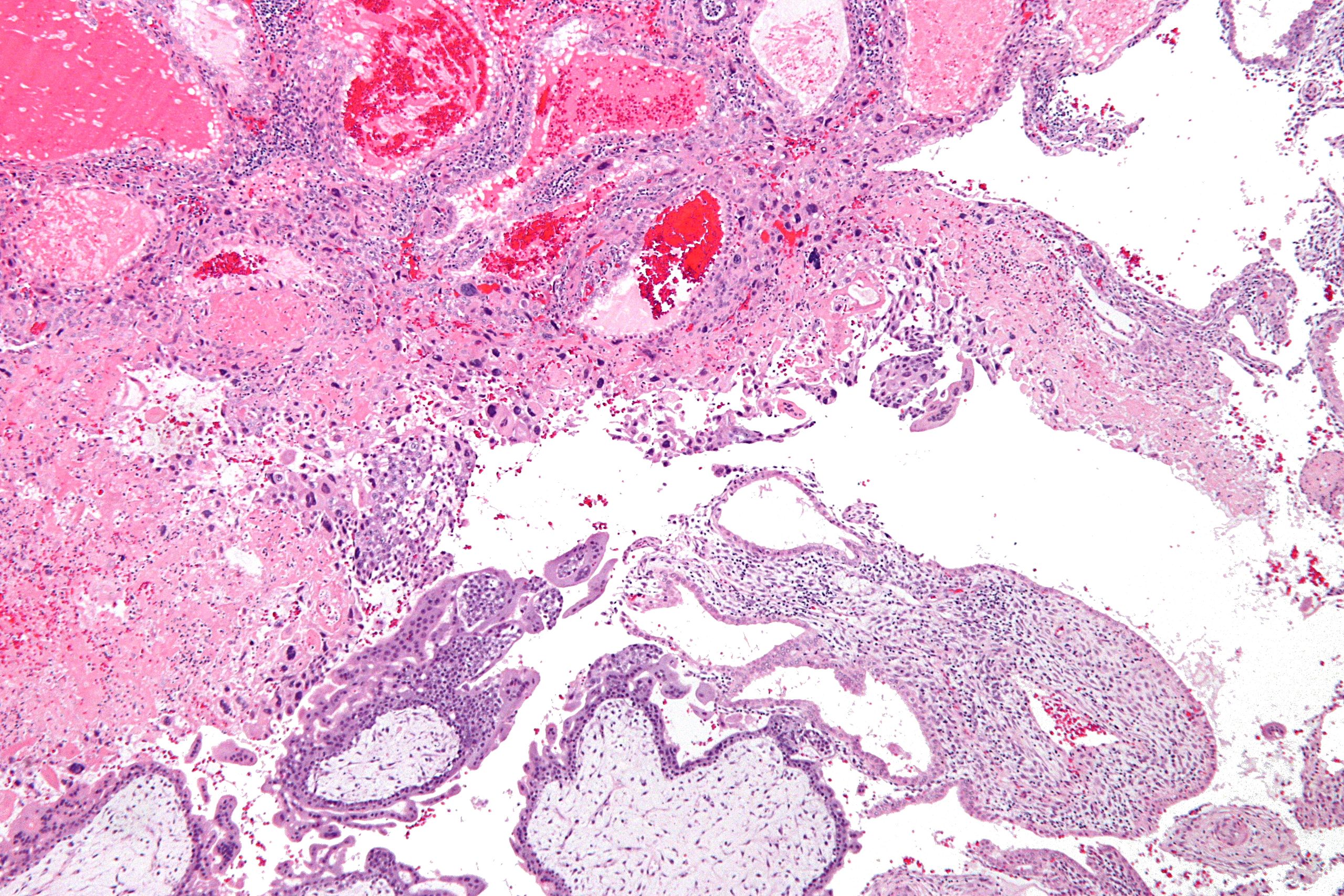
==Microscopic Pathology== | |||
On [[microscopic]] [[Histopathology|histopathological]] analysis, the characteristic features of each sub-type of gestational trophoblastic neoplasia are explained in the table below:<ref name="abc">Cellular Classification of Gestational Trophoblastic Disease. National Cancer Institute. http://www.cancer.gov/types/gestational-trophoblastic/hp/gtd-treatment-pdq/#section/_5 Accessed on October 8, 2015</ref><ref name="pmid62002622">{{cite journal |vauthors=Young RH, Scully RE |title=Placental-site trophoblastic tumor: current status |journal=Clin Obstet Gynecol |volume=27 |issue=1 |pages=248–58 |date=March 1984 |pmid=6200262 |doi= |url=}}</ref><ref name="pmid171499672">{{cite journal |vauthors=Allison KH, Love JE, Garcia RL |title=Epithelioid trophoblastic tumor: review of a rare neoplasm of the chorionic-type intermediate trophoblast |journal=Arch. Pathol. Lab. Med. |volume=130 |issue=12 |pages=1875–7 |date=December 2006 |pmid=17149967 |doi=10.1043/1543-2165(2006)130[1875:ETTROA]2.0.CO;2 |url=}}</ref> | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 600px" align="center" | |||
| valign="top" | | |||
|+ | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Types of Gestational Trophoblastic Neoplasia}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|Histopathological features}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
Invasive mole | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* [[Hyperplasia]] of [[Cytotrophoblast|cytotrophoblastic]] and [[Syncytiotrophoblast|syncytial]] elements and persistence of villous structures | |||
* [[Trophoblast|Trophoblastic]] invasion of the [[myometrium]] with identifiable villous structures | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
Choriocarcinoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Columns and sheets of [[Trophoblast|trophoblastic]] [[Tissue (biology)|tissue]] invading [[Uterus|uterine]] [[muscle]] and [[Blood vessel|blood vessels]] | |||
* [[Syncytiotrophoblast|Syncytiotrophoblasts]] (large [[eosinophilic]] smudgy [[Multinucleate|multinucleated]] [[Cell (biology)|cells]] with large [[Hyperchromicity|hyperchromatic]] [[Cell nucleus|nuclei]]) are intermixed with [[Cytotrophoblast|cytotrophoblasts]] (polygonal [[Cell (biology)|cells]] with distinct borders, and single irregular [[Cell nucleus|nuclei]]) | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
Placental-site trophoblastic tumor | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* Infiltrative growth of large, polyhedral to round, mononuclear intermediate [[Trophoblast|trophoblasts]] | |||
* [[Tumor]] [[Cell (biology)|cells]] have plentiful amphophilic, [[eosinophilic]], or clear [[cytoplasm]] | |||
* [[Cell nucleus|Nuclear]] [[pleomorphism]] | |||
* Large, convoluted [[Cell nucleus|nuclei]] with marked [[Hyperchromicity|hyperchromasia]], [[Cell nucleus|nuclear]] grooves, and [[Cell nucleus|nuclear]] pseudoinclusions | |||
* [[Mitosis|Mitotic]] count ranges from 2 - 4 per 10 high-power fields in most cases | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
Epithelioid trophoblastic tumor | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
* The [[tumor]] has a monomorphic [[Cell (biology)|cellular]] pattern of [[epithelioid]] [[Cell (biology)|cells]] and may resemble [[Squamous cell carcinoma|squamous cell cancer]] of the [[cervix]] when arising in the [[cervical]] canal | |||
* [[Nodule (medicine)|Nodular]], expansile growth of uniform, medium-sized [[Cell (biology)|cells]] arranged in cords, nests, or sheets | |||
* Characteristic well-circumscribed [[tumor]] border | |||
|} | |||
[[File:Intermediate trophoblast 3 - low mag.jpg|center|thumbnail|Courtesy Wikipedia]] | |||
==References== | ==References== | ||
| Line 79: | Line 142: | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | |||
[[Category:Medicine]] | |||
[[Category:Gynecology]] | |||
[[Category:Surgery]] | |||
Latest revision as of 00:04, 3 April 2019
|
Gestational trophoblastic neoplasia Microchapters |
|
Differentiating Gestational trophoblastic neoplasia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gestational trophoblastic neoplasia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Gestational trophoblastic neoplasia pathophysiology |
|
Gestational trophoblastic neoplasia pathophysiology in the news |
|
Blogs on Gestational trophoblastic neoplasia pathophysiology |
|
Directions to Hospitals Treating Gestational trophoblastic neoplasia |
|
Risk calculators and risk factors for Gestational trophoblastic neoplasia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Sabawoon Mirwais, M.B.B.S, M.D.[2]
Overview
Pregnancy occurs when an egg, which is released from the ovary during ovulation, is fertilized by a sperm. Human pregnancy takes approximately 40 weeks. Gestational trophoblastic neoplasia arises from the trophoblastic tissue, which provides nutrients to the embryo and develops into a large part of the placenta. Invasive mole is basically a benign tumor which arises from the invasion of the myometrium of a hydatidiform mole. Choriocarcinoma is a malignant tumor of the trophoblastic epithelium. Placental-site trophoblastic tumor (PSTT), a rare tumor, arises from the implantation site of placenta. Epithelioid trophoblastic tumor (ETT) is basically a rare variant of placental-site trophoblastic tumor (PSTT) which arises from the malignant transformation of chorionic-type intermediate trophoblastic cells. Invasive mole is usually diploid but can also be aneuploid in karyotype. Choriocarcinoma has an aneuploid karyotype and majority of the cases have a Y chromosome.
Pathophysiology
Physiology
The normal physiology of pregnancy can be understood as follows:
- Pregnancy occurs when an egg, which is released from the ovary during ovulation, is fertilized by a sperm.
- After ejaculation, the released sperm must spend some time in the female reproductive tract and undergo capacitation, which is basically the acquisition of fertilization capability.[1][2][3]
- The sperm then penetrates the egg after the acrosomal reaction and initiates the process of fertilization in the fallopian tube.[4]
- The sperm breaks through the oocyte's plasma membrane and releases its haploid nucleus into the oocyte.[5]
- Cortical reaction (changes in the oocyte membrane) prevents any further penetration by another sperm.
- Unification of the two haploid nuclei (one each from the sperm and egg) marks the completion of fertilization, resulting in the formation of a diploid zygote.
- The zygote undergoes multiple divisions called cleavage before its migration to the uterus.[6]
- Human pregnancy takes approximately 40 weeks.
Placental Trophoblast and Pregnancy
- Trophoblast (outer layer of the blastocyst) is composed of cytotrophoblast, syncytiotrophoblast, and intermediate trophoblast.[7]
- Syncytiotrophoblast invades the endometrial stroma and produces human chorionic gonadotropin (hCG).[8]
- Cytotrophoblast supplies the syncitium with cells and also forms the outpouchings that later become the chorionic villi.[9]
- Intermediate trophoblast is situated in the chroionic villi, the implantation site, and the chorionic sac.[10]
For more information on fertilization, click here.
For more information on pregnancy, click here.
Pathogenesis
Pathogenesis of each sub-type of gestational trophoblastic neoplasia is explained as follows:
Invasive Mole
- Invasive mole is basically a benign tumor which arises from the invasion of the myometrium of a hydatidiform mole.[11]
- It may be preceded by a complete or partial molar pregnancy and it rarely metastasizes.[12][13][14]
- Invasive moles are more aggressive than complete or partial hydatidiform moles.[15]
- Although rarely metastatic, it can spread through the hematogenous route to the following organs:
Choriocarcinoma
- Choriocarcinoma is a malignant tumor of the trophoblastic epithelium.[17]
- Cytotrophoblastic cells, functioning as stem cells, can undergo malignant transformation.[18]
- After the malignant transformation, the cells can differentiate into intermediate trophoblast and syncytiotrophoblast.[19]
- This mixture of cells can mimic normal development of a previllous blastocyst.[20]
- Choriocarcinoma can invade the uterine tissue and vasculature and spread to distant sites such as lungs, brain, liver, pelvis, vagina, spleen, intestines, and kidney.[21]
- Choriocarcinoma most commonly follows a molar pregnancy, spontaneous abortion, or ectopic pregnancy.
- Less commonly, choriocarcinoma can also follow a full-term pregnancy.
Placental-site Trophoblastic Tumor (PSTT)
- Placental-site trophoblastic tumor (PSTT), a rare tumor, arises from the implantation site of placenta.
- It can resemble an amplified form of syncytial endometritis.[22]
- The tumor represents malignant transformation of intermediate trophoblastic cells.[23]
- It is associated with less vascular invasion, hemorrhage, and necrosis compared to choriocarcinoma.
- Placental-site trophoblastic tumor (PSTT) has a tendency for lymphatic metastasis.[24]
- Because of the lower growth rate, the presentation of placental-site trophoblastic tumor (PSTT) can be delayed by months or even years.[25]
- Majority of the cases of placental-site trophoblastic tumor (PSTT) follow non-molar pregnancies.[26]
- 35% of placental-site trophoblastic tumors (PSTT) have distant metastases at the time of diagnosis.[23][26]
- Common sites of metastasis include the lungs, pelvis, and lymph nodes.
Epithelioid Trophoblastic Tumor (ETT)
- Epithelioid trophoblastic tumor (ETT) is basically a rare variant of placental-site trophoblastic tumor (PSTT).
- It arises from the malignant transformation of chorionic-type intermediate trophoblastic cells.[27]
- Epithelioid trophoblastic tumor (ETT) can clinically present as benign or malignant.[28]
- Majority of the cases of epithelioid trophoblastic tumors (ETT) present years after full-term gestations.[27][29]
Genetics
- Invasive mole is usually diploid but can also be aneuploid in karyotype.[30]
- Choriocarcinoma has an aneuploid karyotype and majority of the cases have a Y chromosome.[31]
- Mutation in the following genes has been associated with recurrent hydatidiform mole, a precursor of and a risk factor for gestational trophoblastic neoplasia:
- NLR family, pyrin domain-containing 7 (NLRP7)[32][33]
- KHDC3-like protein, subcortical maternal complex member (KHDC3L)[32][33]
Associated Conditions
Conditions associated with gestational trophoblastic neoplasia include:
Gross Pathology
Gross pathological findings of the sub-types of gestational trophoblastic neoplasia are as follows:
Invasive mole
- It appears as an erosive hemorrhagic lesion
- Hydropic villi sticking out from the endometrium into the myometrium can also be visible
Choriocarcinoma
- Bulky, destructive mass with hemorrhage and necrosis[37][38]
- Can be associated with deep myometrial invasion
Epithelioid Trophoblastic Tumor (ETT)
- Cystic or nodular hemorrhagic masses that can compress and infiltrate the structures around it[27][39][40]
- Size of the tumor ranges from 0.5 - 5 cm.[27][29]
- Cut surface can have a tan or white appearance with hemorrhage and necrosis
- Ulceration can be present
- Fistula formation is common
Placental-site Trophoblastic Tumor (PSTT)
- It can appear as a nodular, round, solid mass or varying size
- Necrosis and hemorrhage is commonly seen[41][42]
- Can result in perforation and extend into the broad ligament and adnexa[43]
Microscopic Pathology
On microscopic histopathological analysis, the characteristic features of each sub-type of gestational trophoblastic neoplasia are explained in the table below:[44][45][46]
| Types of Gestational Trophoblastic Neoplasia | Histopathological features |
|---|---|
|
Invasive mole |
|
|
Choriocarcinoma |
|
|
Placental-site trophoblastic tumor |
|
|
Epithelioid trophoblastic tumor |
|
References
- ↑ CHANG MC (October 1951). "Fertilizing capacity of spermatozoa deposited into the fallopian tubes". Nature. 168 (4277): 697–8. PMID 14882325.
- ↑ AUSTIN CR (November 1951). "Observations on the penetration of the sperm in the mammalian egg". Aust J Sci Res B. 4 (4): 581–96. PMID 14895481.
- ↑ AUSTIN CR (August 1952). "The capacitation of the mammalian sperm". Nature. 170 (4321): 326. PMID 12993150.
- ↑ Moore, Keith (1988). Essentials of human embryology. Toronto Philadelphia Saint Louis, Mo: B.C. Decker C.V. Mosby Co. distributor. ISBN 9780941158978.
- ↑ Moore, Keith (1988). Essentials of human embryology. Toronto Philadelphia Saint Louis, Mo: B.C. Decker C.V. Mosby Co. distributor. ISBN 9780941158978.
- ↑ Miklavcic JJ, Flaman P (May 2017). "Personhood status of the human zygote, embryo, fetus". Linacre Q. 84 (2): 130–144. doi:10.1080/00243639.2017.1299896. PMC 5499222. PMID 28698706.
- ↑ Moore, Keith (2016). The developing human : clinically oriented embryology. Philadelphia, PA: Elsevier. ISBN 9780323313384.
- ↑ Moore, Keith (2016). The developing human : clinically oriented embryology. Philadelphia, PA: Elsevier. ISBN 9780323313384.
- ↑ Moore, Keith (2016). The developing human : clinically oriented embryology. Philadelphia, PA: Elsevier. ISBN 9780323313384.
- ↑ Moore, Keith (2016). The developing human : clinically oriented embryology. Philadelphia, PA: Elsevier. ISBN 9780323313384.
- ↑ Lurain, John R. (2010). "Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole". American Journal of Obstetrics and Gynecology. 203 (6): 531–539. doi:10.1016/j.ajog.2010.06.073. ISSN 0002-9378.
- ↑ https://www.cancer.gov
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Seckl MJ, Sebire NJ, Berkowitz RS (August 2010). "Gestational trophoblastic disease". Lancet. 376 (9742): 717–29. doi:10.1016/S0140-6736(10)60280-2. PMID 20673583.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Brown J, Naumann RW, Seckl MJ, Schink J (January 2017). "15years of progress in gestational trophoblastic disease: Scoring, standardization, and salvage". Gynecol. Oncol. 144 (1): 200–207. doi:10.1016/j.ygyno.2016.08.330. PMID 27743739.
- ↑ https://www.cancer.gov
- ↑ 16.0 16.1 16.2 Seckl MJ, Sebire NJ, Fisher RA, Golfier F, Massuger L, Sessa C (October 2013). "Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up". Ann. Oncol. 24 Suppl 6: vi39–50. doi:10.1093/annonc/mdt345. PMID 23999759.
- ↑ https://www.cancer.gov
- ↑ Bishop BN, Edemekong PF. PMID 30571055. Missing or empty
|title=(help) - ↑ Mao TL, Kurman RJ, Huang CC, Lin MC, Shih I (November 2007). "Immunohistochemistry of choriocarcinoma: an aid in differential diagnosis and in elucidating pathogenesis". Am. J. Surg. Pathol. 31 (11): 1726–32. doi:10.1097/PAS.0b013e318058a529. PMID 18059230. Vancouver style error: initials (help)
- ↑ Shih I (July 2007). "Gestational trophoblastic neoplasia--pathogenesis and potential therapeutic targets". Lancet Oncol. 8 (7): 642–50. doi:10.1016/S1470-2045(07)70204-8. PMID 17613426. Vancouver style error: initials (help)
- ↑ https://www.cancer.gov
- ↑ https://www.cancer.gov
- ↑ 23.0 23.1 Feltmate CM, Genest DR, Goldstein DP, Berkowitz RS (May 2002). "Advances in the understanding of placental site trophoblastic tumor". J Reprod Med. 47 (5): 337–41. PMID 12063871.
- ↑ https://www.cancer.gov
- ↑ https://www.cancer.gov
- ↑ 26.0 26.1 Schmid P, Nagai Y, Agarwal R, Hancock B, Savage PM, Sebire NJ, Lindsay I, Wells M, Fisher RA, Short D, Newlands ES, Wischnewsky MB, Seckl MJ (July 2009). "Prognostic markers and long-term outcome of placental-site trophoblastic tumours: a retrospective observational study". Lancet. 374 (9683): 48–55. doi:10.1016/S0140-6736(09)60618-8. PMID 19552948.
- ↑ 27.0 27.1 27.2 27.3 Shih IM, Kurman RJ (November 1998). "Epithelioid trophoblastic tumor: a neoplasm distinct from choriocarcinoma and placental site trophoblastic tumor simulating carcinoma". Am. J. Surg. Pathol. 22 (11): 1393–403. PMID 9808132.
- ↑ https://www.cancer.gov
- ↑ 29.0 29.1 Allison KH, Love JE, Garcia RL (December 2006). "Epithelioid trophoblastic tumor: review of a rare neoplasm of the chorionic-type intermediate trophoblast". Arch. Pathol. Lab. Med. 130 (12): 1875–7. doi:10.1043/1543-2165(2006)130[1875:ETTROA]2.0.CO;2. PMID 17149967.
- ↑ http://www.cancer.gov
- ↑ http://www.cancer.gov
- ↑ 32.0 32.1 Murdoch S, Djuric U, Mazhar B, Seoud M, Khan R, Kuick R, Bagga R, Kircheisen R, Ao A, Ratti B, Hanash S, Rouleau GA, Slim R (March 2006). "Mutations in NALP7 cause recurrent hydatidiform moles and reproductive wastage in humans". Nat. Genet. 38 (3): 300–2. doi:10.1038/ng1740. PMID 16462743.
- ↑ 33.0 33.1 Parry DA, Logan CV, Hayward BE, Shires M, Landolsi H, Diggle C, Carr I, Rittore C, Touitou I, Philibert L, Fisher RA, Fallahian M, Huntriss JD, Picton HM, Malik S, Taylor GR, Johnson CA, Bonthron DT, Sheridan EG (September 2011). "Mutations causing familial biparental hydatidiform mole implicate c6orf221 as a possible regulator of genomic imprinting in the human oocyte". Am. J. Hum. Genet. 89 (3): 451–8. doi:10.1016/j.ajhg.2011.08.002. PMC 3169823. PMID 21885028.
- ↑ 34.0 34.1 von Welser SF, Grube M, Ortmann O (December 2015). "Invasive mole in a perimenopausal woman: a case report and systematic review". Arch. Gynecol. Obstet. 292 (6): 1193–9. doi:10.1007/s00404-015-3777-z. PMID 26050078.
- ↑ Simes BC, Mbanaso AA, Zapata CA, Okoroji CM (2018). "Hyperthyroidism in a complete molar pregnancy with a mature cystic ovarian teratoma". Thyroid Res. 11: 12. doi:10.1186/s13044-018-0056-7. PMC 6086074. PMID 30116304.
- ↑ Lu D, Tang JJ, Zakashansky K, Berkowitz RS, Kalir T, Liu Y (September 2017). "Heterotopic Pregnancy Including Intrauterine Normal Gestation and Tubal Complete Hydatidiform Mole: A Case Report and Review of the Literature". Int. J. Gynecol. Pathol. 36 (5): 428–432. doi:10.1097/PGP.0000000000000347. PMID 28800576.
- ↑ Ober, William B.; Edgcomb, John H.; Price, Edward B. (1971). "THE PATHOLOGY OF CHORIOCARCINOMA". Annals of the New York Academy of Sciences. 172 (10 Physiology a): 299–426. doi:10.1111/j.1749-6632.1971.tb34943.x. ISSN 0077-8923.
- ↑ Smith, Harriet O.; Kohorn, Ernest; Cole, Laurence A. (2005). "Choriocarcinoma and Gestational Trophoblastic Disease". Obstetrics and Gynecology Clinics of North America. 32 (4): 661–684. doi:10.1016/j.ogc.2005.08.001. ISSN 0889-8545.
- ↑ Fadare O, Parkash V, Carcangiu ML, Hui P (January 2006). "Epithelioid trophoblastic tumor: clinicopathological features with an emphasis on uterine cervical involvement". Mod. Pathol. 19 (1): 75–82. doi:10.1038/modpathol.3800485. PMID 16258513.
- ↑ Meydanli, Mutlu M.; Kucukali, Turkan; Usubutun, Alp; Ataoglu, Omur; Kafkasli, Ayse (2002). "Epithelioid Trophoblastic Tumor of the Endocervix: A Case Report". Gynecologic Oncology. 87 (2): 219–224. doi:10.1006/gyno.2002.6820. ISSN 0090-8258.
- ↑ Young RH, Scully RE (March 1984). "Placental-site trophoblastic tumor: current status". Clin Obstet Gynecol. 27 (1): 248–58. PMID 6200262.
- ↑ Baergen, Rebecca N.; Rutgers, Joanne L.; Young, Robert H.; Osann, Kathryn; Scully, Robert E. (2006). "Placental site trophoblastic tumor: A study of 55 cases and review of the literature emphasizing factors of prognostic significance". Gynecologic Oncology. 100 (3): 511–520. doi:10.1016/j.ygyno.2005.08.058. ISSN 0090-8258.
- ↑ Baergen RN, Rutgers J, Young RH (October 2003). "Extrauterine lesions of intermediate trophoblast". Int. J. Gynecol. Pathol. 22 (4): 362–7. doi:10.1097/01.pgp.0000092132.88121.d1. PMID 14501817.
- ↑ Cellular Classification of Gestational Trophoblastic Disease. National Cancer Institute. http://www.cancer.gov/types/gestational-trophoblastic/hp/gtd-treatment-pdq/#section/_5 Accessed on October 8, 2015
- ↑ Young RH, Scully RE (March 1984). "Placental-site trophoblastic tumor: current status". Clin Obstet Gynecol. 27 (1): 248–58. PMID 6200262.
- ↑ Allison KH, Love JE, Garcia RL (December 2006). "Epithelioid trophoblastic tumor: review of a rare neoplasm of the chorionic-type intermediate trophoblast". Arch. Pathol. Lab. Med. 130 (12): 1875–7. doi:10.1043/1543-2165(2006)130[1875:ETTROA]2.0.CO;2. PMID 17149967.