Flank pain
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1],Associate Editor(s)-in-Chief: Jaspinder Kaur, MBBS[2]
Overview
Flank pain is a sensation of discomfort, distress, or agony usually beginning posteriorly or in the midaxillary line in the area below the rib and above the ilium resulting from the stimulation of specialized nerve endings upon distention of the ureter or renal capsule. Flank pain originating from urinary tract pathology may be due to underlying obstruction, inflammation, or mass. Urologic etiologies such as renal calculus disease or acute pyelonephritis are considered as the most common causes; however, cardiac, intraabdominal, musculoskeletal, and psychological causes should be considered on a probable list. The kidney and its capsule are innervated by sensory fibers traveling to the T10-L1 spinal cord; hence, pain originating from it is often felt just lateral to the sacrospinalis muscle beneath the 12th rib posteriorly. The pain often radiates anteriorly and referred to the inguinal, labial, penile, or testicular areas. The quality and severity of the pain may aid in making the probable diagnosis as the severity of the pain generally correlates inversely with the duration of the problem. A dull and steady pain indicates the infectious etiology such as acute pyelonephritis; whereas pain that is due to an acutely obstructing calculus can be intense and sharp. Mild to moderate flank pain is usually reported in the cases such as slowly enlarging ureteral tumor because it results in chronic gradual but possibly severe distention of the renal collecting system and capsule over a long period of time. Conversely, the acute flank pain due to an obstructing renal calculus termed as renal colic is often severe and sharp as it results in sudden distention of the renal collecting system and capsule. It is important to determine if the pain represents an emergency condition or can be managed in the outpatient setting. When flank pain is associated with fever, dehydration, nausea, vomiting or other comorbid medical conditions, such as diabetes, immunocompromised state, or pregnancy; hospital admission may be necessary to prevent possible complications such as pyelonephritis, urosepsis or even renal failure.
Pathophysiology
- Characteristics of pain: Flank pain originating in the urinary system is caused by distention of the ureter, renal pelvis or renal capsule. The severity of the pain is directly related to the rapidity or acuteness of the obstruction irrespective of the degree of distention.
- Acute onset: These patient will have extremely severe pain with mild dilation of the ureter and no irreversible renal damage. Hence, as stone passes through the ureter and suddenly becomes lodged in one position causes extremely severe pain and subsequently, causing multiple episodes of pain with a stone becoming lodged in a new and more distal position in the ureter.
- Chronic onset: They might have no pain or mild pain because the ureteral dilation has developed over a long period of time resulting in a severe ureteral obstruction and irreversible renal damage.
- Course of pain in ureteral obstruction: The location of pain can help to predict the level of obstruction in the urinary tract.
- Proximal ureteral or renal pelvic obstruction: Flank pain originating in the posterior part of the flank and radiating to the ipsilateral testicle of the male or the labia of the female is usually due to the common innervation of the testicle and the renal pelvis (T11–12).
- Middle third of the ureter: Gradually, the pain becomes lower and more anterior in the flank.
- Ureterovesical junction obstruction: The pain is lower and radiates to the scrotal skin rather than the testicle, and is associated with voiding symptoms such as urinary frequency and urgency.
- Renal stone formation: It involves two processes namely urine supersaturation and physicochemical changes.
- Urine supersaturation: Patients with low urine volumes (usually less than 1 liter per day) increase the concentration of solutes (indicated by urine with an osmolarity greater than 600 mOsm/kg) and promote urinary stasis, which can cause supersaturation of solutes and lead to stone formation. In the setting of supersaturation, solutes precipitate in the urine leading to nucleation and crystal concretions. In respect to nephrolithiasis, supersaturation of stone-forming constituents like calcium, phosphorus, uric acid, oxalate, cystine, and low urine volume are risk factors for crystallization.
- Physicochemical changes: PH and specific concentrations of excess substances influence the transformation of a liquid to a solid. Most urinary stones start as Randall's plaque at the junction of the nephron's collecting tubule and the renal pelvis in the papilla. These plaques start suburothelial and then gradually grow until they break through into the renal pelvis. Once in continuous contact with urine, layers of calcium oxalate typically start to form on the calcium phosphate nidus (all Randall's plaques are composed of calcium phosphate). Calcium oxalate stones tend to form when the urinary pH is under 7.2, while calcium phosphate will form in the more alkaline urine. Hyperparathyroidism and similar metabolic disturbances like renal tubular acidosis typically form stones that are primarily or significantly composed of calcium phosphate. Overly acidic urine is the primary cause of uric acid stones (not hyperuricosuria).
- Acute pyelonephritis: E. coli is the most common bacteria due to its unique ability to adhere to and colonize the urinary tract and kidneys. E.coli has adhesive molecules called P-fimbriae which interact with receptors on the surface of uroepithelial cells. Kidneys infected with E. coli can lead to an acute inflammatory response which can cause scarring of the renal parenchyma. Though the mechanism in which renal scarring occurs is still poorly understood, it has been hypothesized that the adhesion of bacteria to the renal cells disrupts the protective barriers resulting in the localized infection, hypoxia, ischemia, and clotting in an attempt to contain the infection. Inflammatory cytokines, bacterial toxins, and other reactive processes further lead to complete pyelonephritis and in many cases systemic symptoms of sepsis and shock.
Causes
- The etiology of flank pain is multifactorial which ranges from local, systemic, metabolic to underlying genetic factors. Depending upon the etiology in association with other comorbidities, it is determined to treat the patients in an outpatient or hospital setting; as life-threatening causes may result in death or permanent renal disability within 24 hours if left untreated.
Table 1: List the most common and life threatening causes of flank pain
| Common Causes | Life Threatening Causes |
|---|---|
Flank pain developed by WikiDoc.org |
Flank pain developed by WikiDoc.org |
Table 2: System wise causative factors of flank pain
Table 3: Alphabetical presentation of the causative factors of flank pain
Epidemiology and Demographics
- Renal colic: Nephrolithiasis affects approximately 5% to 15% of the population, and out of those, 50% will have a recurrent stone within 5-7 years of the initial presentation if preventive measures are not practiced. Over 70% of stones occur in people 20 to 50 years old, and they are more common in men than women by a factor of about 2:1.
- Acute pyelonephritis: It is reported at a rate of 15 to 17 cases per 10,000 females and 3 to 4 cases per 10,000 males annually in the United States. Extreme age groups such as the elderly and infants are at increased risk due to abnormalities in anatomy and changes in hormones. Sexually active young women and pregnant females can also be at higher risk, and usually 20% to 30% will develop acute pyelonephritis during the second and early third trimester. Acute pyelonephritis has no racial predisposition.
- Renal infarction: Renal artery thrombosis is usually seen at the age of 30-50’s. Renal infarctions are rare, numbers vary according to different studies (0.007%), and reported incidence is 0.01% in Europe and Asia. It can be missed on patient work-up, and hence, makes its documented incidence falsely lower than the true incidence.
- Urinary tract infection: They are very frequent bacterial infection in women and usually occur between the ages of 16-35 years, with 10% of women getting an infection yearly and more than 40% to 60% having an infection at least once in their lives. Recurrences are common, with nearly half getting a second infection within a year. They occur four times more frequently in females than males.
Risk Factors
- Risk factor consists of primary factors which are mainly related to urinary system, and secondary conditions arising from extra-urinary pathologies which predisposes the patients to the flank pain.
Table: List the risk factors for flank pain
| Urinary conditions | Extra-urinary conditions |
|---|---|
|
|
Screening
- Prenatal renal ultrasound: Its objective is to describe the type of renal anomaly, to exclude associated malformations, and to screen for parameters predictive of deranged renal function postnatally; hence, allowing for a needful multidisciplinary perinatal approach.
- It can detect several conditions such as unilateral renal agenesis or aplasia, ectopic kidneys, fetal hyperechoic kidneys resulting from obstructive dysplasia, bilateral multicystic kidney disease (both autosomal recessive and dominant), nephroblastomatosis, renal vein thrombosis, ischemia, infectious and metabolic diseases, nephrotic syndrome and aneuploidy; obstructive cystic dysplasia and antenatal hydronephrosis.
- These conditions can present with flank pain at any age depending upon the severity of the underlying disorder. Therefore, knowledge about the specific conditions will help with prenatal counseling, determination of the need for therapeutic intervention in utero versus early delivery, and the postnatal evaluation and management of these condition.
Prognosis
- Nephrolithiasis: The prognosis for most patients with kidney stones is good as most of them passes within four weeks, but stones larger than 8 mm may require some intervention before they can get excreted. The recurrence of kidney stones is common as 30-50% of individuals have a recurrent stone within 10 years after a first stone episode; therefore, the patient should be educated on adequate fluid intake and avoidance of certain foods.
- Acute pyelonephritis: Overall mortality has been reported around 10% to 20% in some studies with a recent study from Hong Kong stating a mortality rate closer to 7.4%. It further reported that the old age (older than 65 years), male gender, impaired renal function, or presence of disseminated intravascular coagulation were associated with increased mortality. However, with the timely detection of the underlying etiology and prompt intervention with adequate treatment, even patients with severe pyelonephritis generally have a good outcome.
- Urinary tract infection: The majority of women have an excellent outcome as the mortality after a UTI is close to zero. The duration of symptoms is usually 2 to 4 days following treatment with an antibiotic; however, nearly 30% of women will have a recurrent episode. Morbidity is usually seen in older debilitated patients, and those with renal calculi, diabetes, underlying malignancy, chemotherapy and chronic catheterization of the bladder.
Complications
- Acute pyelonephritis: Renal or perinephric abscess formation, sepsis, renal vein thrombosis, papillary necrosis, acute renal failure, emphysematous pyelonephritis.
- Urinary tract infection: pyelonephritis and/or pyonephrosis.
- Renal infarction: Declining renal function and/or renal failure.
Flank pain in reproductive aged and pregnant females
- In females of reproductive age, the gynecologic and obstetric causes of flank pain such as ectopic pregnancy, ovarian cyst, ovarian torsion, and pelvic inflammatory disease are important considerations in addition to the diagnoses commonly found in the general population.
- Before ordering diagnostic work-up in premenopausal women, it is mandatory to obtain a beta human chorionic gonadotropin (β-hCG) measurement to narrow the differential diagnosis and to limit the possibility of exposing an embryo or fetus to ionizing radiation.
- Transvaginal or transabdominal ultrasonography (USG) of the pelvis is the recommended imaging study for reproductive-aged females in whom a gynecologic etiology is suspected or a β-hCG test result is positive.
- In pregnant patients with acute flank pain, USG and MRI are typically the imaging studies of choice because they lack ionizing radiation.
- MRI has been shown to have excellent sensitivity and specificity for the evaluation of the etiologies of the flank pain in females.
- If USG and MRI are unavailable or inconclusive and if serious pathology remains a concern, CT can be used. The risk of a negative outcome for a developing embryo or fetus exposed to a single CT of the abdomen and pelvis is very low.
- The American College of Radiology (ACR) practice parameter regarding the use of imaging with ionizing radiation in pregnant patients outlines the specific risks based on gestational age and emphasizes the importance of obtaining informed consent from the patient before imaging is performed.
- Physiologic hydronephrosis of pregnancy occurs in >80% of pregnant women, more commonly occurs on the right than the left, and is generally seen beginning in the second trimester. *However, the differential diagnosis of hydronephrosis in the pregnant patient is confounded by physiologic hydronephrosis of pregnancy which is thought to be caused by compression of the ureters between the gravid uterus and the linea terminalis.
Diagnosis
History and Symptoms
- The history is the most important and initial source of the evaluation of the patient presenting with flank pain.
- Onset and severity:
- Acute and severe pain most commonly results from an acute obstruction of the urinary tract due to a calculus and often termed as a renal colic.
- Chronic and dull pain is more typical of an underlying infectious, malignant, or congenital anomalies.
- Nausea and Vomiting: These symptoms are due to irritation of the peritoneum and distention of the renal capsule; and are most severe when the flank pain is acute and severe originating from a renal calculi.
- Urinary frequency and urgency: It is due to the referred pain to the bladder area.
- Gross hematuria: It mandates a complete urological evaluation to rule out a malignancy of the urinary tract such as a renal carcinoma, bladder carcinoma, or ureteral tumor. The diagnostic work-up should include imaging of the upper urinary tract with ultrasound or CT scan and evaluation of the bladder with cystoscopy.
- Fever: It is an ominous sign indicating an infectious etiology. The source of the fever typically is infected urine that remains undrained behind the source of obstruction such as a calculi, stricture, or tumor. However, in the cases where the patient complains of flank pain and fever with no underlying obstruction of the urinary tract collecting system; acute pyelonephritis should be most likely suspected as the renal tissue itself is infected.
- Comorbid conditions: They might predispose an individual to urosepsis.
- Tobacco use: Its use should be ruled out as it increases the risk for developing a transitional cell carcinoma. The tumor or a blood clot formation from gross hematuria can cause obstruction resulting in the flank pain similar to produced by a renal calculi.
- Cardiac arrhythmias: It can presents with acutely severe flank pain due to underlying possible thromboembolic event. In such scenarios, a cardiac thrombus suddenly is dislodged and obstructs the main renal artery or one of its branches. The resulting pain is identical to that produced by a renal calculi; hence, a history of cardiac arrhythmia is essential for establishing the diagnosis. A functional imaging study such as an IVP, contrast-enhanced CT, or renal angiogram demonstrates absence of renal blood flow and confirms the obstruction of the renal artery.
Physical Examination
- A complete physical examination helps to determine the etiology and the severity of the problem in order to avoid the focus on the urinary tract or flank area exclusively.
- Vital signs: They are taken to determine the association with dehydration, infection, or urosepsis.
- Urosepsis: It is suggested in patients with fever, rapid pulse rate, respiratory rate and labile blood pressure. The patients should be hospitalized in all suspected cases of urosepsis to prevent septic shock by providing intravenous antibiotics, aggressive fluid replacement and urologic relief of any hydronephrosis situation.
- Urinary tract infection: A low grade fever may indicate a lower urinary tract infection (bladder) and high spiking temperatures suggest upper tract infection (kidney). However, it is not always correct to localize the site of the infection by the severity of the temperature. In other words, a high temperature necessarily does not indicate upper urinary tract infection and vice versa especially in children.
- Carotid arteries: They should be auscultated for bruits to evaluate for a possible cardiac etiology of the flank pain such as a renal artery disease or embolus.
- Heart auscultation: Heart rate, rhythm, and murmurs should be listened for underlying renal artery embolism which usually occurs in patients with atrial fibrillation.
- Abdomen: It should be examined for bruits, tenderness, and masses. If the pain is more severe during the abdominal examination, consider intraabdominal etiologies for the flank pain.
- Rectal examination: It should be done with stool for guaiac test to exclude a possible intraabdominal cause for the flank pain.
- Genital examination: It should be done in both males and females since referred pain is common. The bladder sometimes is able to be palpated just above the pubic symphysis. A distended bladder suggests a possible urological etiology for the pain. In females, it is essential to determine if the patient is pregnant with a urine or serum b-human chorionic gonadotropin (b-HCG) test. If the patient is pregnant, x-rays should be avoided, and ultrasound should be used for the evaluation.
- Flank area: It should be examined for asymmetry, mass, and percussion tenderness. It is uncommon to discover a palpable flank mass unless a large underlying renal tumor is present. Patients with acute pyelonephritis or obstructing renal calculi complain of severe pain when the flank is percussed, so it is important to tap lightly in order to maintain patient confidence.
- Lower extremities: The lower extremities should be examined for motor and sensory function to rule out a musculoskeletal etiology for the flank pain.
Laboratory Findings
- Urinalysis:
- Initial diagnostic test.
- Parameters to be considered: pH, WBCs, RBCs, bacteria, casts, and crystals
- High (alkaline) pH: Infected urine secondary to urea splitting bacteria
- Acidic pH: Patients with uric acid stones tend to have an acidic urine, since these stones do not form when the urine is alkaline.
- WBC: The presence of WBCs in the urine may signify infection, but it also may be due to inflammation caused by a stone. The presence of WBC casts strongly suggests urinary tract infection or acute pyelonephritis.
- RBC: Tumors of the urinary tract usually result in urinary RBCs, and the urine may appear grossly bloody. A stone similarly can result in RBCs in the urine, so it is important to repeat a urinalysis in patients after they have passed the stone to exclude an underlying urologic cancer. If the patient has RBCs in the urine after the stone has passed, urologic evaluation is necessary.
- Gram stain: It should be done in the emergency room or clinic and can help determine if infection is present. In the case presented, a negative Gram stain suggests sterile urine. Finding bacteria on an unspun specimen suggests infection. Most urinary tract infections are caused by gram-negative bacteria such as E. coli; however, gram-positive organisms can cause urinary tract infections as well. If urinary calculi are present within the urinary tract, it is not uncommon to find crystals in the urine analysis, along with RBCs and WBCs.
- Crystals: The shape of the crystal can be used by the laboratory technician to help identify its composition.
- The urinalysis may be normal if the etiology of the flank pain is due to cardiac, intraabdominal, musculoskeletal, or psychological problems.
- Complete Blood Count:
- If the serum WBC count is elevated, infection is suspected.
- Anemia and a low or high platelet count might be seen in the presence of bleeding urologic tumors.
- An abnormally high hematocrit can be seen if the patient is dehydrated.
- Serum blood urea nitrogen (BUN):
- An elevated BUN can be due to renal disease or dehydration.
- In general, if the BUN is greater than 10 times the serum creatinine level, then the elevation most likely is due to dehydration.
- If the BUN to serum creatinine ratio is 10 or less, then renal disease is likely.
- Serum creatinine:
- It level directly reflects renal function.
- An elevated creatinine indicates impaired renal function, regardless of the BUN value. The impaired function could be due to dehydration, obstruction, tumor, infarct, or medical renal disease. Moreover, an elevated serum creatinine indicates bilateral renal disease or disease involving a solitary kidney, since only one healthy kidney is required to maintain a normal serum creatinine.
- Serum sodium: Hyponatremia results from volume overload and can cause nausea, vomiting, and seizures.
- Serum potassium: Hyperkalemia is dangerous, since it could result in cardiac arrhythmias.
- Serum bicarbonate: Its level falls in long-standing renal compromise along with hyperkalemia.
- Serum uric acid level and Serum calcium level: The levels are measured if a urinary calculus is suspected.
- Beta hCG test: It is done to confirm or rule out a pregnancy in reproductive age group females.
- Miscellaneous: Anti nuclear antibody, perinuclear anti neutrophil and cythoplasmic anti neutrophilic antibody, protein C and protein S levels, Factor V Leiden mutation, anticardiolipine antibody IgM and IgG, antithrombine 3 activity, B12 vitamine, folic acid, homocysteine levels are done to rule out other differential conditions, hypercoaguable states and thromboembolic events.
- Blood and Urine culture: Positive urine culture shows growth of ≥ 105 colony-forming units per mL of urine. Positive blood culture is found in 15 to 30 percent of cases.
- Peripheral blood film: It show leukocytosis with or without left shift.
X-ray
- A plain film of the abdomen can help identify urinary calculi. This film is called a KUB, since it visualizes the kidney, ureter, and bladder.
- The entire film should be viewed for intestinal gas pattern, gallstones, bony structure, and free air, which may provide insight into the etiology of the pain.
- Renal cell carcinomas are osteolytic tumors, and this can be seen radiographically in metastatic disease.
- An abnormal intestinal gas pattern, gallstones, or free air suggest intraabdominal pathology.
- Aortic calcifications and aneurysms should be determined, since they might suggest renal artery disease as the etiology of the flank pain.
- Urinary calculi typically are seen as calcifications overlying the kidney shadow or along the course of the ureter. Small stones, 1 to 2mm in size, can cause severe flank pain if they obstruct the flow of urine into the bladder. Stones typically become obstructive where the ureter meets the renal pelvis [ureteropelvic junction (UPJ)], where the ureter crosses over the pelvic brim, and where the ureter enters the bladder [ureterovesical junction (UVJ)]. Small stones tend to lodge at the UVJ, whereas bigger stones lodge higher in the urinary tract. It should be noted that uric acid calculi are radiolucent and are not seen on a plain film of the abdomen, but they can be seen on ultrasound or CT scan.
Intravenous pyelogram (IVP)
- The IVP is a relatively inexpensive functional study that diagnoses most urologic, infectious, and cardiac causes of flank pain.
- It requires the administration of iodine-based intravenous contrast medium; therefore, an allergic reaction to the contrast is possible. These reactions can be severe and have resulted in hemodynamic and respiratory collapse. To avoid contrast reactions, an ultrasound or noncontrast CT can be used instead of an IVP.

Source: Case courtesy of Dr Aditya Shetty, Radiopaedia.org, rID: 27633 - However, if the clinician is concerned about a possible renal infarct secondary to an arterial embolus, a renal ultrasound and noncontrast CT scan might be normal, since they do not assess renal function. In this instance, the kidney looks normal; however, it is no longer functioning due to the recent infarct. To assess function, either an IVP or intravenous contrast enhanced CT scan could be done.
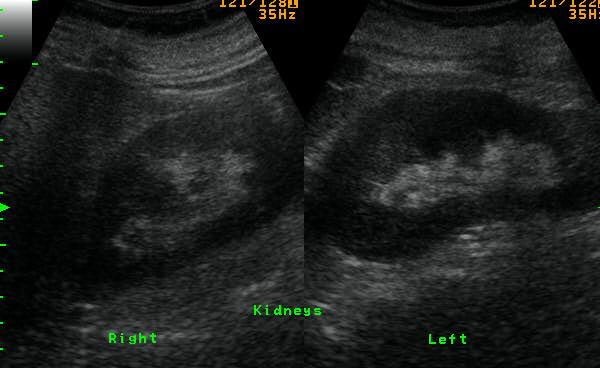
Ultrasonography (USG)
- U/S is commonly performed as primary imaging modality in patient with acute flank pain since it is a safe, rapid, inexpensive and repeatable technique allowing the identification of stones located in the renal pelvis and calyces, detect renal pelvic dilation and other renal pathologies.
- Advantages of US are its lack of ionizing radiation and its ability to demonstrate some stones. Its disadvantages include the need for skilled personnel, its inability to accurately measure the size of the stone, the need to observe the ureteral jet phenomenon at the ureterovesical junction, and its inability to differentiate dilatation without obstruction from true obstruction.
- Ultrasonographic findings in Renal stones:
- Renal stones on US are hyperechoic and show posterior acoustic shadowing depending on their size and the transducer frequency.
- US is highly effective at showing large stones (>5 mm), with nearly 100% sensitivity, but poor at visualizing stones smaller than 3 mm. It may be hard to distinguish small stones from vascular calcifications.
- When renal stones obstruct the ureter, US is very effective in demonstrating the secondary sign of hydronephrosis. Although US can detect renal stones located at the upper ureter or distally at the ureterovesical junction that cause hydronephrosis, most ureteral stones are typically obscured by overlying bowel gas. US had a sensitivity of only 37% for direct ureteral stone detection, but when hydronephrosis was included as a positive sign for a ureteral stone the sensitivity increased to 74%. Additional kidneyureter bladder plain abdomen radiography or CT increased the sensitivity for ureteric stones to 100%.
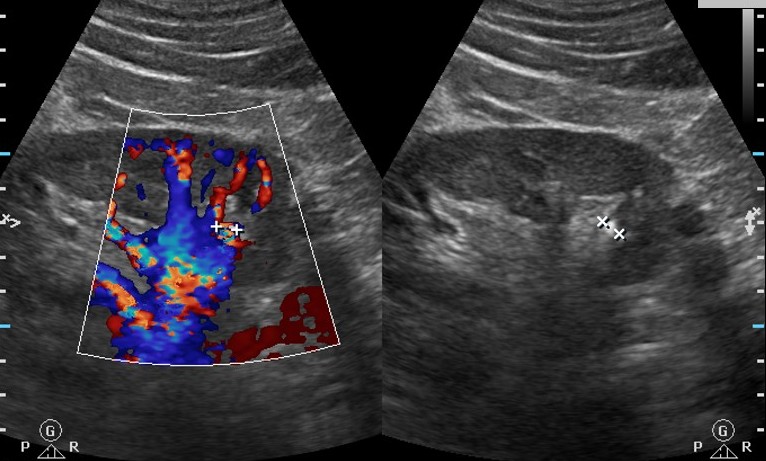
Source: Case courtesy of Brendan Cullinane, Radiopaedia.org, rID: 12932 - In addition, secondary findings of renal stones or hydronephrosis include the twinkling artifact and the absence of a urine jet on the affected side. The twinkling artifact is a rapid alternation of color immediately behind a stone that may be observed on color Doppler imaging, just like gallbladder stones. The twinkling artifact is mainly observed on rough, hyperechoic, irregular surfaces with multiple cracks, which cause a strong reflection of incident ultrasound waves. It appears as a discrete focus of alternatingcolors with or without an associated color comet-tail artifact. The appearance of the twinkling artifact is highly dependent on the machine settings, and in order to observe it clearly, it is recommended to use a low pulse repetition frequency and high color priority. Urine jets occur from the periodic contraction of the ureters and are easily visible on color Doppler imaging. Obstruction manifests as either the complete absence of the urine jet on the affected side or continuous low-level flow on the affected side, depending on the severity of the obstruction.
- Ultrasonographic findings in Acute Pyelonephritis:
Source: Case courtesy of Dr Ayush Goel, Radiopaedia.org, rID: 26161 - The most common sonographic finding of APN is normal echogenicity. In other words, most patients with clinically suspected APN (up to 80%) have negative US results.
- When positive findings of APN are suspected on US, they can include hypoechogenicity due to parenchymal edema and hyperechogenicity in cases of hemorrhage, swelling, a perfusion defect on power Doppler images, loss of corticomedullary differentiation,wall thickening of the renal pelvis, or abscess formation.
- Despite the presence of several ancillary findings for the diagnosis of APN, it can be very difficult to differentiate between artifacts and true positive findings if the sonic window is poor (due to bowel gas, bony thorax, or thick subcutaneous fat tissue) or if the patient’s respiration is irregular (due to conditions such as tachypnea). Thus, CT is considered to be the modality of choice for evaluating acute bacterial pyelonephritis.
CT scan
- UNENHANCED HELICAL COMPUTED TOMOGRAPHY:
- Since its introduction by Smith et al in 1995, unenhanced helical computed tomography (CT) has revolutionized the imaging evaluation of acute flank pain. Unlike excretory urography, unenhanced helical CT is fast (less than 5 minutes), usually does not require the intravenous administration of contrast material, and has very low interobserver variability. It also requires no patient bowel preparation, making it particularly effective in the emergent setting.
- The sensitivity and specificity of CT for diagnosing kidney stones have been reported as 95% to 96% and 98% to 100%, respectively, with overall accuracy of 98%.
- Unenhanced helical CT scan is now thought to be the investigation of choice for the diagnosis of renal colic, since it can be rapidly performed and can detect nearly all types of renal calculi. In addition it may detect extrarenal causes of abdominal pain including appendicitis, diverticulitis, biliary tract disease, leaking aortic aneurysm, and gynecologic disease. However, it cannot easily detect renal artery thromboembolism.
- The only stones that CT typically does not detect are completely radiolucent stones, such as stones secondary to indinavir therapy, an antiretroviral agent. Computed tomography can determine both the size and location of stones, the primary predictors of whether a ureteral stone will pass primarily without intervention. Ureteral stones that are 5 mm or smaller in maximum diameter and/or distally located are much more likely to pass. However, CT measurement of the maximum stone diameter does not always correlate well with the actual stone size, often overestimating the maximum diameter by 1 mm or more.

Source: Case courtesy of Assoc Prof Frank Gaillard, Radiopaedia.org, rID: 9233 - CT scan of the kidney with intravenous contrast media is fast becoming the diagnostic technique of choice for renal embolism. Renal infarcts are most easily identified on post contrast images, preferably in the cortical/arterial phase. One or more focal, wedge-shaped parenchymal defects that involve both the cortex and medulla and extend to the capsular surface are demonstrated. In cases where the main renal artery is occluded, then the entire kidney fails to enhance. In ~50% of cases, a thin rim of cortex continues to enhance, due to collateral capsular perfusion. This is known as the cortical rim sign, and is not usually present immediately after infarction, but can be seen as early as 8 hours after occlusion (typically best seen several days later). Occasionally flip-flop enhancement can be seen, where a region of hypoenhancement on early phases becomes hyperattenuating on delayed imaging.
- Although CT scanning has become the diagnostic test of choice for kidney stones, it is not without drawbacks, primarily exposure to ionizing radiation and cost. Another important consideration is the discovery of incidental findings on CT that, although at times may be helpful, may frequently lead to further testing and intervention that may be unnecessary and result in increased risk and cost.
MRI
- MRI can be considered as an alternative to low-dose NCCT in certain patient populations, such as pregnant women (noncontrast MRI), young individuals, and individuals who have undergone multiple prior CT examinations.
- In general, MRI is highly accurate for the diagnosis of hydronephrosis and perinephric edema but is less accurate in directly visualizing stones as compared to NCCT.
- The sensitivity of MRI, at 82%, is higher than that of ultrasonography and KUB radiography but less than that of CT, as stones are less easily visible when using MRI than they are when using CT.
- Diffusion-weighted imaging has also been shown to detect changes in renal perfusion and diffusion in the setting of acute ureteral obstruction.
- A major advantage of MRI is the ability to provide 3D imaging without radiation. Unfortunately, the drawbacks of MRI prevent it from widespread use in stone imaging. In general, MRI costs about three times more than a CT scan and has lower accuracy and much longer image acquisition times.
Other Diagnostic Studies
- CT renal angiography, CT angiography, and DMSA radioisotope scan can be used to diagnose renal infarction.
- In renal infarction patients, the CT angiography is the initial tool of choice, but definite diagnosis is made by renal angiography. The classic finding is of a wedge-shaped zone of peripheral diminished density without enhancement.
- Renal doppler: Doppler evaluation of renal arterial and venous blood flow should be able to detect global or major segmental renal infarction by demonstrating the absence of blood flow. Yet, segmental renal infarction has more risk to be missed by Doppler than global renal infarction.
- ECG, Echocardiography and Holter monitoring: They are done to rule out other underlying systemic conditions such as atrial fibrillation, infective endocarditis, previous infarction, and valvular or ischemic heart disease resulting in renal infarction.
Tips to remember
- NCCT is the most accurate technique for evaluating flank pain.
- Low-dose NCCT should be performed when evaluating for renal or ureteral stones.
- If there is uncertainty about whether a calcific density represents a ureteral stone or a phlebolith, intravenous contrast material can be administered and excretory-phase images obtained for definitive diagnosis.
- In pregnant patients with flank pain, US is the best initial study.
- Abdominal radiography combined with US may be able to diagnose most clinically significant stones and should be considered, especially in young patients and those with known stone disease.
- MR could be considered to evaluate for hydronephrosis though is less accurate for the direct visualization of renal and ureteral stones.
Treatment
- Treatment can be provided as as either outpatient or inpatient. Inpatient treatment is usually required for those who are very young, elderly, immunocompromised, those with poorly controlled diabetes, renal transplant, patients, patients with structural abnormalities of the urinary tract, pregnant patients, or those who cannot tolerate oral intake.
- The mainstay of treatment is analgesics, antipyretics, and antibiotics. Optimal timing of intervention for renal colic depends on the underlying etiology. For an obstructing stone, intervention is suggested even in asymptomatic patients after 30 days due to the increased risk of scarring and other complications.
- NSIADS: Immediate intervention with analgesia and antiemetics. NSAIDs and opiates are first-line therapies for analgesia. NSAIDs work in two ways in renal colic. First, NSAIDs decrease the production of arachidonic acid metabolites, which mediate pain receptors, alleviating pain caused by distension of the renal capsule. Additionally, they cause contraction of the efferent arterioles to the glomerulus, causing a reduction in glomerular filtration, and reducing hydrostatic pressure across the glomerulus. Because patients are frequently unable to tolerate oral medications, parenteral NSAIDs such as ketorolac (15 mg to 30 mg intravenously (IV) or intramuscularly (IM)) or diclofenac (37.5 mg IV) are most commonly used.
- LIDOCAINE: Successful use of intravenous lidocaine for renal colic has been reported. The protocol is to inject lidocaine 120 mg in 100 mL normal saline intravenously over 10 minutes for pain management. It has been quite effective for intractable renal colic unresponsive to standard therapy and typically starts to work in 3-5 minutes. No adverse events have been reported.
- OPIATES: Opiate pain medication, such as morphine sulfate (0.1 mg/kg IV or IM) or hydromorphone (0.02 mg/kg IV or IM), can also be used effectively for analgesia, especially when other measures have failed. However, opiates are associated with respiratory depression and sedation, and there is a risk of dependence associated with prolonged opiate use. Anti-emetic agents may be given along with the narcotics as nausea and emesis may occur with stone passage and commonly complicate narcotic use.
- FLUIDS: Fluid hydration. Although there is no evidence to support that empiric fluid will help “flush out” a stone, many patients are dehydrated secondary to decreased oral intake or vomiting and can benefit from hydration.
- MEDICAL THERAPY: Medical expulsive therapy. Alpha 1 adrenergic receptors exist in increasing concentration in the distal ureter. The use of alpha blockade medications (for example, tamsulosin or nifedipine) is theorized to facilitate stone passage by decreasing intra-ureteral pressure and dilating the distal ureter. However, data from randomized control trials are somewhat mixed as to whether these medications improved stone passage. The consensus opinion is they may be helpful in smaller stones in the lower or distal ureter. They are probably of little use in larger stones in the proximal ureter.
- CONSERVATIVE VS SURGICAL MANAGEMENT: The size of the stone is a major determinant of the need for surgical management vs. conservative management. Stones vary from less than 2 mm to greater than 2 cm in diameter. The majority of stones are less than 4 mm in width, small enough to pass spontaneously in most patients. A stone’s size is an important factor together with symptom severity, degree of obstruction, presence or absence of infection, and level of renal function in deciding whether to manage the stone initially by observation, awaiting spontaneous passage, or to intervene with a surgical procedure. Stones with a width of 5 mm or less have a 50% chance of spontaneous passage if in the proximal ureter and a better chance if in the distal ureter. Overall, for stones ≤5 mm, approximately 68% will pass spontaneously. For stones >5 mm and ≤10 mm, an estimated 47% will pass spontaneously. One study found that stones > 9mm had only a 25% chance of spontaneous passage. Distal stones are more likely to clear than proximal stones (proximal ureter 48%, mid-ureter 60%, distal ureter 75% passage rate). Thus, in many patients with renal colic symptomatic treatment and close follow-up with the anticipation of stone passage is reasonable. The presence of infection, obstruction, refractory or difficult to treat pain, or deterioration of renal function indicates the need to urological consultation and the consideration of surgical intervention.
- SURGICAL OPTIONS: Definitive management of impacted stones. There are several invasive methods to improve stone passage. These include shock wave lithotripsy, in which high energy shock waves are used to fragment stones, ureteroscopy with either laser or electrohydraulic stone fragmentation, or in rare cases, open surgery. In the presence of infection, a double J stent or percutaneous nephrostomy may be used to help with urinary drainage of the affected renal unit with definitive stone therapy postponed until the patient is stable.
- NERVE BLOCK: Nerve blocks can often be helpful, especially in chronic cases of flank pain. An anesthetic injection is typically injection proximal to the area of the 11th or 12th intercostal nerve. Good efficacy of a nerve block suggests a musculoskeletal or neuropathic etiology. Paraveterbral, splanchnic and intercostal nerve blocks have all shown varying degrees of efficacy in relief from flank pain.
- ANTIBIOTICS in UTI: Trimethoprim/Sulfamethoxazole for 3 days is good mini-dose therapy, but resistance rates are high in many areas. First-generation cephalosporins are good choices for mini-dose therapy. Nitrofurantoin is a good choice for uncomplicated UTI, but it is bacteriostatic, not bacteriocidal, and must be used for 5 to 7 days. Fluoroquinolones have high resistance but are a favorite of urologists for some reason. Recent precautions from the FDA about fluoroquinolone side effects should be heeded. Recently the FDA approved fosfomycin as a single-dose therapy for uncomplicated UTI caused by E coli. Adjunctive therapy with phenazopyridine for several days may help provide symptom relief. Even without treatment, the UTI will spontaneously resolve in about 20% of women. The likelihood that a female will develop acute pyelonephritis is very small. Asymptomatic bacteriuria is quite common and requires no treatment, except in pregnant women, those who are immunosuppressed, have undergone a transplant or have undergone a urological procedure.
- ANTIBIOTICS in Pyelonephritis: The initial selection of antibiotics will be empiric and should be based on the local antibiotic resistance. Antibiotic therapy should then be adjusted based on the results of the urine culture. Most uncomplicated cases of acute pyelonephritis will be caused by E. coli for which patients can be treated with oral cephalosporins or TMP-SMX for 14 days. Complicated cases of acute pyelonephritis require intravenous (IV) antibiotic treatment until there are clinical improvements. Examples of IV antibiotics include piperacillin-tazobactam, fluoroquinolones, meropenem, and cefepime. For patients who have allergies to penicillin, vancomycin can be used.
Preventive measures
- Nephrolithiasis:
- Fluid intake: Increase it to optimize urine output to 2-2.5ltr/daily.
- Calcium stones and high urine calcium: Patients should limit sodium intake and maintain a goal of moderate calcium intake of 1-1.2 kg dietary calcium daily.
- Hyperuricosuric calcium stone: Those with calcium stones and low urinary citrate or those with uric acid stones and high urinary uric acid should increase intake of fruits and vegetables and decrease non-dairy animal protein. They may benefit from potassium citrate supplementation and prophylactic allopurinol.
- Recurrent calcium stones and high urinary calcium: Thiazide diuretics are indicated to reduce the amount of urinary calcium.
- Hyperoxaluria: Patients should be encouraged to lower their oxalate intake (spinach, nuts, chocolate, green leafy vegetables).
- Urinary tract infection and Pyelonephritis:
- The key to prevent recurrent episodes is the patient education.
- Fluid intake: It should be increased to maintain vigorous urine flow and avoid dehydration to prevent acute pyelonephritis and improves kidney function.
- Sexually active women: They should try to void right after sexual intercourse as this can help flush the bacteria out of the bladder because bacteria in the bladder can increase by ten-fold after intercourse. After urination, women should wipe from front to back, not from the anal area forward, which seems to drag pathogenic organisms nearer to the urethra.
- Recurrent UTIs: Prophylactic antibiotics should be used.
- Non-medical remedies: The use of cranberry juice and probiotics may help to reduce the severity and frequency of UTI in some women.
References
- ↑ Wolffram, S.; Bisang, B.; Grenacher, B.; Scharrer, E. (1990). "Transport of tri- and dicarboxylic acids across the intestinal brush border membrane of calves". J Nutr. 120 (7): 767–74. PMID 2366111. Unknown parameter
|month=ignored (help) - ↑ Christodoulidou, M.; Thomas, M.; Sharma, SD. (2012). "Hydronephrosis and loin pain as a presentation of tubo-ovarian abscess developing after Mirena coil removal". BMJ Case Rep. 2012. doi:10.1136/bcr-03-2012-6108. PMID 22865801.
- ↑ Smith, HS.; Bajwa, ZH. (2012). "Loin pain hematuria syndrome-visceral or neuropathic pain syndrome?". Clin J Pain. 28 (7): 646–51. doi:10.1097/AJP.0b013e31823d47f3. PMID 22699133. Unknown parameter
|month=ignored (help)