Loin pain hematuria syndrome
| Loin pain hematuria syndrome | |
| Classification and external resources | |
| |
|---|---|
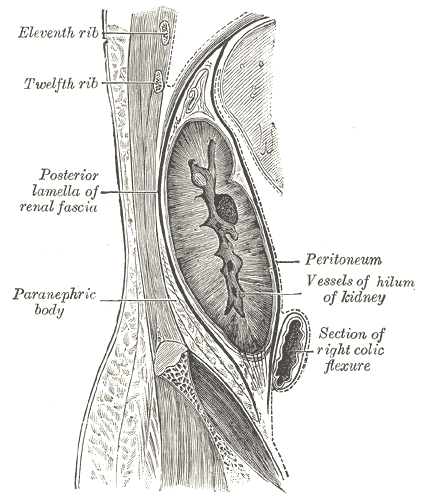
| Sagittal section of the kidney and its capsule. Pain in LPHS is thought to result from distension of the kidney capsule. |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Mugilan Poongkunran M.B.B.S [2]
Synonyms and keywords: LPHS
Overview
Loin pain hematuria syndrome is the combination of unilateral or bilateral flank pain and microscopic or macroscopic amounts of blood in the urine that is otherwise unexplained.[1]
Causes
The cause of LPHS is currently not known.[1] One theory proposes that it is caused by a thin glomerular basement membrane and red blood cell (RBC) renal tubular congestion that leads to swelling of the kidney and distension of the renal fascia resulting in pain.[2]. Loin pain hematuria syndrome is considered a diagnosis of exclusion.
Differentiating Loin Pain Hematuria Syndrome from other Diseases
- Kidney stones
- Nutcracker syndrome
- IgA nephropathy
- Cancer of the genitourinary tract - classically not associated with pain
- Chronic pelvic pain
- Endometriosis
Epidemiology and Demographics
The condition is very rare and predominately affects females. Worldwide, only several hundred cases have been reported.
Natural History, Complications and Prognosis
At this time no cure has been found for this disease. LPHS is a debilitating disease due to chronic pain and the inability to know how to control the glomerular aspect. The pain of LPHS can be worsened by acts as simple as riding in the car and undertaking daily activities.[citation needed] Many people with this disease are unable to maintain employment due to the debilitating pain.[citation needed]
Diagnosis
History and Symptoms
The syndrome presents with hematuria (blood in the urine) and flank (a region of the lower back beneath the ribs and above the ilium) pain which can result from a number of causes. It has considerable overlap with chronic pelvic pain syndrome.
Laboratory Findings
A thin glomerular basement membrane, as in thin basement membrane disease, is proposed to be the characteristic finding on renal biopsy,[2] but not part of the syndrome definition.
Treatment
The treatment of LPHS varies considerably from centre to centre. As the condition is rare and poorly understood, a widely adopted standard of care is not existent.
Medical Therapy
Pain management with opiate and non-opiate analgesia is common. Angiotensin converting enzyme inhibitors are thought to be beneficial,[2] as they reduce intraglomerular pressure and, presumably, reduce renal tubular congestion with RBCs.
Surgery
Surgery (autotransplantation) is thought by some to be of benefit in selected individuals[3] and advocated in some centres, but usually considered the last resort.[4]
Many physicians discourage surgery, as LPHS symptoms often re-occur after autotransplantation.[4]
References
- ↑ 1.0 1.1 Pukenas BA, Zaslau S (2003). "Loin pain hematuria syndrome: case series". W V Med J. 99 (5): 192–3. PMID 14959511.
- ↑ 2.0 2.1 2.2 Hebert LA, Betts JA, Sedmak DD, Cosio FG, Bay WH, Carlton S (1996). "Loin pain-hematuria syndrome associated with thin glomerular basement membrane disease and hemorrhage into renal tubules". Kidney Int. 49 (1): 168–73. doi:10.1038/ki.1996.23. PMID 8770964.
- ↑ Chin JL, Kloth D, Pautler SE, Mulligan M (1998). "Renal autotransplantation for the loin pain-hematuria syndrome: long-term followup of 26 cases". J. Urol. 160 (4): 1232–5, discussion 1235–6. doi:10.1016/S0022-5347(01)62503-5. PMID 9751325.
- ↑ 4.0 4.1 Parnham AP, Low A, Finch P, Perlman D, Thomas MA (1996). "Recurrent graft pain following renal autotransplantation for loin pain haematuria syndrome". Br J Urol. 78 (1): 25–8. PMID 8795395.