Esophageal cancer surgery
|
Esophageal cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Esophageal cancer surgery On the Web |
|
American Roentgen Ray Society Images of Esophageal cancer surgery |
|
Risk calculators and risk factors for Esophageal cancer surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The treatment is determined by the cellular type of cancer (adenocarcinoma or squamous cell carcinoma vs other types), the stage of the disease, the general condition of the patient and other diseases present. On the whole, adequate nutrition needs to be assured, and adequate dental care is vital.
Surgery
Stage 0 esophageal cancer
Stage 0 squamous esophageal cancer is rarely seen in the United States, but surgery has been used for this stage of cancer.
Stage I Esophageal Cancer
Standard treatment options:
- Chemoradiation with subsequent surgery
- Surgery
Stage II Esophageal Cancer
Standard treatment options:
- Chemoradiation with subsequent surgery
- Chemoradiation alone
- Surgery alone
Stage III Esophageal Cancer
Standard treatment options:
- Chemoradiation with subsequent surgery
- Chemoradiation alone
Stage IV Esophageal Cancer
At diagnosis, approximately 50% of patients with esophageal cancer will have metastatic disease and will be candidates for palliative therapy. Standard treatment options:
- Chemoradiation with subsequent surgery (for patients with stage IVA disease)
- Endoscopic-placed stents to provide palliation of dysphagia
- Radiation therapy with or without intraluminal intubation and dilation
- Intraluminal brachytherapy to provide palliation of dysphagia
- Nd:YAG endoluminal tumor destruction or electrocoagulation
- Chemotherapy has provided partial responses for patients with metastatic distal esophageal adenocarcinomas
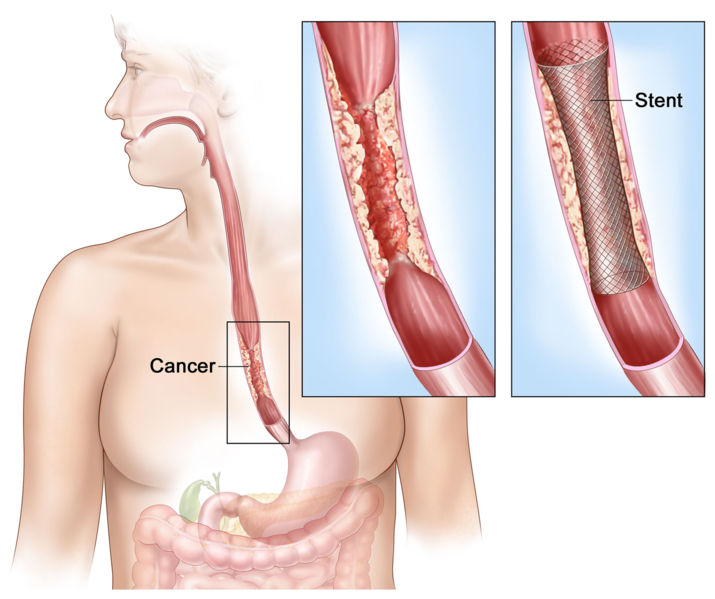
Stenting
If the patient cannot swallow at all, a stent may be inserted to keep the esophagus patent; stents may also assist in occluding fistulas. A nasogastric tube may be necessary to continue feeding while treatment for the tumor is given, and some patients require a gastrostomy (feeding hole in the skin that gives direct access to the stomach). The latter two are especially important if the patient tends to aspirate food or saliva into the airways, predisposing for aspiration pneumonia.
-
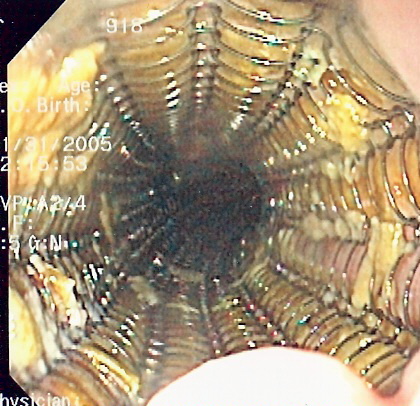
Self-expandable metallic stents are used for the palliation of esophageal cancer
-
Shows cancer blocking esophagus. Insets show enlarged area of cancer and a stent placed in the esophagus to keep it open.
Esophagectomy
Surgery is possible if the disease is localised, which is the case in 20-30% of all patients. If the tumor is larger but localised, chemotherapy and/or radiotherapy may occasionally shrink the tumor to the extent that it becomes "operable"; however, this combination of treatments (referred to as neoadjuvant chemoradiation) is still somewhat controversial in most medical circles. Esophagectomy is the removal of a segment of the esophagus; as this shortens the distance between the throat and the stomach, some other segment of the digestive tract (typically the stomach or part of the colon) is placed in the chest cavity and interposed.[1]
The optimal surgical procedure is controversial. One approach advocates transhiatal esophagectomy with anastomosis of the stomach to the cervical esophagus. A second approach advocates abdominal mobilization of the stomach and transthoracic excision of the esophagus with anastomosis of the stomach to the upper thoracic esophagus or the cervical esophagus.
Laser therapy
Laser therapy is the use of high-intensity light to destroy tumor cells; it affects only the treated area. This is typically done if the cancer cannot be removed by surgery. The relief of a blockage can help to reduce dysphagia and pain. Photodynamic therapy (PDT), a type of laser therapy, involves the use of drugs that are absorbed by cancer cells; when exposed to a special light, the drugs become active and destroy the cancer cells.
Radiotherapy
Radiotherapy is given before, during or after chemotherapy or surgery, and sometimes on its own to control symptoms. In patients with localised disease but contraindications to surgery, "radical radiotherapy" may be used with curative intent.
Other modalities
Radiofrequency ablation (RFA) Argon plasma coagulation Electrocoagulation
Follow-up
Patients are followed up frequently after a treatment regimen has been completed. Frequently, other treatments are necessary to improve symptoms and maximize nutrition.