Endocarditis pathophysiology: Difference between revisions
No edit summary |
|||
| (30 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
{|class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right; | |||
|- | |||
| {{#ev:youtube|https://https://www.youtube.com/watch?v=kW-85yk0ErQ|350}} | |||
|- | |||
|} | |||
__NOTOC__ | __NOTOC__ | ||
{{Infective endocarditis}} | {{Infective endocarditis}} | ||
| Line 5: | Line 11: | ||
==Overview== | ==Overview== | ||
The pathogenesis of infective endocarditis includes valvular damage, altered and turbulent flow, bacteremia, and lack of blood supply to the [[valve]]s. | The pathogenesis of infective endocarditis includes valvular damage, altered and turbulent flow, bacteremia, and lack of blood supply to the [[valve]]s. Damaged endothelium becomes a site for attachment of infectious agents in infectious endocarditis. Nonbacterial thrombotic endocarditis is related to hypercoagulable states such as [[pregnancy]] or systemic bacterial [[infection]]. The characteristic lesion of endocarditis is vegetation. Vegetations are composed of [[fibrin]], inflammatory cells, [[platelets]], and microorganisms. | ||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | |||
====Infective Endocarditis==== | |||
* The pathogenesis of infective endocarditis includes: | |||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 600px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 600px" align=center | ||
|valign=top| | |valign=top| | ||
| Line 42: | Line 48: | ||
|- | |- | ||
|} | |} | ||
====Nonbacterial thrombotic endocarditis==== | ====Nonbacterial Thrombotic Endocarditis==== | ||
* The exact pathogenesis of nonbacterial thrombotic endocarditis is not completely understood. | |||
*[[Nonbacterial thrombotic endocarditis]] (NBTE), also called marantic endocarditis is most commonly found on previously undamaged valves. | |||
*The vegetations in nonbacterial thrombotic endocarditis are sterile and small. | |||
*The vegetations mostly aggregate at the edges of the valve or the cusps. | |||
* We can divide the pathogenesis pathway of nonbacterial endocarditis into to phase: | |||
** Initiating phase | |||
*** Immune complexes:<ref name="pmid3135393">{{cite journal |vauthors=Ford PM, Ford SE, Lillicrap DP |title=Association of lupus anticoagulant with severe valvular heart disease in systemic lupus erythematosus |journal=J. Rheumatol. |volume=15 |issue=4 |pages=597–600 |date=April 1988 |pmid=3135393 |doi= |url=}}</ref><ref>{{cite book | last = Williams | first = Ralph | title = Immune complexes in clinical and experimental medicine | publisher = Harvard University Press | location = Cambridge, Mass | year = 1980 | isbn = 978-0674444386 }}</ref> | |||
****Circulating immune complexes and complement deposition can initiate the process. | |||
****The example for this initiating factor in libman sacks endocarditis in lupus patients. | |||
*** Hypoxia:<ref name="pmid9808440">{{cite journal |vauthors=Nakanishi K, Tajima F, Nakata Y, Osada H, Ogata K, Kawai T, Torikata C, Suga T, Takishima K, Aurues T, Ikeda T |title=Tissue factor is associated with the nonbacterial thrombotic endocarditis induced by a hypobaric hypoxic environment in rats |journal=Virchows Arch. |volume=433 |issue=4 |pages=375–9 |date=October 1998 |pmid=9808440 |doi=10.1007/s004280050262 |url=}}</ref><ref name="pmid11355169">{{cite journal |vauthors=Truskinovsky AM, Hutchins GM |title=Association between nonbacterial thrombotic endocarditis and hypoxigenic pulmonary diseases |journal=Virchows Arch. |volume=438 |issue=4 |pages=357–61 |date=April 2001 |pmid=11355169 |doi=10.1007/s004280000372 |url=}}</ref> | |||
****Some studies demonstrated that hypoxia may lead to tissue factor activation. | |||
****Higher tissue factor level has an association with higher rate of endocarditis. | |||
****Other studies implies that the rate of endocarditis is higher in smokers and patients with chronic lung disease and possibly hypoxia. | |||
*** Hypercoagulability:<ref name="pmid13403513">{{cite journal |vauthors=MACDONALD RA, ROBBINS SL |title=The significance of nonbacterial thrombotic endocarditis: an autopsy and clinical study of 78 cases |journal=Ann. Intern. Med. |volume=46 |issue=2 |pages=255–73 |date=February 1957 |pmid=13403513 |doi=10.7326/0003-4819-46-2-255 |url=}}</ref><ref name="pmid834136">{{cite journal |vauthors=Sack GH, Levin J, Bell WR |title=Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic, and therapeutic features |journal=Medicine (Baltimore) |volume=56 |issue=1 |pages=1–37 |date=January 1977 |pmid=834136 |doi= |url=}}</ref> | |||
****There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis. | |||
***** | |||
*** Carcinomatosis:<ref name="pmid4577065">{{cite journal |vauthors=Gralnick HR, Abrell E |title=Studies of the procoagulant and fibrinolytic activity of promyelocytes in acute promyelocytic leukaemia |journal=Br. J. Haematol. |volume=24 |issue=1 |pages=89–99 |date=January 1973 |pmid=4577065 |doi=10.1111/j.1365-2141.1973.tb05730.x |url=}}</ref> | |||
****The association between cancer and nonbacterial thrombotic endocarditis is well established. | |||
****In most of the cases of cancer related endocarditis we have abnormal activity of tissue factor. | |||
****Tissue factor may be secreted from promyelocytic leukaemia cells. | |||
****Tissue factor may be expressed on the surface of adenocarcinoma cells which leads to increased expression of tissue factor by endothelial cells. | |||
***** | |||
** Verrucae formation | |||
== Genetics == | |||
Genes involved in the pathogenesis of infective endocarditis include:<ref name="pmid25299518">{{cite journal |vauthors=Weinstock M, Grimm I, Dreier J, Knabbe C, Vollmer T |title=Genetic variants in genes of the inflammatory response in association with infective endocarditis |journal=PLoS ONE |volume=9 |issue=10 |pages=e110151 |date=2014 |pmid=25299518 |pmc=4192365 |doi=10.1371/journal.pone.0110151 |url=}}</ref> | |||
* Interleukin-6 c.471+870G>A | |||
* Interleukin-1b c.315C>T | |||
* Selectin-E c.-19 GT | |||
[[ | Genes involved in the pathogenesis of nonbacterial thrombotic [[endocarditis]] include:<ref name="pmid21560828">{{cite journal |vauthors=Durante-Mangoni E, Iossa D, Nappi F, Utili R |title=Inherited hyper-homocysteinemia as a cause of nonbacterial thrombotic endocarditis |journal=J. Heart Valve Dis. |volume=20 |issue=2 |pages=232–3 |date=March 2011 |pmid=21560828 |doi= |url=}}</ref> | ||
* Homozygous for the C677T mutation of the [[Methylenetetrahydrofolate-tRNA-(uracil-5-)-methyltransferase|methylenetetrahydrofolate]] reductase gene which leads to [[hyperhomocysteinemia]]. | |||
* | |||
== Associated Conditions == | |||
{| {{table}} | Conditions associated with [[endocarditis]] include: | ||
*[[Prosthetic heart valve]]s<ref name="pmid3272238">{{cite journal |vauthors=Arvay A, Lengyel M |title=Incidence and risk factors of prosthetic valve endocarditis |journal=Eur J Cardiothorac Surg |volume=2 |issue=5 |pages=340–6 |date=1988 |pmid=3272238 |doi= |url=}}</ref> | |||
*Valvular heart disease ([[mitral valve prolapse]] is the most common valvular lesion that predisposes to endocarditis)<ref name="pmid117941522">{{cite journal| author=Mylonakis E, Calderwood SB| title=Infective endocarditis in adults. | journal=N Engl J Med | year= 2001 | volume= 345 | issue= 18 | pages= 1318-30 | pmid=11794152 | doi=10.1056/NEJMra010082 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11794152 }}</ref><ref name="CorrigallBolen1977">{{cite journal|last1=Corrigall|first1=Denton|last2=Bolen|first2=James|last3=Hancock|first3=E.William|last4=Popp|first4=Richard L.|title=Mitral valve prolapse and infective endocarditis|journal=The American Journal of Medicine|volume=63|issue=2|year=1977|pages=215–222|issn=00029343|doi=10.1016/0002-9343(77)90235-2}}</ref> | |||
*[[Intravenous]] drug abuse<ref name="SousaBotelho2012">{{cite journal|last1=Sousa|first1=C.|last2=Botelho|first2=C.|last3=Rodrigues|first3=D.|last4=Azeredo|first4=J.|last5=Oliveira|first5=R.|title=Infective endocarditis in intravenous drug abusers: an update|journal=European Journal of Clinical Microbiology & Infectious Diseases|volume=31|issue=11|year=2012|pages=2905–2910|issn=0934-9723|doi=10.1007/s10096-012-1675-x}}</ref> | |||
*Intracardiac devices, such as [[implantable cardioverter-defibrillators]]<ref name="SohailUslan2008">{{cite journal|last1=Sohail|first1=Muhammad R.|last2=Uslan|first2=Daniel Z.|last3=Khan|first3=Akbar H.|last4=Friedman|first4=Paul A.|last5=Hayes|first5=David L.|last6=Wilson|first6=Walter R.|last7=Steckelberg|first7=James M.|last8=Jenkins|first8=Sarah M.|last9=Baddour|first9=Larry M.|title=Infective Endocarditis Complicating Permanent Pacemaker and Implantable Cardioverter-Defibrillator Infection|journal=Mayo Clinic Proceedings|volume=83|issue=1|year=2008|pages=46–53|issn=00256196|doi=10.4065/83.1.46}}</ref> | |||
*[[Hemodialysis]]<ref name="MccarthySteckelberg2000">{{cite journal|last1=Mccarthy|first1=James T.|last2=Steckelberg|first2=James M.|title=Infective Endocarditis in Patients Receiving Long-term Hemodialysis|journal=Mayo Clinic Proceedings|volume=75|issue=10|year=2000|pages=1008–1014|issn=00256196|doi=10.4065/75.10.1008}}</ref> | |||
*[[Congenital heart disease]]<ref name="KnirschNadal2011">{{cite journal|last1=Knirsch|first1=Walter|last2=Nadal|first2=David|title=Infective endocarditis in congenital heart disease|journal=European Journal of Pediatrics|volume=170|issue=9|year=2011|pages=1111–1127|issn=0340-6199|doi=10.1007/s00431-011-1520-8}}</ref> | |||
*History of [[rheumatic heart disease]]<ref name="pmid9841581">{{cite journal |vauthors=Strom BL, Abrutyn E, Berlin JA, Kinman JL, Feldman RS, Stolley PD, Levison ME, Korzeniowski OM, Kaye D |title=Dental and cardiac risk factors for infective endocarditis. A population-based, case-control study |journal=Ann. Intern. Med. |volume=129 |issue=10 |pages=761–9 |date=November 1998 |pmid=9841581 |doi=10.7326/0003-4819-129-10-199811150-00002 |url=}}</ref> | |||
*[[Diabetes mellitus]]<ref name="pmid31242695">{{cite journal |vauthors=Lin CJ, Chua S, Chung SY, Hang CL, Tsai TH |title=Diabetes Mellitus: An Independent Risk Factor of In-Hospital Mortality in Patients with Infective Endocarditis in a New Era of Clinical Practice |journal=Int J Environ Res Public Health |volume=16 |issue=12 |pages= |date=June 2019 |pmid=31242695 |pmc=6617149 |doi=10.3390/ijerph16122248 |url=}}</ref><ref name="pmid20583393">{{cite journal |vauthors=Chirillo F, Bacchion F, Pedrocco A, Scotton P, De Leo A, Rocco F, Valfrè C, Olivari Z |title=Infective endocarditis in patients with diabetes mellitus |journal=J. Heart Valve Dis. |volume=19 |issue=3 |pages=312–20 |date=May 2010 |pmid=20583393 |doi= |url=}}</ref> | |||
*[[Colon cancer]]<ref name="LazarovitchShango2012">{{cite journal|last1=Lazarovitch|first1=T.|last2=Shango|first2=M.|last3=Levine|first3=M.|last4=Brusovansky|first4=R.|last5=Akins|first5=R.|last6=Hayakawa|first6=K.|last7=Lephart|first7=P. R.|last8=Sobel|first8=J. D.|last9=Kaye|first9=K. S.|last10=Marchaim|first10=D.|title=The relationship between the new taxonomy of Streptococcus bovis and its clonality to colon cancer, endocarditis, and biliary disease|journal=Infection|volume=41|issue=2|year=2012|pages=329–337|issn=0300-8126|doi=10.1007/s15010-012-0314-x}}</ref> | |||
*[[Hypercoagulable state]] such as [[pregnancy]] and systemic bacterial infection <ref>{{cite journal|title=THE SIGNIFICANCE OF NONBACTERIAL THROMBOTIC ENDOCARDITIS: AN AUTOPSY AND CLINICAL STUDY OF 78 CASES|journal=Annals of Internal Medicine|volume=46|issue=2|year=1957|pages=255|issn=0003-4819|doi=10.7326/0003-4819-46-2-255}}</ref><ref name="HorwitzWard1971">{{cite journal|last1=Horwitz|first1=Charles A.|last2=Ward|first2=Patrick C.J.|title=Disseminated intravascular coagulation, nonbacterial thrombotic endocarditis and adult pulmonary hyaline membranes-an interrelated triad?|journal=The American Journal of Medicine|volume=51|issue=2|year=1971|pages=272–280|issn=00029343|doi=10.1016/0002-9343(71)90245-2}}</ref> | |||
*[[Malignancy]] especially mucin-producing [[adenocarcinoma]]s (most commonly associated with pancreatic adenocarcinomas)<ref name="MinGyorkey1980">{{cite journal|last1=Min|first1=Kyung-Whan|last2=Gyorkey|first2=Ferene|last3=Sato|first3=Clifford|title=Mucin-producing adenocarcinomas and nonbacterial thrombotic endocarditis. Pathogenetic role of tumor mucin|journal=Cancer|volume=45|issue=9|year=1980|pages=2374–2382|issn=0008-543X|doi=10.1002/1097-0142(19800501)45:9<2374::AID-CNCR2820450923>3.0.CO;2-J}}</ref> | |||
*[[Systemic lupus erythematosus]]<ref name="MoyssakisTektonidou2007">{{cite journal|last1=Moyssakis|first1=Ioannis|last2=Tektonidou|first2=Maria G.|last3=Vasilliou|first3=Vassilios A.|last4=Samarkos|first4=Michael|last5=Votteas|first5=Vassilios|last6=Moutsopoulos|first6=Haralampos M.|title=Libman-Sacks Endocarditis in Systemic Lupus Erythematosus: Prevalence, Associations, and Evolution|journal=The American Journal of Medicine|volume=120|issue=7|year=2007|pages=636–642|issn=00029343|doi=10.1016/j.amjmed.2007.01.024}}</ref> | |||
== Gross Pathology == | |||
On gross pathology, characteristic findings of endocarditis are: | |||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Endocarditis Subtype'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Endocarditis Subtype'''}} | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | ||
|- | |- | ||
| Infective Endocarditis|| | ! style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Infective Endocarditis | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Left-sided valve involvement (mitral, aortic) more common generally | *Left-sided valve involvement (mitral, aortic) more common generally | ||
*Right-sided valve involvement (pulmonic, tricuspid valve) more common in intravenous drug abusers | *Right-sided valve involvement (pulmonic, tricuspid valve) more common in intravenous drug abusers | ||
*Valvular vegetations | *Valvular vegetations | ||
*Valvular destruction | *Valvular destruction | ||
| | |- | ||
! style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Nonbacterial Thrombotic Endocarditis | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Round non-destructive vegetations, usually at the line of closure | |||
|- | |||
|} | |||
== Microscopic Pathology == | |||
On microscopic histopathological, characteristic findings of endocarditis are: | |||
* Vegetation: | |||
** Vegetations are composed of fibrin, inflammatory cells, platelets, and microorganisms.<ref name="pmid11794152">{{cite journal| author=Mylonakis E, Calderwood SB| title=Infective endocarditis in adults. | journal=N Engl J Med | year= 2001 | volume= 345 | issue= 18 | pages= 1318-30 | pmid=11794152 | doi=10.1056/NEJMra010082 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11794152 }}</ref> | |||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | |||
| align="center" style="background: #4479BA;" |{{fontcolor|#FFF|'''Endocarditis Subtype'''}} | |||
| align="center" style="background: #4479BA;" |{{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Infective Endocarditis | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Inflammatory infiltrate | *Inflammatory infiltrate | ||
*Abundant neutrophils | *Abundant neutrophils | ||
| Line 65: | Line 139: | ||
*Microorganisms present | *Microorganisms present | ||
|- | |- | ||
| Nonbacterial Thrombotic Endocarditis| | ! style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | Nonbacterial Thrombotic Endocarditis | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
*Vegetations without inflammation and microorganisms | *Vegetations without inflammation and microorganisms | ||
|- | |- | ||
|} | |} | ||
[http://www.peir.net Image courtesy of Professor Peter Anderson DVM Ph.D. and published with permission © PEIR, the University of Alabama at Birmingham, Department of Pathology] | |||
[http://www.peir.net Image courtesy of Professor Peter Anderson DVM | |||
<div align="left"> | <div align="left"><gallery heights="150" widths="150"> | ||
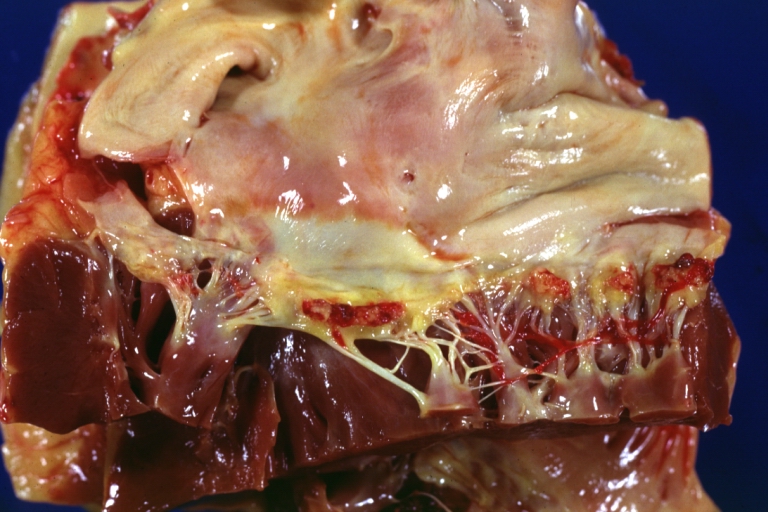
<gallery heights="150" widths="150"> | Image: Breast intraductal papilloma metastasis.jpg|Heart; Breast intraductal papilloma metastasis. Thrombotic Nonbacterial Endocarditis (Infected): Gross mitral valve natural color vegetations well-illustrated these were secondarily infected with staphylococcus case of 8-year survival breast intraductal papillary adenocarcinoma with extensive metastases. Aortic valve also involved. | ||
Image:Breast intraductal papilloma metastasis.jpg|Heart; Breast intraductal papilloma metastasis. Thrombotic Nonbacterial Endocarditis (Infected): Gross mitral valve natural color vegetations well illustrated these were secondarily infected with staphylococcus case of 8 year survival breast intraductal papillary adenocarcinoma with extensive metastases. Aortic valve also involved. | Image: Papillar intraductal carcinoma metastasis to heart.JPG|Nonbacterial Thrombotic Endocarditis Infected: Micro low mag H&E fibrin vegetation with masses of staphylococci and inflammatory cells in valve secondarily infected case 8-year survival breast papillary intraductal adenocarcinoma with extensive metastases gross is aortic valve lesions. | ||
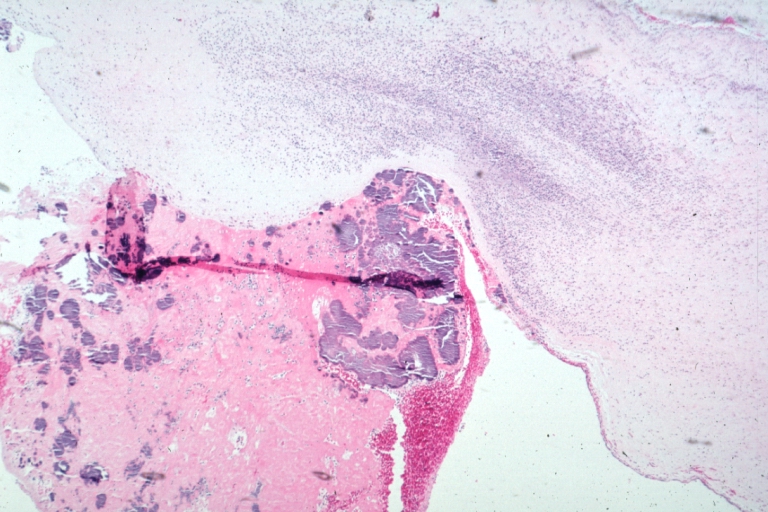
Image:Papillar intraductal carcinoma metastasis to heart.JPG|Nonbacterial Thrombotic Endocarditis Infected: Micro low mag H&E fibrin vegetation with masses of staphylococci and inflammatory cells in valve secondarily infected case 8 year survival breast papillary intraductal adenocarcinoma with extensive metastases gross is aortic valve lesions. | |||
</gallery> | </gallery> | ||
</div> | </div> | ||
==Videos== | ==Videos== | ||
{{#ev:youtube|gk7cpP2ymOs}} | {{#ev:youtube|gk7cpP2ymOs}} {{#ev:youtube|BiNulEFh6rU}} | ||
{{#ev:youtube|BiNulEFh6rU}} | |||
==References== | ==References== | ||
| Line 92: | Line 161: | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Intensive care medicine]] | [[Category:Intensive care medicine]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
Latest revision as of 02:24, 6 March 2020
| https://https://www.youtube.com/watch?v=kW-85yk0ErQ%7C350}} |
|
Endocarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease |
|
Case Studies |
|
Endocarditis pathophysiology On the Web |
|
Risk calculators and risk factors for Endocarditis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maliha Shakil, M.D. [2]
Overview
The pathogenesis of infective endocarditis includes valvular damage, altered and turbulent flow, bacteremia, and lack of blood supply to the valves. Damaged endothelium becomes a site for attachment of infectious agents in infectious endocarditis. Nonbacterial thrombotic endocarditis is related to hypercoagulable states such as pregnancy or systemic bacterial infection. The characteristic lesion of endocarditis is vegetation. Vegetations are composed of fibrin, inflammatory cells, platelets, and microorganisms.
Pathophysiology
Pathogenesis
Infective Endocarditis
- The pathogenesis of infective endocarditis includes:
| Pathogenic Factors | Mechanism |
|---|---|
|
|
|
|
|
|
Nonbacterial Thrombotic Endocarditis
- The exact pathogenesis of nonbacterial thrombotic endocarditis is not completely understood.
- Nonbacterial thrombotic endocarditis (NBTE), also called marantic endocarditis is most commonly found on previously undamaged valves.
- The vegetations in nonbacterial thrombotic endocarditis are sterile and small.
- The vegetations mostly aggregate at the edges of the valve or the cusps.
- We can divide the pathogenesis pathway of nonbacterial endocarditis into to phase:
- Initiating phase
- Immune complexes:[1][2]
- Circulating immune complexes and complement deposition can initiate the process.
- The example for this initiating factor in libman sacks endocarditis in lupus patients.
- Hypoxia:[3][4]
- Some studies demonstrated that hypoxia may lead to tissue factor activation.
- Higher tissue factor level has an association with higher rate of endocarditis.
- Other studies implies that the rate of endocarditis is higher in smokers and patients with chronic lung disease and possibly hypoxia.
- Hypercoagulability:[5][6]
- There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis.
- There is an association between hypercoagulable state and clotting factor abnormalities with initiation of nonbacterial thrombotic endocarditis.
- Carcinomatosis:[7]
- The association between cancer and nonbacterial thrombotic endocarditis is well established.
- In most of the cases of cancer related endocarditis we have abnormal activity of tissue factor.
- Tissue factor may be secreted from promyelocytic leukaemia cells.
- Tissue factor may be expressed on the surface of adenocarcinoma cells which leads to increased expression of tissue factor by endothelial cells.
- Immune complexes:[1][2]
- Verrucae formation
- Initiating phase
Genetics
Genes involved in the pathogenesis of infective endocarditis include:[8]
- Interleukin-6 c.471+870G>A
- Interleukin-1b c.315C>T
- Selectin-E c.-19 GT
Genes involved in the pathogenesis of nonbacterial thrombotic endocarditis include:[9]
- Homozygous for the C677T mutation of the methylenetetrahydrofolate reductase gene which leads to hyperhomocysteinemia.
Associated Conditions
Conditions associated with endocarditis include:
- Prosthetic heart valves[10]
- Valvular heart disease (mitral valve prolapse is the most common valvular lesion that predisposes to endocarditis)[11][12]
- Intravenous drug abuse[13]
- Intracardiac devices, such as implantable cardioverter-defibrillators[14]
- Hemodialysis[15]
- Congenital heart disease[16]
- History of rheumatic heart disease[17]
- Diabetes mellitus[18][19]
- Colon cancer[20]
- Hypercoagulable state such as pregnancy and systemic bacterial infection [21][22]
- Malignancy especially mucin-producing adenocarcinomas (most commonly associated with pancreatic adenocarcinomas)[23]
- Systemic lupus erythematosus[24]
Gross Pathology
On gross pathology, characteristic findings of endocarditis are:
| Endocarditis Subtype | Features on Gross Pathology |
| Infective Endocarditis |
|
|---|---|
| Nonbacterial Thrombotic Endocarditis |
|
Microscopic Pathology
On microscopic histopathological, characteristic findings of endocarditis are:
- Vegetation:
- Vegetations are composed of fibrin, inflammatory cells, platelets, and microorganisms.[25]
| Endocarditis Subtype | Features on Histopathological Microscopic Analysis |
| Infective Endocarditis |
|
|---|---|
| Nonbacterial Thrombotic Endocarditis |
|
-
Heart; Breast intraductal papilloma metastasis. Thrombotic Nonbacterial Endocarditis (Infected): Gross mitral valve natural color vegetations well-illustrated these were secondarily infected with staphylococcus case of 8-year survival breast intraductal papillary adenocarcinoma with extensive metastases. Aortic valve also involved.
-
Nonbacterial Thrombotic Endocarditis Infected: Micro low mag H&E fibrin vegetation with masses of staphylococci and inflammatory cells in valve secondarily infected case 8-year survival breast papillary intraductal adenocarcinoma with extensive metastases gross is aortic valve lesions.
Videos
{{#ev:youtube|gk7cpP2ymOs}} {{#ev:youtube|BiNulEFh6rU}}
References
- ↑ Ford PM, Ford SE, Lillicrap DP (April 1988). "Association of lupus anticoagulant with severe valvular heart disease in systemic lupus erythematosus". J. Rheumatol. 15 (4): 597–600. PMID 3135393.
- ↑ Williams, Ralph (1980). Immune complexes in clinical and experimental medicine. Cambridge, Mass: Harvard University Press. ISBN 978-0674444386.
- ↑ Nakanishi K, Tajima F, Nakata Y, Osada H, Ogata K, Kawai T, Torikata C, Suga T, Takishima K, Aurues T, Ikeda T (October 1998). "Tissue factor is associated with the nonbacterial thrombotic endocarditis induced by a hypobaric hypoxic environment in rats". Virchows Arch. 433 (4): 375–9. doi:10.1007/s004280050262. PMID 9808440.
- ↑ Truskinovsky AM, Hutchins GM (April 2001). "Association between nonbacterial thrombotic endocarditis and hypoxigenic pulmonary diseases". Virchows Arch. 438 (4): 357–61. doi:10.1007/s004280000372. PMID 11355169.
- ↑ MACDONALD RA, ROBBINS SL (February 1957). "The significance of nonbacterial thrombotic endocarditis: an autopsy and clinical study of 78 cases". Ann. Intern. Med. 46 (2): 255–73. doi:10.7326/0003-4819-46-2-255. PMID 13403513.
- ↑ Sack GH, Levin J, Bell WR (January 1977). "Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasms: clinical, pathophysiologic, and therapeutic features". Medicine (Baltimore). 56 (1): 1–37. PMID 834136.
- ↑ Gralnick HR, Abrell E (January 1973). "Studies of the procoagulant and fibrinolytic activity of promyelocytes in acute promyelocytic leukaemia". Br. J. Haematol. 24 (1): 89–99. doi:10.1111/j.1365-2141.1973.tb05730.x. PMID 4577065.
- ↑ Weinstock M, Grimm I, Dreier J, Knabbe C, Vollmer T (2014). "Genetic variants in genes of the inflammatory response in association with infective endocarditis". PLoS ONE. 9 (10): e110151. doi:10.1371/journal.pone.0110151. PMC 4192365. PMID 25299518.
- ↑ Durante-Mangoni E, Iossa D, Nappi F, Utili R (March 2011). "Inherited hyper-homocysteinemia as a cause of nonbacterial thrombotic endocarditis". J. Heart Valve Dis. 20 (2): 232–3. PMID 21560828.
- ↑ Arvay A, Lengyel M (1988). "Incidence and risk factors of prosthetic valve endocarditis". Eur J Cardiothorac Surg. 2 (5): 340–6. PMID 3272238.
- ↑ Mylonakis E, Calderwood SB (2001). "Infective endocarditis in adults". N Engl J Med. 345 (18): 1318–30. doi:10.1056/NEJMra010082. PMID 11794152.
- ↑ Corrigall, Denton; Bolen, James; Hancock, E.William; Popp, Richard L. (1977). "Mitral valve prolapse and infective endocarditis". The American Journal of Medicine. 63 (2): 215–222. doi:10.1016/0002-9343(77)90235-2. ISSN 0002-9343.
- ↑ Sousa, C.; Botelho, C.; Rodrigues, D.; Azeredo, J.; Oliveira, R. (2012). "Infective endocarditis in intravenous drug abusers: an update". European Journal of Clinical Microbiology & Infectious Diseases. 31 (11): 2905–2910. doi:10.1007/s10096-012-1675-x. ISSN 0934-9723.
- ↑ Sohail, Muhammad R.; Uslan, Daniel Z.; Khan, Akbar H.; Friedman, Paul A.; Hayes, David L.; Wilson, Walter R.; Steckelberg, James M.; Jenkins, Sarah M.; Baddour, Larry M. (2008). "Infective Endocarditis Complicating Permanent Pacemaker and Implantable Cardioverter-Defibrillator Infection". Mayo Clinic Proceedings. 83 (1): 46–53. doi:10.4065/83.1.46. ISSN 0025-6196.
- ↑ Mccarthy, James T.; Steckelberg, James M. (2000). "Infective Endocarditis in Patients Receiving Long-term Hemodialysis". Mayo Clinic Proceedings. 75 (10): 1008–1014. doi:10.4065/75.10.1008. ISSN 0025-6196.
- ↑ Knirsch, Walter; Nadal, David (2011). "Infective endocarditis in congenital heart disease". European Journal of Pediatrics. 170 (9): 1111–1127. doi:10.1007/s00431-011-1520-8. ISSN 0340-6199.
- ↑ Strom BL, Abrutyn E, Berlin JA, Kinman JL, Feldman RS, Stolley PD, Levison ME, Korzeniowski OM, Kaye D (November 1998). "Dental and cardiac risk factors for infective endocarditis. A population-based, case-control study". Ann. Intern. Med. 129 (10): 761–9. doi:10.7326/0003-4819-129-10-199811150-00002. PMID 9841581.
- ↑ Lin CJ, Chua S, Chung SY, Hang CL, Tsai TH (June 2019). "Diabetes Mellitus: An Independent Risk Factor of In-Hospital Mortality in Patients with Infective Endocarditis in a New Era of Clinical Practice". Int J Environ Res Public Health. 16 (12). doi:10.3390/ijerph16122248. PMC 6617149 Check
|pmc=value (help). PMID 31242695. - ↑ Chirillo F, Bacchion F, Pedrocco A, Scotton P, De Leo A, Rocco F, Valfrè C, Olivari Z (May 2010). "Infective endocarditis in patients with diabetes mellitus". J. Heart Valve Dis. 19 (3): 312–20. PMID 20583393.
- ↑ Lazarovitch, T.; Shango, M.; Levine, M.; Brusovansky, R.; Akins, R.; Hayakawa, K.; Lephart, P. R.; Sobel, J. D.; Kaye, K. S.; Marchaim, D. (2012). "The relationship between the new taxonomy of Streptococcus bovis and its clonality to colon cancer, endocarditis, and biliary disease". Infection. 41 (2): 329–337. doi:10.1007/s15010-012-0314-x. ISSN 0300-8126.
- ↑ "THE SIGNIFICANCE OF NONBACTERIAL THROMBOTIC ENDOCARDITIS: AN AUTOPSY AND CLINICAL STUDY OF 78 CASES". Annals of Internal Medicine. 46 (2): 255. 1957. doi:10.7326/0003-4819-46-2-255. ISSN 0003-4819.
- ↑ Horwitz, Charles A.; Ward, Patrick C.J. (1971). "Disseminated intravascular coagulation, nonbacterial thrombotic endocarditis and adult pulmonary hyaline membranes-an interrelated triad?". The American Journal of Medicine. 51 (2): 272–280. doi:10.1016/0002-9343(71)90245-2. ISSN 0002-9343.
- ↑ Min, Kyung-Whan; Gyorkey, Ferene; Sato, Clifford (1980). "Mucin-producing adenocarcinomas and nonbacterial thrombotic endocarditis. Pathogenetic role of tumor mucin". Cancer. 45 (9): 2374–2382. doi:10.1002/1097-0142(19800501)45:9<2374::AID-CNCR2820450923>3.0.CO;2-J. ISSN 0008-543X.
- ↑ Moyssakis, Ioannis; Tektonidou, Maria G.; Vasilliou, Vassilios A.; Samarkos, Michael; Votteas, Vassilios; Moutsopoulos, Haralampos M. (2007). "Libman-Sacks Endocarditis in Systemic Lupus Erythematosus: Prevalence, Associations, and Evolution". The American Journal of Medicine. 120 (7): 636–642. doi:10.1016/j.amjmed.2007.01.024. ISSN 0002-9343.
- ↑ Mylonakis E, Calderwood SB (2001). "Infective endocarditis in adults". N Engl J Med. 345 (18): 1318–30. doi:10.1056/NEJMra010082. PMID 11794152.