Cough resident survival guide: Difference between revisions
Sara Haddadi (talk | contribs) |
|||
| (175 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="width: 90%;"> | <div style="width: 90%;"> | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}}; {{AE}} {{SaraH}} | {{CMG}}; {{AE}} {{SaraH}} {{Sara.Zand}} | ||
<div style="width: 1px; height: 1px; background-color: #999999; position: fixed; top: 10px; left: 10px"></div> | <div style="width: 1px; height: 1px; background-color: #999999; position: fixed; top: 10px; left: 10px"></div> | ||
| Line 24: | Line 24: | ||
==Overview== | ==Overview== | ||
[[Cough]] is a defense mechanism for preventation of [[airway]] [[irritation]] or [[aspiration ]] by cleaning excessive secretion or [[foreign body]] from the [[airway]] and also it may spread [[infection]]. [[Cough]] is the [[symptom]] of involving [[organs]] such as [[upper airway tract]], [[lung]], [[heart]], or [[gastrointestinal tract]]. Dependent on the [[duration]] of [[cough]], it can be categorized to three groups including [[acute]], [[subacute]], [[chronic]]. Acute [[cough]] is the most common causes of seeking medical attention every year. Chronic [[cough]] may affect the quality of life and also may increase [[mortality]] based on the underlying [[disorder]]. Assessment of the [[life threatening]] causes of [[cough]] such as [[ obstructive airway disease]] or [[pulmonary embolism]] is of important. | |||
==Causes== | ==Causes== | ||
===Common Causes=== | ===Common Causes=== | ||
* [[Allergic Rhinitis]] | * [[Allergic Rhinitis]] | ||
* [[Asthma]] | * [[Asthma]]<ref name="pmid11716169">{{cite journal |vauthors=Janson C, Chinn S, Jarvis D, Burney P |title=Determinants of cough in young adults participating in the European Community Respiratory Health Survey |journal=Eur Respir J |volume=18 |issue=4 |pages=647–54 |date=October 2001 |pmid=11716169 |doi=10.1183/09031936.01.00098701 |url=}}</ref> | ||
* [[ | * [[Bronchitis]]<ref name="pmid23204254">{{cite journal |vauthors=Kim V, Criner GJ |title=Chronic bronchitis and chronic obstructive pulmonary disease |journal=Am J Respir Crit Care Med |volume=187 |issue=3 |pages=228–37 |date=February 2013 |pmid=23204254 |pmc=4951627 |doi=10.1164/rccm.201210-1843CI |url=}}</ref> | ||
* [[Gastroesophageal Reflux Disease]] ([[GERD]]) | * [[Gastroesophageal Reflux Disease]] ([[GERD]]) | ||
* [[Post-nasal drip]] | * [[Post-nasal drip]]<ref name="pmid22577385">{{cite journal |vauthors=Sylvester DC, Karkos PD, Vaughan C, Johnston J, Dwivedi RC, Atkinson H, Kortequee S |title=Chronic cough, reflux, postnasal drip syndrome, and the otolaryngologist |journal=Int J Otolaryngol |volume=2012 |issue= |pages=564852 |date=2012 |pmid=22577385 |pmc=3332192 |doi=10.1155/2012/564852 |url=}}</ref> | ||
* | * [[Foreign body aspiration]]<ref name="AkelmaCizmeci2013">{{cite journal|last1=Akelma|first1=Ahmet Zulfikar|last2=Cizmeci|first2=Mehmet Nevzat|last3=Kanburoglu|first3=Mehmet Kenan|last4=Mete|first4=Emin|title=An Overlooked Cause of Cough in Children: Foreign Body Aspiration|journal=The Journal of Pediatrics|volume=163|issue=1|year=2013|pages=292–293|issn=00223476|doi=10.1016/j.jpeds.2012.12.089}}</ref> | ||
*[[ACE inhibitor|ACE inhibitors]]<ref name="pmid30664425">{{cite journal |vauthors=Yılmaz İ |title=Angiotensin-Converting Enzyme Inhibitors Induce Cough |journal=Turk Thorac J |volume=20 |issue=1 |pages=36–42 |date=January 2019 |pmid=30664425 |pmc=6340691 |doi=10.5152/TurkThoracJ.2018.18014 |url=}}</ref> | |||
*[[ | *[[Bronchiectasis]]<ref name="pmid31176801">{{cite journal |vauthors=Mac Aogáin M, Chotirmall SH |title=Bronchiectasis and cough: An old relationship in need of renewed attention |journal=Pulm Pharmacol Ther |volume=57 |issue= |pages=101812 |date=August 2019 |pmid=31176801 |pmc=7110869 |doi=10.1016/j.pupt.2019.101812 |url=}}</ref> | ||
*[[Laryngopharyngeal reflux disease|Laryngopharyngeal reflux]] | *[[Laryngopharyngeal reflux disease|Laryngopharyngeal reflux]]<ref name="pmid30364386">{{cite journal |vauthors=Patel DA, Blanco M, Vaezi MF |title=Laryngopharyngeal Reflux and Functional Laryngeal Disorder: Perspective and Common Practice of the General Gastroenterologist |journal=Gastroenterol Hepatol (N Y) |volume=14 |issue=9 |pages=512–520 |date=September 2018 |pmid=30364386 |pmc=6194652 |doi= |url=}}</ref> | ||
*[[Respiratory tract infection]] | *[[Respiratory tract infection]]<ref name="pmid25383204">{{cite journal |vauthors=Dicpinigaitis PV |title=Effect of viral upper respiratory tract infection on cough reflex sensitivity |journal=J Thorac Dis |volume=6 |issue=Suppl 7 |pages=S708–11 |date=October 2014 |pmid=25383204 |pmc=4222932 |doi=10.3978/j.issn.2072-1439.2013.12.02 |url=}}</ref> | ||
*[[Lung cancer]] | *[[Lung cancer]]<ref name="HarleMolassiotis2020">{{cite journal|last1=Harle|first1=Amélie|last2=Molassiotis|first2=Alex|last3=Buffin|first3=Oliver|last4=Burnham|first4=Jack|last5=Smith|first5=Jaclyn|last6=Yorke|first6=Janelle|last7=Blackhall|first7=Fiona H.|title=A cross sectional study to determine the prevalence of cough and its impact in patients with lung cancer: a patient unmet need|journal=BMC Cancer|volume=20|issue=1|year=2020|issn=1471-2407|doi=10.1186/s12885-019-6451-1}}</ref> | ||
* | *Non-[[asthmatic]] [[eosinophilic]] [[bronchitis]]<ref name="pmid29404185">{{cite journal |vauthors=Yıldız T, Dülger S |title=Non-astmatic Eosinophilic Bronchitis |journal=Turk Thorac J |volume=19 |issue=1 |pages=41–45 |date=January 2018 |pmid=29404185 |pmc=5783052 |doi=10.5152/TurkThoracJ.2017.17017 |url=}}</ref> | ||
*Non-[[acid reflux disease]]<ref name="QiuXu2015">{{cite journal|last1=Qiu|first1=Zhongmin|last2=Xu|first2=Xianghuai|last3=Yu|first3=Li|last4=Chen|first4=Qiang|last5=Lv|first5=Hanjing|title=Diagnosis and treatment of patients with nonacid gastroesophageal reflux-induced chronic cough|journal=Journal of Research in Medical Sciences|volume=20|issue=9|year=2015|pages=885|issn=1735-1995|doi=10.4103/1735-1995.170625}}</ref> | |||
*[[Swallowing]] disorder<ref name="pmid25991980">{{cite journal |vauthors=Drozdz DR, Costa CC, Jesus PR, Trindade MS, Weiss G, Neto AB, da Silva AM, Mancopes R |title=Pharyngeal swallowing phase and chronic cough |journal=Int Arch Otorhinolaryngol |volume=16 |issue=4 |pages=502–8 |date=October 2012 |pmid=25991980 |pmc=4399588 |doi=10.7162/S1809-97772012000400012 |url=}}</ref> | |||
*[[Congestive heart failure]]<ref name="FerasinLinney2019">{{cite journal|last1=Ferasin|first1=L.|last2=Linney|first2=C.|title=Coughing in dogs: what is the evidence for and against a cardiac cough?|journal=Journal of Small Animal Practice|volume=60|issue=3|year=2019|pages=139–145|issn=00224510|doi=10.1111/jsap.12976}}</ref> | |||
* Habit [[cough]]<ref name="WeinbergerLockshin2017">{{cite journal|last1=Weinberger|first1=Miles|last2=Lockshin|first2=Boris|title=When is cough functional, and how should it be treated?|journal=Breathe|volume=13|issue=1|year=2017|pages=22–30|issn=1810-6838|doi=10.1183/20734735.015216}}</ref> | |||
==Diagnosis== | ==Diagnosis== | ||
Shown below is an algorithm summarizing the evaluation of acute [[cough]] | Shown below is an algorithm summarizing the evaluation of acute, subacute, chronic [[cough]].<ref name="pmid29080708">{{cite journal| author=Irwin RS, French CL, Chang AB, Altman KW, CHEST Expert Cough Panel*| title=Classification of Cough as a Symptom in Adults and Management Algorithms: CHEST Guideline and Expert Panel Report. | journal=Chest | year= 2018 | volume= 153 | issue= 1 | pages= 196-209 | pmid=29080708 | doi=10.1016/j.chest.2017.10.016 | pmc=6689094 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29080708 }} </ref><ref name="BoujaoudePratter2009">{{cite journal|last1=Boujaoude|first1=Ziad C.|last2=Pratter|first2=Melvin R.|title=Clinical Approach to Acute Cough|journal=Lung|volume=188|issue=S1|year=2009|pages=41–46|issn=0341-2040|doi=10.1007/s00408-009-9170-6}}</ref><ref name="pmid27029594">{{cite journal |vauthors=Kilgore PE, Salim AM, Zervos MJ, Schmitt HJ |title=Pertussis: Microbiology, Disease, Treatment, and Prevention |journal=Clin Microbiol Rev |volume=29 |issue=3 |pages=449–86 |date=July 2016 |pmid=27029594 |pmc=4861987 |doi=10.1128/CMR.00083-15 |url=}}</ref><ref name="pmid32026427">{{cite journal |vauthors=Kaplan AG |title=Chronic Cough in Adults: Make the Diagnosis and Make a Difference |journal=Pulm Ther |volume=5 |issue=1 |pages=11–21 |date=June 2019 |pmid=32026427 |pmc=6966942 |doi=10.1007/s41030-019-0089-7 |url=}}</ref> | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | '''Acute Cough''' | | | | | |'''Acute Cough'''='''Acute Cough'''}} | {{familytree | | | | | | | | | '''Acute Cough''' | | | | | |'''Acute Cough'''='''Acute [[Cough]]''' ≤ 3 [[weeks]] duration}} | ||
{{familytree | | | | | | | | | |!| | | | | | | | }} | {{familytree | | | | | | | | | |!| | | | | | | | }} | ||
{{familytree | | | | | | | | | History and physical | {{familytree | | | | | | | | | History and physical | ||
| Line 57: | Line 64: | ||
occupational factors | occupational factors | ||
and travel exposures | and travel exposures | ||
± investigations=History and physical | ± investigations=[[History]] and physical | ||
examination, ask about | examination, ask about | ||
environmental and | [[environmental]] and | ||
occupational factors | [[occupational]] factors | ||
and travel exposures | and [[travel]] exposures | ||
± investigations}} | ± investigations}} | ||
{{familytree | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} | {{familytree | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} | ||
| Line 67: | Line 74: | ||
diagnosis | | | | | | | | | | | |Non-life-threatening | diagnosis | | | | | | | | | | | |Non-life-threatening | ||
diagnosis|Life-threatening | diagnosis|Life-threatening | ||
diagnosis=Life-threatening | diagnosis=[[Life-threatening]] | ||
diagnosis|Non-life-threatening | diagnosis|Non-life-threatening | ||
diagnosis=Non-life-threatening | diagnosis=[[Non-life-threatening]] | ||
diagnosis}} | diagnosis}} | ||
{{familytree | | |!| | | | | | | |,|-|-|-|-|-|^|-|-|-|-|-|.| }} | {{familytree | | |!| | | | | | | |,|-|-|-|-|-|^|-|-|-|-|-|.| }} | ||
| Line 75: | Line 82: | ||
{{familytree | | Pneumonia, severe | {{familytree | | Pneumonia, severe | ||
exacerbation of asthma | exacerbation of asthma | ||
or COPD, | or COPD, pulmonary embolism, heart | ||
failure, other serious | failure, other serious | ||
disease | disease | ||
| | | | | |Infections| | | | | | | | | | Exacerbation of pre-existing condition |Pneumonia, severe | | | | | | |Infections| | | | | | | | | | Exacerbation of pre-existing condition |Pneumonia, severe | ||
exacerbation of asthma | exacerbation of asthma | ||
or COPD, | or COPD, pulmonary embolism, heart | ||
failure, other serious | failure, other serious | ||
disease | disease | ||
=Pneumonia, severe | =[[Pneumonia]], severe | ||
exacerbation of asthma | exacerbation of [[asthma]] | ||
or COPD, | or [[COPD]], [[pulmonary embolism]], [[heart failure]], other serious | ||
failure, other serious | disease|Exacerbation of pre-existing condition=Exacerbation of pre-existing [[condition]]|Infections=[[Infections]]}} | ||
disease|Exacerbation of pre-existing condition=Exacerbation of pre-existing condition|Infections=Infections}} | |||
{{familytree | | |!| | | | | |,|-|^|-|.| | | | | | |,|-|-|-|+|-|-|-|,|-|-|-|.|}} | {{familytree | | |!| | | | | |,|-|^|-|.| | | | | | |,|-|-|-|+|-|-|-|,|-|-|-|.|}} | ||
{{familytree | | |!| | | | LRTI | | | URTI | | | | Asthma | | Bronchiectasis | | UACS | | COPD |LRTI= | {{familytree | | |!| | | | LRTI | | | URTI | | | | Asthma | | Bronchiectasis | | UACS | | COPD |LRTI=[[Lower respiratory tract infection]]|URTI=[[Upper respiratory tract infection]]|Asthma=[[Asthma]]|Bronchiectasis=[[Bronchiectasis]]|UACS=[[Upper airway]] [[cough]] syndrome|COPD=[[COPD]]}} | ||
{{familytree | | Evaluate | {{familytree | | Evaluate | ||
and treat first | |,|-|+|-|-|.| | | | | | | | | | | | | |Evaluate | and treat first | |,|-|+|-|-|.| | | | | | | | | | | | | |Evaluate | ||
| Line 95: | Line 101: | ||
and treat first}} | and treat first}} | ||
{{familytree | | | | | |!| |!| | |!| | | | | | | | | | | }} | {{familytree | | | | | |!| |!| | |!| | | | | | | | | | | }} | ||
{{familytree | | | | | Acute Bronchitis |!| | Pertussis | | | | | | | | | | | | |Acute Bronchitis=Acute Bronchitis|Pertussis=Pertussis}} | {{familytree | | | | | Acute Bronchitis |!| | [[Pertussis]] | | | | | | | | | | | | |Acute Bronchitis=Acute [[Bronchitis]]|[[Pertussis]]=[[Pertussis]]}} | ||
{{familytree | | | | | | | |!| | | | | | | | | | | | | | }} | {{familytree | | | | | | | |!| | | | | | | | | | | | | | }} | ||
{{familytree | | | | | | | Consider TB in | {{familytree | | | | | | | Consider [[tuberculosis]] ([[TB]]) in | ||
endemic areas | endemic areas | ||
or high risk | or high risk | ||
| | | | | | | | | | | | |Consider TB in | | | | | | | | | | | | | |Consider [[tuberculosis]] ([[TB]]) in | ||
endemic areas | endemic areas | ||
or high risk | or high risk | ||
=Consider TB in | =Consider [[tuberculosis]] ([[TB]]) in | ||
endemic areas | endemic areas | ||
or high risk | or high risk | ||
| Line 109: | Line 115: | ||
{{familytree/end}} | {{familytree/end}} | ||
. | |||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | '''Subacute Cough''' | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |'''Subacute Cough'''='''Subacute Cough'''}} | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | '''Subacute Cough''' | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |'''Subacute Cough'''='''Subacute [[Cough]]''' ,(3-8 weeks duration)}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |!| | | | | | | }} | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |!| | | | | | | }} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | History and Physical Exam Ask about red flags, | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | History and Physical Exam Ask about red flags, | ||
| Line 120: | Line 126: | ||
environmental and | environmental and | ||
occupational factors, | occupational factors, | ||
travel exposures=History and Physical Exam Ask about red flags, | travel exposures=[[History]] and [[Physical Exam]], Ask about red flags ''( [[hemoptysis]], [[smoking ]], [[dyspnea]], [[hoarseness]], abnormal [[CXR]] findings)'' | ||
environmental and | [[environmental]] and | ||
occupational factors, | [[occupational]] factors, | ||
travel exposures }} | [[travel]] exposures }} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | | | |,|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|+|-|-|-|-|-|-|.| | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | {{familytree | | | | | | | |,|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|-|+|-|-|-|-|-|-|.| | | | | | | | | | | | | | | | | | | | | | | | | | | | | }} | ||
{{familytree | | | | | | |Postinfectious or life-threatening diagnosis | {{familytree | | | | | | |Postinfectious or life-threatening diagnosis | ||
| | | | | | | | | | | | | | | | | | | | | New onset or exacerbation of pre-existing condition| | | | | Not postinfectious | | | | | | | | | | | | | | | | | | | | | | New onset or exacerbation of pre-existing condition| | | | | Not postinfectious |Postinfectious or life-threatening diagnosis | ||
=Postinfectious or life-threatening diagnosis | =Postinfectious or [[life-threatening]] diagnosis | ||
|New onset or exacerbation of pre-existing condition=New onset or exacerbation of pre-existing condition|Not postinfectious | |New onset or exacerbation of pre-existing condition=New onset or exacerbation of pre-existing [[condition]]|Not postinfectious=Not [[postinfectious]]}} | ||
{{familytree | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | |!| | }} | {{familytree | | | | | | | |!| | | | | | | | | | | | | | | | | | | | | | |!| | }} | ||
{{familytree | | | |,|-|-|-|^|-|-|-|.| | | | | | | | | | | | | | | | | | |!| | | | | | | | }} | {{familytree | | | |,|-|-|-|^|-|-|-|.| | | | | | | | | | | | | | | | | | |!| | | | | | | | }} | ||
{{familytree | | |Pneumonia, severe exacerbation of asthma or COPD, | {{familytree | | |Pneumonia, severe exacerbation of asthma or COPD, pulmonary embolism, heart failure, other serious disease | ||
| | | | | | |!| | | | | | | | | | | | | | | | | | |!| | | | | | |Pneumonia, severe exacerbation of asthma or COPD, | | | | | | | |!| | | | | | | | | | | | | | | | | | |!| | | | | | |Pneumonia, severe exacerbation of asthma or COPD, pulmonary embolism, heart failure, other serious disease=[[Pneumonia]], severe exacerbation of [[asthma]] or [[COPD]],[[ pulmonary embolism]], [[heart failure]], other serious [[disease]] | ||
=Pneumonia, severe exacerbation of asthma or COPD, | |||
|}} | |}} | ||
{{familytree | | | | | | | | | | | |!| | |,|-| | {{familytree | | | | | | | | | | | |!| | |,|-| Pertussis | | | | | | | | | | | |!| | | | | | | |Pertussis=[[Pertussis]]}} | ||
{{familytree | | | | | | | | | | | |!| | |!| | | | | | | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.}} | {{familytree | | | | | | | | | | | |!| | |!| | | | | | | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.}} | ||
{{familytree | | | | | | | | | | | |!| | |)|-| COPD | | | |!| | | |!| | | |!| | | |!| | | |!| |COPD=COPD}} | {{familytree | | | | | | | | | | | |!| | |)|-| COPD | | | |!| | | |!| | | |!| | | |!| | | |!| |COPD=[[COPD]]}} | ||
{{familytree | | | | | | | | | | | |!| | |!| | | | | | | UACS | | Asthma | | Bronchitis | | GERD | | Bronchiectasis|UACS= | {{familytree | | | | | | | | | | | |!| | |!| | | | | | | UACS | | Asthma | | Bronchitis | | GERD | | Bronchiectasis|UACS=[[Upper airway]] [[cough]] syndrome|Asthma=[[Asthma]]|Bronchitis=[[Bronchitis]]|GERD=[[Gastroesophageal reflux disease]]|Bronchiectasis=[[Bronchiectasis]]}} | ||
{{familytree | | | | | | | | | | | | {{familytree | | | | | | | | | | | k |-|+|-| Postinfectious | | | | | | | | | | | |!| | | |Postinfectious=[[Postinfectious]]|k=[[ Condition]]}} | ||
{{familytree | | | | | | | | | | | | | | |!| | | | | | | | | | | | |,|-|-|^|-|-|.| | | |}} | {{familytree | | | | | | | | | | | | | | |!| | | | | | | | | | | | |,|-|-|^|-|-|.| | | |}} | ||
{{familytree | | | | | | | | | | | | | | | | {{familytree | | | | | | | | | | | | | | |`|-| TB| | | | | | | | NAEB | | | | AECB | ||
| | | |TB= | | | | |TB=[[Tuberculosis]] |NAEB=Non-[[asthmatic]] [[eosinophilic]] [[bronchitis]]|AECB= Acute exacerbation of chronic [[bronchitis]]/[[COPD]] | ||
= | |||
}} | }} | ||
{{familytree/end}} | {{familytree/end}} | ||
<span style="font-size:85%">'''Abbreviations:''' | |||
'''[[TB]]:''' [[Tuberculosis]]; | |||
'''[[COPD]]:''' [[Chronic obstructive pulmonary disease]]; | |||
'''[[GERD]]:'''[[Gastroesophageal reflux disease]] | |||
</span> | |||
<br> | |||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | |'''Chronic Cough'''| | | | | | | | | |'''Chronic Cough'''='''Chronic Cough'''}} | {{familytree | | | | | | | | |'''Chronic Cough'''| | | | | | | | | |'''Chronic Cough'''='''Chronic Cough'''> 8 weeks duration }} | ||
{{familytree | | | | | | | | | |!| | | | | | | | | | | | | | | |}} | {{familytree | | | | | | | | | |!| | | | | | | | | | | | | | | |}} | ||
{{familytree | | | | | | | | | History, Physical exam and CXR | | | | | |History, Physical exam and CXR=History, Physical exam and CXR}} | {{familytree | | | | | | | | | History, Physical exam and CXR | | | | | |History, Physical exam and CXR=[[History]], [[Physical exam]] and [[CXR]]}} | ||
{{familytree | | |,|-|-|-|-|-|-|+|-|-|-|-|-|-|.| }} | {{familytree | | |,|-|-|-|-|-|-|+|-|-|-|-|-|-|.| }} | ||
{{familytree | | Life-threatening condition | | | | | Consider | {{familytree | | Life-threatening condition | | | | | Consider four most common causes | | | | | [[Smoking]], [[ACEI]]|Life-threatening condition=Life-threatening [[condition]]|Consider four most common causes =Consider four most common causes: 1) [[Upper Airway]] [[Cough]] Syndrome secondary to [[rhinosinus]] diseases, 2) [[Asthma]], 3) Non-[[asthmatic]] [[Eosinophilic]] [[Bronchitis]],4) [[Gastroesophageal Reflux Disease]] ([[GERD]])|[[Smoking]], [[ACEI]]=[[Smoking]], [[ACEI]]}} | ||
{{familytree | | |!| | | | | | |!| | | | | | |!| }} | {{familytree | | |!| | | | | | |!| | | | | | |!| }} | ||
{{familytree | | Treat based on the cause | | |,|-|-|^|-|-|-|.| | Discontinue for at least | {{familytree | | Treat based on the cause | | |,|-|-|^|-|-|-|.| | Discontinue for at least four weeks | | | ||Treat based on the cause=[[Treat]] based on the cause|Discontinue for at least four weeks=Discontinue for at least four [[weeks]]}} | ||
{{familytree | | |!| | | |!| | | | | | |!| | |!| | | | | }} | {{familytree | | |!| | | |!| | | | | | |!| | |!| | | | | }} | ||
{{familytree | | Follow up 4-6 weeks if inadequate response| | Initial treatments for each condition| | | | | Further investigation if No response to treatment | {{familytree | | Follow up 4-6 weeks if inadequate response| | Initial treatments for each condition| | | | | Further investigation if No response to treatment | |Consider four most common causes of cough if No response at 4-6 weeks follow up |Follow up 4-6 weeks if inadequate response=[[Follow up]] 4-6 weeks if inadequate response|Further investigation if No response to treatment=Further investigation if No response to [[treatment]]|Initial treatments for each condition=Initial [[treatments]] for each [[condition]]|Follow up 4-6 weeks if inadequate response to optimal treatment=Follow up 4-6 weeks if inadequate response to optimal [[treatment]]|Consider four most common causes of cough if No response at 4-6 weeks follow up=Consider four most common causes of [[cough]] if No response at 4-6 weeks [[follow up]]}} | ||
{{familytree | | | | | | |!| | | | | | | | {{familytree | | | | | | |!| | | | | | |!| | | | | }} | ||
{{familytree | | | | | | Follow up 4-6 weeks if inadequate response to optimal treatment | | | | | {{familytree | | | | | | Follow up 4-6 weeks if inadequate response to optimal treatment | | | | C1 | | | |Follow up 4-6 weeks if inadequate response to optimal treatment=[[Follow up]] 4-6 weeks if inadequate response to optimal [[treatment]]| C1=<div style="float: left; text-align: left; height: 20em; width: 17em; padding:1em;"> '''The investigation:'''<br> | ||
{{familytree | | ---- | ||
❑ 24h [[esophageal]] [[pH]] monitoring<br> ❑ [[Endoscopic]], [[videofluoroscopic]] [[swallow]] evaluation <br> ❑ [[Barium esophagram]] <br> ❑ [[Sinus Imaging]] <br> ❑ [[HRCT]] <br>❑[[Bronchoscopy]]<br>❑ [[ECG]],[[ Holter]] Monitoring, [[Echocardiography]] <br>❑[[Environmental]] / [[Occupational]] Assessment<br></div>}} | |||
{{familytree | | | | | | | | | | | | | | | | | | | }} | |||
{{familytree/end}} | {{familytree/end}} | ||
{{familytree/end}} | |||
<span style="font-size:85%">'''Abbreviations:''' | |||
'''[[CXR]]:''' [[Chest-X-ray]]; | |||
'''[[ACEI]]:''' [[Angiotensin converting enzyme inhibitor]]; | |||
'''[[GERD]]:''' [[Gastroesophageal reflux disease]]; | |||
'''[[HRCT]] scan:'''[[High-resolution computed tomography]]. | |||
</span> | |||
<br> | |||
==Treatment== | ==Treatment== | ||
Shown below is an algorithm summarizing the treatment of [[Cough]] | Shown below is an algorithm summarizing the treatment of [[Cough]].<ref name="BoujaoudePratter2009">{{cite journal|last1=Boujaoude|first1=Ziad C.|last2=Pratter|first2=Melvin R.|title=Clinical Approach to Acute Cough|journal=Lung|volume=188|issue=S1|year=2009|pages=41–46|issn=0341-2040|doi=10.1007/s00408-009-9170-6}}</ref><ref name="YildizDulger2018">{{cite journal|last1=Yildiz|first1=Tekin|last2=Dulger|first2=Seyhan|title=Non-astmatic Eosinophilic Bronchitis|journal=Turkish Thoracic Journal|volume=19|issue=1|year=2018|pages=41–45|issn=21492530|doi=10.5152/TurkThoracJ.2017.17017}}</ref><ref name="pmid31478634">{{cite journal |vauthors=DeGeorge KC, Ring DJ, Dalrymple SN |title=Treatment of the Common Cold |journal=Am Fam Physician |volume=100 |issue=5 |pages=281–289 |date=September 2019 |pmid=31478634 |doi= |url=}}</ref><ref name="pmid26394802">{{cite journal |vauthors=Scanlon KM, Skerry C, Carbonetti NH |title=Novel therapies for the treatment of pertussis disease |journal=Pathog Dis |volume=73 |issue=8 |pages=ftv074 |date=November 2015 |pmid=26394802 |pmc=4626598 |doi=10.1093/femspd/ftv074 |url=}}</ref><ref name="pmid30201828">{{cite journal |vauthors=Speich B, Thomer A, Aghlmandi S, Ewald H, Zeller A, Hemkens LG |title=Treatments for subacute cough in primary care: systematic review and meta-analyses of randomised clinical trials |journal=Br J Gen Pract |volume=68 |issue=675 |pages=e694–e702 |date=October 2018 |pmid=30201828 |pmc=6145999 |doi=10.3399/bjgp18X698885 |url=}}</ref><ref name="Morice2004">{{cite journal|last1=Morice|first1=A.H.|title=The diagnosis and management of chronic cough|journal=European Respiratory Journal|volume=24|issue=3|year=2004|pages=481–492|issn=0903-1936|doi=10.1183/09031936.04.00027804}}</ref> | ||
{{familytree/start |summary=Sample | |||
{{familytree/start |summary=Sample 12}}{{familytree/start |summary=PE diagnosis Algorithm.}} | |||
{{Family tree/start}} | |||
{{Family tree/start}} | |||
{{Family tree | | | | A01 | | | |A01= [[File:Cough image.jpg|300px]]}} | |||
{{Family tree | | | | |!| | | | | }} | |||
{{Family tree | | | | B01 | | | |B01= '''Acute [[Cough]]'''}} | |||
{{Family tree | |,|-|-|^|-|-|.| | }} | |||
{{Family tree | C01 | | | | C02 |C01= ❑''Determine if the cause of the [[cough]] is one of the [[life-threatening]] [[conditions]]'': <br> ❑[[Pneumonia]] <br> ❑Severe exacerbation of [[asthma]] or [[COPD]]<br> ❑ [[Pulmonary embolism]] <br> ❑[[Heart failure]]<br> ❑ Other serious condittons | |||
| C02= ❑''[[Cough]] due to the [[common cold]]'':<br>❑ First-generation [[antihistamine]] plus a [[decongestant]]<br> ❑[[Ipratropium]] <br> ❑ Newer-generation [[nonsedating]] [[antihistamines]] are not effective <br> </div>}} | |||
{{familytree/end}} | |||
<br> | |||
<br> | |||
<br> | |||
<br> | |||
{{familytree/start |summary=Sample 12}}{{familytree/start |summary=PE diagnosis Algorithm.}} | |||
{{Family tree/start}} | {{Family tree/start}} | ||
{{ | {{Family tree/start}} | ||
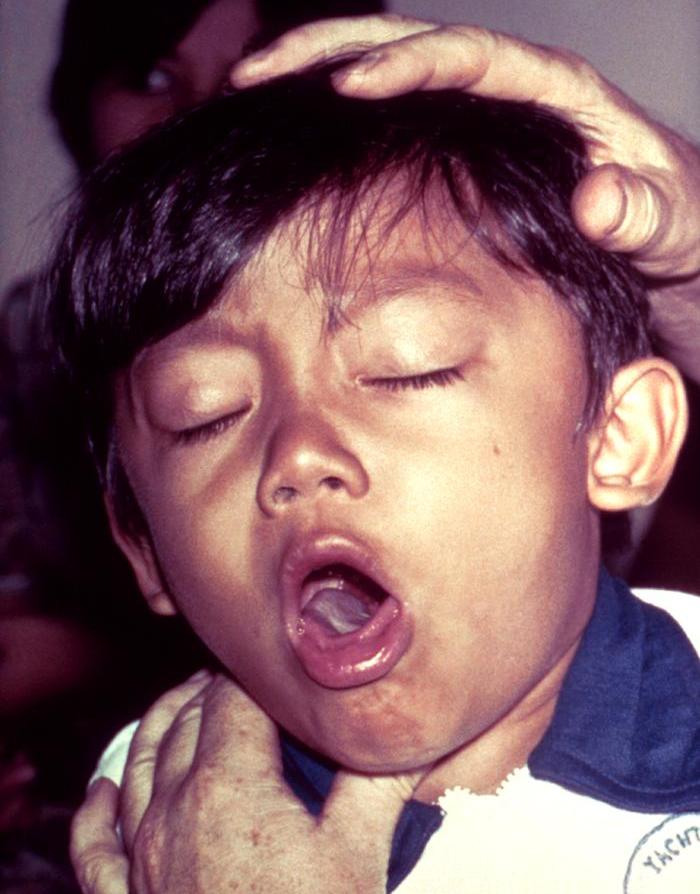
---- | {{Family tree | | | | A01 | | | |A01= [[File:Pertussis.jpg|300px]]}} | ||
{{Family tree | | | | |!| | | | | }} | |||
{{Family tree | | | | B01 | | | |B01= '''Subacute [[Cough]]'''}} | |||
{{Family tree | |,|-|-|^|-|-|.| | }} | |||
{{Family tree | C01 | | | | C02 |C01= confirmed [[whooping]] [[cough]] by [[culture]] positive [[nasopharyngeal]] swab:<br>[[macrolide]] [[antibiotics]] plus [[isolation]] for 5 days| C02= [[Cough]] not caused by [[bordetella pertussis]]:<br>❑ [[Inhaled]] [[ipratropium]] ([[Atrovent]])<br> ❑ If [[cough]] persists: inhaled [[corticosteroids]]<br> ❑ Severe [[cough]]:30 to 40 mg of [[prednisone]] per day for a brief period)<br> ❑ When other [[treatments]] fail: [[codeine]] or [[dextromethorphan]] ([[Delsym]])<br> }} | |||
{{familytree/end}} | {{familytree/end}} | ||
<br> | <br> | ||
{{familytree/start |summary=Sample | <br> | ||
<br> | |||
{{familytree/start |summary=Sample 12}}{{familytree/start |summary=PE diagnosis Algorithm.}} | |||
{{Family tree/start}} | {{Family tree/start}} | ||
{{ | {{Family tree/start}} | ||
---- | {{Family tree | | | | | | | | | | | | | | | A01 | | | |A01= [[File:COPD.jpg|300px]]}} | ||
< | {{Family tree | | | | | | | | | | | | | | | |!| | | | | }} | ||
{{Family tree | | | | | | | | | | | | | | | B01 | | | | | | | | | | | | | | | | | | | | | | | | |B01= '''Chronic [[Cough]]'''}} | |||
{{Family tree | | | | | | |,|-|-|-|-|-|v|-|-|^|-|-|-|v|-|-|-|-|.| | | | | | | | | | | | | | | | | | | | }} | |||
{{Family tree | | | | | | C01 | | | | C02 | | | | | C03 | | | C04 | | | | | |C01='''[[UPPER AIRWAY]] [[COUGH]] SYNDROME–INDUCED CHRONIC [[ COUGH]]'''<br>❑[[First-generation]] [[antihistamine]]/[[decongestant]]<br> ❑Partial or complete resolution of [[cough]] after one to two weeks shows '''[[upper airway]] [[cough]] syndrome''' as the cause<br> ❑ Persistent symptoms: begin a topical [[nasal steroid]]<br> ❑ [[Symptoms]] still persist: [[sinus]] imaging for [[sinusitis]]| C02= '''[[ASTHMA]]-INDUCED CHRONIC [[COUGH]]'''<br>❑ Inhaled [[corticosteroids]] and [[beta agonists]]<br> ❑ No response or cannot take [[inhaled]] [[ medication]]:consider oral [[corticosteroids]] for 5-10 days<br> ❑ Consider adding a [[leukotriene inhibitor]] before an oral [[corticosteroid]]|C03= '''NON-[[ASTHMATIC]] [[EOSINOPHILIC]] [[BRONCHITIS]]-INDUCED CHRONIC [[COUGH]]'''<br>❑ Inhaled [[corticosteroids]] for 4 weeks|C04= '''[[GERD]]-INDUCED CHRONIC [[COUGH]]'''<br>❑ Empirically treated for [[GERD]] if there is not response to [[therapy]]<br> ❑ Anti-[[reflux]] [[diet]], [[lifestyle modification]], [[proton pump inhibitor]]<br> ❑ Adding [[prokinetic]] [[therapy]] if there is NO response to [[treatment]]}} | |||
{{familytree/end}} | {{familytree/end}} | ||
<br> | |||
<br> | |||
==Do's== | |||
* Always first determine if the cause of the [[cough]] is one of the life-threatening [[conditions]] especially during management of acute [[cough ]] such as [[pulmonary embolism]] or [[obstructive airway disease]]. | |||
* Always evaluate [[environmental]] factors such as [[air pollution]] and occupational exposure for management of chronic [[cough]].<ref name="JoSong2019">{{cite journal|last1=Jo|first1=Eun-Jung|last2=Song|first2=Woo-Jung|title=Environmental triggers for chronic cough|journal=Asia Pacific Allergy|volume=9|issue=2|year=2019|issn=2233-8276|doi=10.5415/apallergy.2019.9.e16}}</ref> | |||
*[[Leukotriene inhibitor]] is prefered to treat [[asthma]] induced chronic [[cough]] before begining of oral [[corticosteroid]] agents for prevention of the side effects of [[cotricosteroid]]. | |||
* Three common causes of chronic [[cough]] include [[upper aiway]] [[cough]] syndrome, [[asthma]], and [[gastroesophageal reflux disease]].<ref name="pmid22010767">{{cite journal |vauthors=Benich JJ, Carek PJ |title=Evaluation of the patient with chronic cough |journal=Am Fam Physician |volume=84 |issue=8 |pages=887–92 |date=October 2011 |pmid=22010767 |doi= |url=}}</ref><ref name="pmid8624180">{{cite journal |vauthors=Mello CJ, Irwin RS, Curley FJ |title=Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause |journal=Arch Intern Med |volume=156 |issue=9 |pages=997–1003 |date=May 1996 |pmid=8624180 |doi= |url=}}</ref> | |||
*Notify [[GERD]] in [[pediatric]] presented with [[cough]], [[vomiting]], poor [[weight gain]], [[dysphagia]], [[abdominal]] or [[substernal]] [[pain]].<ref name="RudolphMazur2001">{{cite journal|last1=Rudolph|first1=Colin D.|last2=Mazur|first2=Lynnette J.|last3=Liptak|first3=Gregory S.|last4=Baker|first4=Robert D.|last5=Boyle|first5=John T.|last6=Colletti|first6=Richard B.|last7=Gerson|first7=William T.|last8=Werlin|first8=Steven L.|title=Guidelines for Evaluation and Treatment of Gastroesophageal Reflux in Infants and Children|journal=Journal of Pediatric Gastroenterology and Nutrition|volume=32|year=2001|pages=S1–S31|issn=0277-2116|doi=10.1097/00005176-200100002-00001}}</ref> | |||
*The mechanism of [[cough]] in [[upper airway]] [[cough]] syndrome may include [[postnatal drip]], [[ direct irritation]], or [[inflammation]] of the [[cough]] receptors in the [[upper airway]].<ref name="Pratter2006">{{cite journal|last1=Pratter|first1=Melvin R.|title=Chronic Upper Airway Cough Syndrome Secondary to Rhinosinus Diseases (Previously Referred to as Postnasal Drip Syndrome )|journal=Chest|volume=129|issue=1|year=2006|pages=63S–71S|issn=00123692|doi=10.1378/chest.129.1_suppl.63S}}</ref> | |||
* In [[patients]] with [[tuberclusis]] or [[covid-19]], [[cough]] can promote the [[aerosolization]] of [[infectious]] [[particle]].<ref name="TurnerBothamley2015">{{cite journal|last1=Turner|first1=Richard D.|last2=Bothamley|first2=Graham H.|title=Cough and the Transmission of Tuberculosis|journal=The Journal of Infectious Diseases|volume=211|issue=9|year=2015|pages=1367–1372|issn=0022-1899|doi=10.1093/infdis/jiu625}}</ref><ref name="MacIntyreBourouiba2020">{{cite journal|last1=MacIntyre|first1=C Raina|last2=Bourouiba|first2=Lydia|last3=Chughtai|first3=Abrar Ahmad|last4=de Silva|first4=Charitha|last5=Doolan|first5=Con|last6=Bahl|first6=Prateek|title=Airborne or Droplet Precautions for Health Workers Treating Coronavirus Disease 2019?|journal=The Journal of Infectious Diseases|year=2020|issn=0022-1899|doi=10.1093/infdis/jiaa189}}</ref> | |||
==Don'ts== | |||
{{ | * Do not continue [[ACE inhibitors]] if [[cough]] is associated with the begining of [[ACEI]].<ref name="McEwanChoudry1989">{{cite journal|last1=McEwan|first1=J. R.|last2=Choudry|first2=N.|last3=Street|first3=R.|last4=Fuller|first4=R. W.|title=Change in cough reflex after treatment with enalapril and ramipril.|journal=BMJ|volume=299|issue=6690|year=1989|pages=13–16|issn=0959-8138|doi=10.1136/bmj.299.6690.13}}</ref> | ||
== | * Do not miss the following red flags during an assessment of [[cough]]:<ref name="pmid32026427">{{cite journal |vauthors=Kaplan AG |title=Chronic Cough in Adults: Make the Diagnosis and Make a Difference |journal=Pulm Ther |volume=5 |issue=1 |pages=11–21 |date=June 2019 |pmid=32026427 |pmc=6966942 |doi=10.1007/s41030-019-0089-7 |url=}}</ref> | ||
* | **[[Hemoptysis]] | ||
** Changing in [[ cough]] or initiating [[caugh]] in smoker > 45 years old | |||
** Coexisting [[voice]] disturbance | |||
** [[Hoarseness]] | |||
** [[Systemic]] [[symptoms]] including [[fever]], [[weight loss]], [[Peripheral edema]] with [[weight gain]] | |||
** [[Vomiting]] | |||
** Recurrent [[pneumonia]] | |||
** Abnormal [[ chest]] [[radiographic]] findings | |||
** Adults aged 55-80 years with a history of a 30 [[pack-year]] [[smoking]], currently [[smoking]] or history of quitting within the past 15 years | |||
** [[Dyspnea]] at rest, [[orthopnea]] | |||
** [[swallowing]] difficulty during [[eating]] or [[drinking]] | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 09:20, 19 March 2021
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sara Haddadi, M.D.[2] Sara Zand, M.D.[3]
| Cough Resident Survival Guide |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Cough is a defense mechanism for preventation of airway irritation or aspiration by cleaning excessive secretion or foreign body from the airway and also it may spread infection. Cough is the symptom of involving organs such as upper airway tract, lung, heart, or gastrointestinal tract. Dependent on the duration of cough, it can be categorized to three groups including acute, subacute, chronic. Acute cough is the most common causes of seeking medical attention every year. Chronic cough may affect the quality of life and also may increase mortality based on the underlying disorder. Assessment of the life threatening causes of cough such as obstructive airway disease or pulmonary embolism is of important.
Causes
Common Causes
- Allergic Rhinitis
- Asthma[1]
- Bronchitis[2]
- Gastroesophageal Reflux Disease (GERD)
- Post-nasal drip[3]
- Foreign body aspiration[4]
- ACE inhibitors[5]
- Bronchiectasis[6]
- Laryngopharyngeal reflux[7]
- Respiratory tract infection[8]
- Lung cancer[9]
- Non-asthmatic eosinophilic bronchitis[10]
- Non-acid reflux disease[11]
- Swallowing disorder[12]
- Congestive heart failure[13]
- Habit cough[14]
Diagnosis
Shown below is an algorithm summarizing the evaluation of acute, subacute, chronic cough.[15][16][17][18]
| Acute Cough ≤ 3 weeks duration | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| History and physical
examination, ask about environmental and occupational factors and travel exposures ± investigations | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Life-threatening diagnosis | Non-life-threatening diagnosis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Pneumonia, severe
exacerbation of asthma or COPD, pulmonary embolism, heart failure, other serious disease | Infections | Exacerbation of pre-existing condition | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Lower respiratory tract infection | Upper respiratory tract infection | Asthma | Bronchiectasis | Upper airway cough syndrome | COPD | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Evaluate and treat first | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Acute Bronchitis | Pertussis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Consider tuberculosis (TB) in
endemic areas or high risk | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
.
| Subacute Cough ,(3-8 weeks duration) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| History and Physical Exam, Ask about red flags ( hemoptysis, smoking , dyspnea, hoarseness, abnormal CXR findings)
environmental and occupational factors, travel exposures | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Postinfectious or life-threatening diagnosis | New onset or exacerbation of pre-existing condition | Not postinfectious | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Pneumonia, severe exacerbation of asthma or COPD,pulmonary embolism, heart failure, other serious disease | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Pertussis | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| COPD | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Upper airway cough syndrome | Asthma | Bronchitis | Gastroesophageal reflux disease | Bronchiectasis | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Condition | Postinfectious | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Tuberculosis | Non-asthmatic eosinophilic bronchitis | Acute exacerbation of chronic bronchitis/COPD | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Abbreviations: TB: Tuberculosis; COPD: Chronic obstructive pulmonary disease; GERD:Gastroesophageal reflux disease
| Chronic Cough> 8 weeks duration | |||||||||||||||||||||||||||||||||||||||||||||||||||
| History, Physical exam and CXR | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Life-threatening condition | Consider four most common causes: 1) Upper Airway Cough Syndrome secondary to rhinosinus diseases, 2) Asthma, 3) Non-asthmatic Eosinophilic Bronchitis,4) Gastroesophageal Reflux Disease (GERD) | Smoking, ACEI | |||||||||||||||||||||||||||||||||||||||||||||||||
| Treat based on the cause | Discontinue for at least four weeks | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Follow up 4-6 weeks if inadequate response | Initial treatments for each condition | Further investigation if No response to treatment | Consider four most common causes of cough if No response at 4-6 weeks follow up | ||||||||||||||||||||||||||||||||||||||||||||||||
| Follow up 4-6 weeks if inadequate response to optimal treatment | The investigation: ❑ 24h esophageal pH monitoring ❑ Endoscopic, videofluoroscopic swallow evaluation ❑ Barium esophagram ❑ Sinus Imaging ❑ HRCT ❑Bronchoscopy ❑ ECG,Holter Monitoring, Echocardiography ❑Environmental / Occupational Assessment | ||||||||||||||||||||||||||||||||||||||||||||||||||
Abbreviations: CXR: Chest-X-ray; ACEI: Angiotensin converting enzyme inhibitor; GERD: Gastroesophageal reflux disease; HRCT scan:High-resolution computed tomography.
Treatment
Shown below is an algorithm summarizing the treatment of Cough.[16][19][20][21][22][23]
 | |||||||||||||||||||
| Acute Cough | |||||||||||||||||||
| ❑Determine if the cause of the cough is one of the life-threatening conditions: ❑Pneumonia ❑Severe exacerbation of asthma or COPD ❑ Pulmonary embolism ❑Heart failure ❑ Other serious condittons | ❑Cough due to the common cold: ❑ First-generation antihistamine plus a decongestant ❑Ipratropium ❑ Newer-generation nonsedating antihistamines are not effective | ||||||||||||||||||
 | |||||||||||||||||||
| Subacute Cough | |||||||||||||||||||
| confirmed whooping cough by culture positive nasopharyngeal swab: macrolide antibiotics plus isolation for 5 days | Cough not caused by bordetella pertussis: ❑ Inhaled ipratropium (Atrovent) ❑ If cough persists: inhaled corticosteroids ❑ Severe cough:30 to 40 mg of prednisone per day for a brief period) ❑ When other treatments fail: codeine or dextromethorphan (Delsym) | ||||||||||||||||||
 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Chronic Cough | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| UPPER AIRWAY COUGH SYNDROME–INDUCED CHRONIC COUGH ❑First-generation antihistamine/decongestant ❑Partial or complete resolution of cough after one to two weeks shows upper airway cough syndrome as the cause ❑ Persistent symptoms: begin a topical nasal steroid ❑ Symptoms still persist: sinus imaging for sinusitis | ASTHMA-INDUCED CHRONIC COUGH ❑ Inhaled corticosteroids and beta agonists ❑ No response or cannot take inhaled medication:consider oral corticosteroids for 5-10 days ❑ Consider adding a leukotriene inhibitor before an oral corticosteroid | NON-ASTHMATIC EOSINOPHILIC BRONCHITIS-INDUCED CHRONIC COUGH ❑ Inhaled corticosteroids for 4 weeks | GERD-INDUCED CHRONIC COUGH ❑ Empirically treated for GERD if there is not response to therapy ❑ Anti-reflux diet, lifestyle modification, proton pump inhibitor ❑ Adding prokinetic therapy if there is NO response to treatment | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Do's
- Always first determine if the cause of the cough is one of the life-threatening conditions especially during management of acute cough such as pulmonary embolism or obstructive airway disease.
- Always evaluate environmental factors such as air pollution and occupational exposure for management of chronic cough.[24]
- Leukotriene inhibitor is prefered to treat asthma induced chronic cough before begining of oral corticosteroid agents for prevention of the side effects of cotricosteroid.
- Three common causes of chronic cough include upper aiway cough syndrome, asthma, and gastroesophageal reflux disease.[25][26]
- Notify GERD in pediatric presented with cough, vomiting, poor weight gain, dysphagia, abdominal or substernal pain.[27]
- The mechanism of cough in upper airway cough syndrome may include postnatal drip, direct irritation, or inflammation of the cough receptors in the upper airway.[28]
- In patients with tuberclusis or covid-19, cough can promote the aerosolization of infectious particle.[29][30]
Don'ts
- Do not continue ACE inhibitors if cough is associated with the begining of ACEI.[31]
- Do not miss the following red flags during an assessment of cough:[18]
- Hemoptysis
- Changing in cough or initiating caugh in smoker > 45 years old
- Coexisting voice disturbance
- Hoarseness
- Systemic symptoms including fever, weight loss, Peripheral edema with weight gain
- Vomiting
- Recurrent pneumonia
- Abnormal chest radiographic findings
- Adults aged 55-80 years with a history of a 30 pack-year smoking, currently smoking or history of quitting within the past 15 years
- Dyspnea at rest, orthopnea
- swallowing difficulty during eating or drinking
References
- ↑ Janson C, Chinn S, Jarvis D, Burney P (October 2001). "Determinants of cough in young adults participating in the European Community Respiratory Health Survey". Eur Respir J. 18 (4): 647–54. doi:10.1183/09031936.01.00098701. PMID 11716169.
- ↑ Kim V, Criner GJ (February 2013). "Chronic bronchitis and chronic obstructive pulmonary disease". Am J Respir Crit Care Med. 187 (3): 228–37. doi:10.1164/rccm.201210-1843CI. PMC 4951627. PMID 23204254.
- ↑ Sylvester DC, Karkos PD, Vaughan C, Johnston J, Dwivedi RC, Atkinson H, Kortequee S (2012). "Chronic cough, reflux, postnasal drip syndrome, and the otolaryngologist". Int J Otolaryngol. 2012: 564852. doi:10.1155/2012/564852. PMC 3332192. PMID 22577385.
- ↑ Akelma, Ahmet Zulfikar; Cizmeci, Mehmet Nevzat; Kanburoglu, Mehmet Kenan; Mete, Emin (2013). "An Overlooked Cause of Cough in Children: Foreign Body Aspiration". The Journal of Pediatrics. 163 (1): 292–293. doi:10.1016/j.jpeds.2012.12.089. ISSN 0022-3476.
- ↑ Yılmaz İ (January 2019). "Angiotensin-Converting Enzyme Inhibitors Induce Cough". Turk Thorac J. 20 (1): 36–42. doi:10.5152/TurkThoracJ.2018.18014. PMC 6340691. PMID 30664425.
- ↑ Mac Aogáin M, Chotirmall SH (August 2019). "Bronchiectasis and cough: An old relationship in need of renewed attention". Pulm Pharmacol Ther. 57: 101812. doi:10.1016/j.pupt.2019.101812. PMC 7110869 Check
|pmc=value (help). PMID 31176801. - ↑ Patel DA, Blanco M, Vaezi MF (September 2018). "Laryngopharyngeal Reflux and Functional Laryngeal Disorder: Perspective and Common Practice of the General Gastroenterologist". Gastroenterol Hepatol (N Y). 14 (9): 512–520. PMC 6194652. PMID 30364386.
- ↑ Dicpinigaitis PV (October 2014). "Effect of viral upper respiratory tract infection on cough reflex sensitivity". J Thorac Dis. 6 (Suppl 7): S708–11. doi:10.3978/j.issn.2072-1439.2013.12.02. PMC 4222932. PMID 25383204.
- ↑ Harle, Amélie; Molassiotis, Alex; Buffin, Oliver; Burnham, Jack; Smith, Jaclyn; Yorke, Janelle; Blackhall, Fiona H. (2020). "A cross sectional study to determine the prevalence of cough and its impact in patients with lung cancer: a patient unmet need". BMC Cancer. 20 (1). doi:10.1186/s12885-019-6451-1. ISSN 1471-2407.
- ↑ Yıldız T, Dülger S (January 2018). "Non-astmatic Eosinophilic Bronchitis". Turk Thorac J. 19 (1): 41–45. doi:10.5152/TurkThoracJ.2017.17017. PMC 5783052. PMID 29404185.
- ↑ Qiu, Zhongmin; Xu, Xianghuai; Yu, Li; Chen, Qiang; Lv, Hanjing (2015). "Diagnosis and treatment of patients with nonacid gastroesophageal reflux-induced chronic cough". Journal of Research in Medical Sciences. 20 (9): 885. doi:10.4103/1735-1995.170625. ISSN 1735-1995.
- ↑ Drozdz DR, Costa CC, Jesus PR, Trindade MS, Weiss G, Neto AB, da Silva AM, Mancopes R (October 2012). "Pharyngeal swallowing phase and chronic cough". Int Arch Otorhinolaryngol. 16 (4): 502–8. doi:10.7162/S1809-97772012000400012. PMC 4399588. PMID 25991980.
- ↑ Ferasin, L.; Linney, C. (2019). "Coughing in dogs: what is the evidence for and against a cardiac cough?". Journal of Small Animal Practice. 60 (3): 139–145. doi:10.1111/jsap.12976. ISSN 0022-4510.
- ↑ Weinberger, Miles; Lockshin, Boris (2017). "When is cough functional, and how should it be treated?". Breathe. 13 (1): 22–30. doi:10.1183/20734735.015216. ISSN 1810-6838.
- ↑ Irwin RS, French CL, Chang AB, Altman KW, CHEST Expert Cough Panel* (2018). "Classification of Cough as a Symptom in Adults and Management Algorithms: CHEST Guideline and Expert Panel Report". Chest. 153 (1): 196–209. doi:10.1016/j.chest.2017.10.016. PMC 6689094 Check
|pmc=value (help). PMID 29080708. - ↑ 16.0 16.1 Boujaoude, Ziad C.; Pratter, Melvin R. (2009). "Clinical Approach to Acute Cough". Lung. 188 (S1): 41–46. doi:10.1007/s00408-009-9170-6. ISSN 0341-2040.
- ↑ Kilgore PE, Salim AM, Zervos MJ, Schmitt HJ (July 2016). "Pertussis: Microbiology, Disease, Treatment, and Prevention". Clin Microbiol Rev. 29 (3): 449–86. doi:10.1128/CMR.00083-15. PMC 4861987. PMID 27029594.
- ↑ 18.0 18.1 Kaplan AG (June 2019). "Chronic Cough in Adults: Make the Diagnosis and Make a Difference". Pulm Ther. 5 (1): 11–21. doi:10.1007/s41030-019-0089-7. PMC 6966942 Check
|pmc=value (help). PMID 32026427 Check|pmid=value (help). - ↑ Yildiz, Tekin; Dulger, Seyhan (2018). "Non-astmatic Eosinophilic Bronchitis". Turkish Thoracic Journal. 19 (1): 41–45. doi:10.5152/TurkThoracJ.2017.17017. ISSN 2149-2530.
- ↑ DeGeorge KC, Ring DJ, Dalrymple SN (September 2019). "Treatment of the Common Cold". Am Fam Physician. 100 (5): 281–289. PMID 31478634.
- ↑ Scanlon KM, Skerry C, Carbonetti NH (November 2015). "Novel therapies for the treatment of pertussis disease". Pathog Dis. 73 (8): ftv074. doi:10.1093/femspd/ftv074. PMC 4626598. PMID 26394802.
- ↑ Speich B, Thomer A, Aghlmandi S, Ewald H, Zeller A, Hemkens LG (October 2018). "Treatments for subacute cough in primary care: systematic review and meta-analyses of randomised clinical trials". Br J Gen Pract. 68 (675): e694–e702. doi:10.3399/bjgp18X698885. PMC 6145999. PMID 30201828.
- ↑ Morice, A.H. (2004). "The diagnosis and management of chronic cough". European Respiratory Journal. 24 (3): 481–492. doi:10.1183/09031936.04.00027804. ISSN 0903-1936.
- ↑ Jo, Eun-Jung; Song, Woo-Jung (2019). "Environmental triggers for chronic cough". Asia Pacific Allergy. 9 (2). doi:10.5415/apallergy.2019.9.e16. ISSN 2233-8276.
- ↑ Benich JJ, Carek PJ (October 2011). "Evaluation of the patient with chronic cough". Am Fam Physician. 84 (8): 887–92. PMID 22010767.
- ↑ Mello CJ, Irwin RS, Curley FJ (May 1996). "Predictive values of the character, timing, and complications of chronic cough in diagnosing its cause". Arch Intern Med. 156 (9): 997–1003. PMID 8624180.
- ↑ Rudolph, Colin D.; Mazur, Lynnette J.; Liptak, Gregory S.; Baker, Robert D.; Boyle, John T.; Colletti, Richard B.; Gerson, William T.; Werlin, Steven L. (2001). "Guidelines for Evaluation and Treatment of Gastroesophageal Reflux in Infants and Children". Journal of Pediatric Gastroenterology and Nutrition. 32: S1–S31. doi:10.1097/00005176-200100002-00001. ISSN 0277-2116.
- ↑ Pratter, Melvin R. (2006). "Chronic Upper Airway Cough Syndrome Secondary to Rhinosinus Diseases (Previously Referred to as Postnasal Drip Syndrome )". Chest. 129 (1): 63S–71S. doi:10.1378/chest.129.1_suppl.63S. ISSN 0012-3692.
- ↑ Turner, Richard D.; Bothamley, Graham H. (2015). "Cough and the Transmission of Tuberculosis". The Journal of Infectious Diseases. 211 (9): 1367–1372. doi:10.1093/infdis/jiu625. ISSN 0022-1899.
- ↑ MacIntyre, C Raina; Bourouiba, Lydia; Chughtai, Abrar Ahmad; de Silva, Charitha; Doolan, Con; Bahl, Prateek (2020). "Airborne or Droplet Precautions for Health Workers Treating Coronavirus Disease 2019?". The Journal of Infectious Diseases. doi:10.1093/infdis/jiaa189. ISSN 0022-1899.
- ↑ McEwan, J. R.; Choudry, N.; Street, R.; Fuller, R. W. (1989). "Change in cough reflex after treatment with enalapril and ramipril". BMJ. 299 (6690): 13–16. doi:10.1136/bmj.299.6690.13. ISSN 0959-8138.