Conjunctivitis
For patient information click here
Template:DiseaseDisorder infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Conjunctivitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Conjunctivitis On the Web |
|
American Roentgen Ray Society Images of Conjunctivitis |
Overview
Historical Perspective
Pathophysiology
Epidemiology & Demographics
Risk Factors
Screening
Causes
Differentiating Conjunctivitis
Complications & Prognosis
Diagnosis
History and Symptoms | Physical Examination | Staging | Laboratory tests | Electrocardiogram | X Rays | CT | MRI Echocardiography or Ultrasound | Other images | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Primary prevention | Secondary prevention | Financial costs | Future therapies
Diagnosis
Physical Examination
Eyes
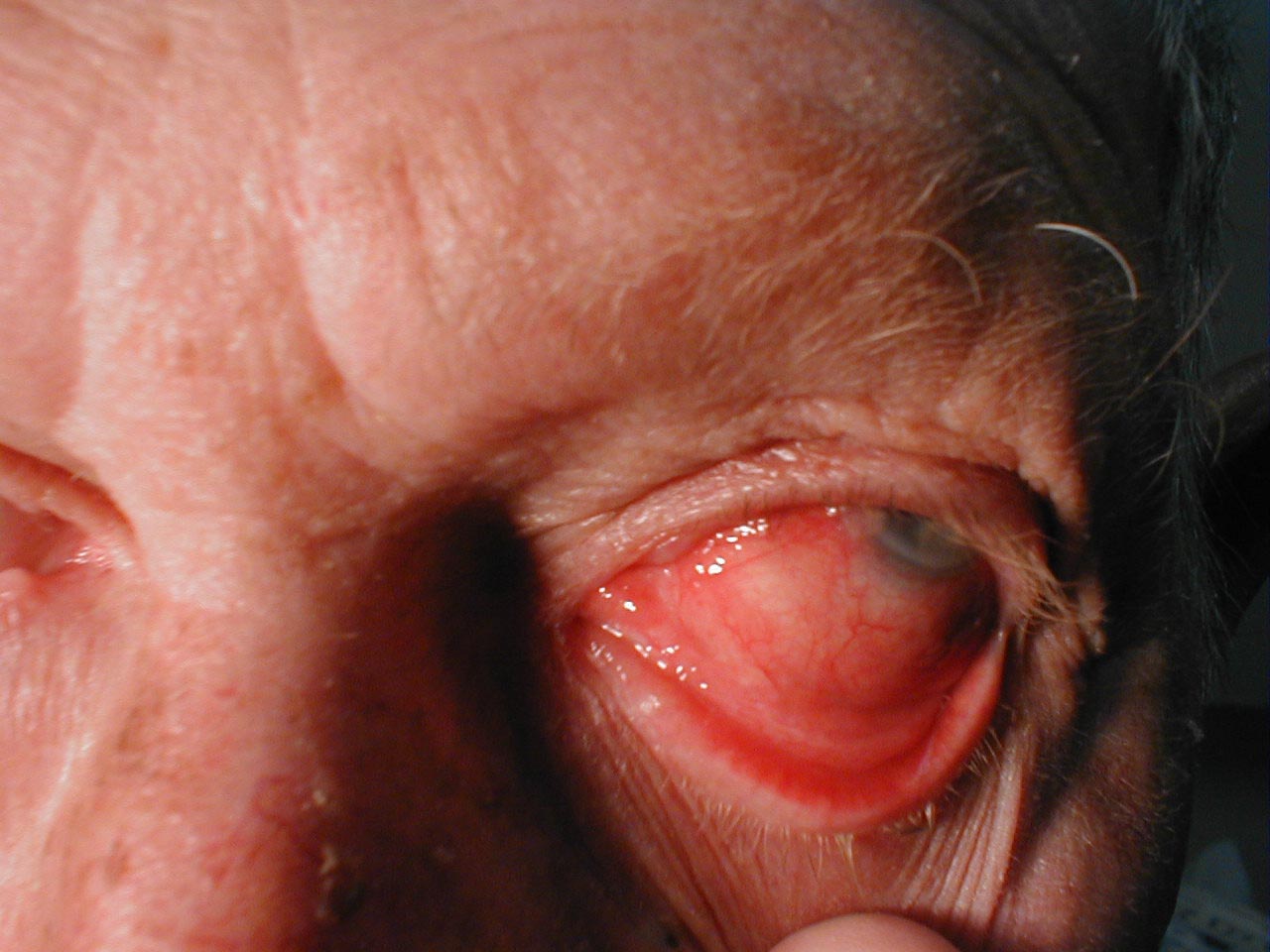
(Images shown below are courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
-
Conjunctivitis: Note inflamed conjunctiva of sclera and reflection onto underside of eyelid.
-
Conjunctivitis: Marked bilateral inflammation involving conjunctiva that covers sclera and under surface of eyelid. Thick exudate can also be seen.
-
Conjunctivitis: Inflammation of conjunctiva covering sclera and under surface of eyelid.
Pathology
Signs
Infection (redness) of the conjunctiva on one or both eyes should be apparent, but may be quite mild. Except in obvious pyogenic or toxic/chemical conjunctivitis, a slit lamp (biomicroscope) is needed to have any confidence in the diagnosis. Examination of the tarsal conjunctiva is usually more diagnostic than the bulbar conjunctiva.
Allergic conjunctivitis shows pale watery swelling or edema of the conjunctiva and sometimes the whole eyelid, often with a ropy, non-purulent mucoid discharge. There is variable redness. Viral conjunctivitis, commonly known as "pink eye", shows a fine diffuse pinkness of the conjunctiva which is easily mistaken for the 'ciliary infection' of iritis, but there are usually corroborative signs on biomicroscopy, particularly numerous lymphoid follicle12:02, 22 January 2008 (EST)12:02, 22 January 2008 (EST)~~s on the tarsal conjunctiva, and sometimes a punctate keratitis.
Pyogenic bacterial conjunctivitis shows an opaque purulent discharge, a very red eye, and on biomicroscopy there are numerous white cells and desquamated epithelial cells seen in the 'tear gutter' along the lid margin. The tarsal conjunctiva is a velvety red and not particularly follicular. Non-pyogenic infections can show just mild injection and be difficult to diagnose. Scarring of the tarsal conjunctiva is occasionally seen in chronic infections, especially in trachoma.
Irritant or toxic conjunctivitis show primarily marked redness. If due to splash injury, it is often present only in the lower conjunctival sac. With some chemicals—above all with caustic alkalis such as sodium hydroxide—there may be necrosis of the conjunctiva with a deceptively white eye due to vascular closure, followed by sloughing of the dead epithelium. This is likely to be associated with slit-lamp evidence of anterior uveitis.
Differential diagnosis
Conjunctivitis symptoms and signs are relatively non-specific. Even after biomicrosopy, laboratory tests are often necessary if proof of aetiology is needed.
A purulent discharge strongly suggests bacterial cause, unless there is known exposure to toxins. Infection with Neisseria gonorrhoeae should be suspected if the discharge is particularly thick and copious.
A diffuse, less "injected" conjunctivitis (looking pink rather than red) suggests a viral cause, especially if numerous follicles are present on the lower tarsal conjunctiva on biomicroscopy.
Scarring of the tarsal conjunctiva suggests trachoma, especially if seen in endemic areas, if the scarring is linear (von Arlt's line), or if there is also corneal vascularisation.
Clinical tests for lagophthalmos, dry eye (Schirmer test) and unstable tear film may help distinguish the various types of dry eye.
Other symptoms including pain, blurring of vision and photophobia should not be prominent in conjunctivitis. Fluctuating blurring is common, due to tearing and mucoid discharge. Mild photophobia is common. However, if any of these symptoms are prominent, it is important to exclude other diseases such as glaucoma, uveitis, keratitis and even meningitis or caroticocavernous fistula.
Investigations
These are done infrequently because most cases of conjunctivitis are treated empirically and (eventually) successfully, but often only after running the gamut of the common possibilities.
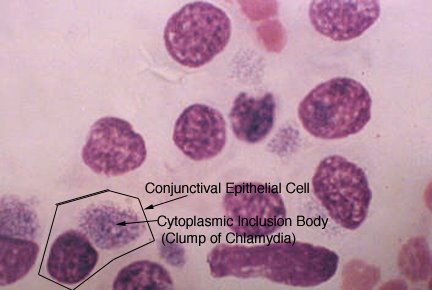
Swabs for bacterial culture are necessary if the history & signs suggest bacterial conjunctivitis, but there is no response to topical antibiotics. Research studies indicate that many bacteria implicated in low-grade conjunctivitis are not detected by the usual culture methods of medical microbiology labs, so negative results are common. Viral culture may be appropriate in epidemic case clusters. Conjunctival scrapes for cytology can be useful in detecting chlamydial and fungal infections, allergy and dysplasia, but are rarely done because of the cost and the general lack of laboratory staff experienced in handling ocular specimens. Conjunctival incisional biopsy is occasionally done when granulomatous diseases (e.g., sarcoidosis) or dysplasia are suspected.
Treatment and management
Conjunctivitis sometimes requires medical attention. The appropriate treatment depends on the cause of the problem. For the allergic type, cool water constricts capillaries, and artificial tears sometimes relieve discomfort in mild cases. In more severe cases, non-steroidal anti-inflammatory medications and antihistamines may be prescribed. Some patients with persistent allergic conjunctivitis may also require topical steroid drops.
Bacterial conjunctivitis is usually treated with antibiotic eye drops or ointments that cover a broad range of bacteria (chloramphenicol or fusidic acid used in UK). However evidence suggests that this does not affect symptom severity and gains only modest reduction in duration from an average of 4.8 days (untreated controls) to 3.3 days for those given immediate antibiotics. Deferring antibiotics yields almost the same duration as those immediately starting treatment with 3.9 days duration, but with half the two-week clinic reattendance rate.[4]
Although there is no cure for viral conjunctivitis, symptomatic relief may be achieved with cool compresses and artificial tears. For the worst cases, topical corticosteroid drops may be prescribed to reduce the discomfort from inflammation. However prolonged usage of corticosteroid drops increases the risk of side effects. Antibiotic drops may also be used for treatment of complementary infections. Patients are often advised to avoid touching their eyes or sharing towels and washcloths. Viral conjunctivitis usually resolves within 3 weeks. However in worst cases it may take over a month.
Conjunctivitis due to burns, toxic and chemical require careful wash-out with saline, especially beneath the lids, and may require topical steroids. The more acute chemical injuries are medical emergencies, particularly alkali burns, which can lead to severe scarring, and intraocular damage. Fortunately, such injuries are uncommon.
Footnotes
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages/
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages/
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ Hazel A Everitt, Paul S Little, Peter W F Smith (2006). "A randomised controlled trial of management strategies for acute infective conjunctivitis in general practice". BMJ.Error: Bad DOI specified!. Unknown parameter
|month=ignored (help)
External links
- Facts About the Cornea and Corneal Disease The National Eye Institute (NEI).
- All About Conjunctivitis
de:Konjunktivitis eo:Konjunktivito hr:Konjunktivitis id:Konjungtivitis it:Congiuntivite nl:Bindvliesontsteking no:Konjunktivitt qu:Ñawi huñuna unquy simple:Conjunctivitis fi:Sidekalvontulehdus

![Bacterial Conjunctivitis[1]](/images/b/b4/Bacterial_Conjunctivitis.jpg)
![Chemical Conjunctivits[2]](/images/a/ab/Chemical_conjunctivits_%28day1-2%29.jpg)