Congenital adrenal hyperplasia Overview: Difference between revisions
(Created page with "__NOTOC__ {{Congenital adrenal hyperplasia}} {{CMG}}; {{AE}}{{MJ}} {{SK}} Congenital adrenal hyperplasia, CAH, Adrenal hyperplasia ==Overview== Congenital adrenal hyperplas...") |
No edit summary |
||
| Line 9: | Line 9: | ||
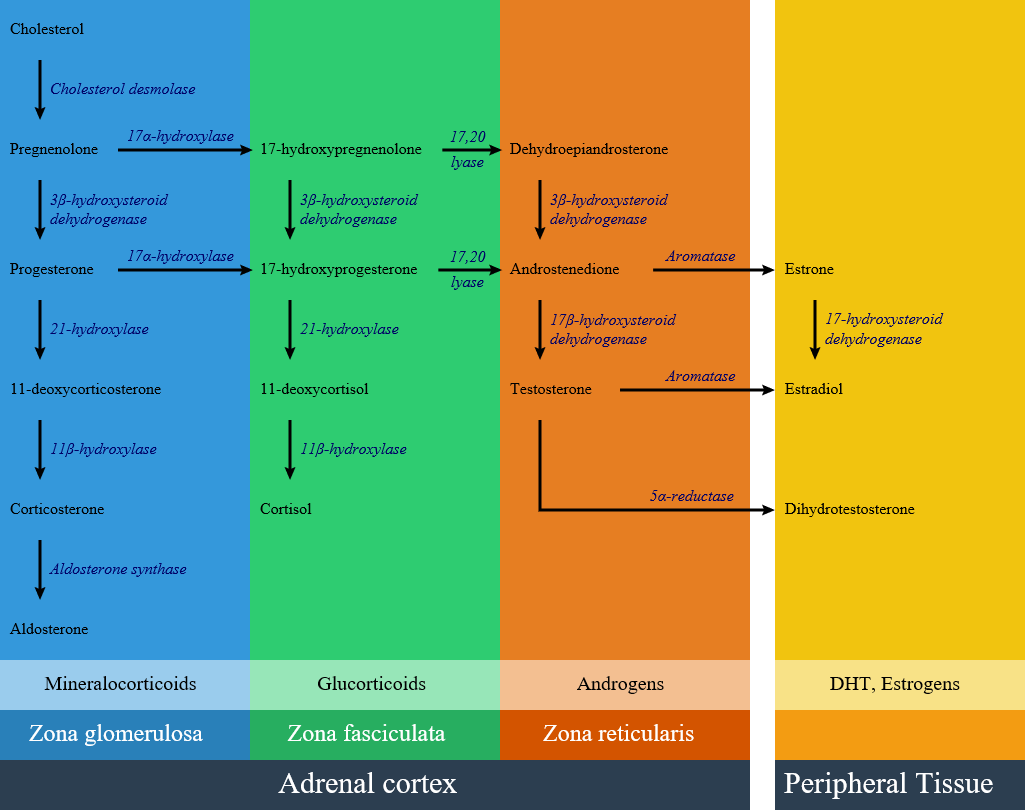
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. | Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. | ||
Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema. | Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema. | ||
==Historical Perspective== | |||
* Congenital adrenal hyperplasia first time seen in 1865 by Luigi De Crecchio, an Italian [[pathologist]], in a man at autopsy, who had large [[adrenal glands]] and female [[internal organs]]. | |||
* Important aspects of discovering [[adrenal]] hormones:<ref name="pmid25635623">{{cite journal |vauthors=Delle Piane L, Rinaudo PF, Miller WL |title=150 years of congenital adrenal hyperplasia: translation and commentary of De Crecchio's classic paper from 1865 |journal=Endocrinology |volume=156 |issue=4 |pages=1210–7 |year=2015 |pmid=25635623 |doi=10.1210/en.2014-1879 |url=}}</ref><ref name="ISBN:978-0323297387">{{cite book | last = Melmed | first = Shlomo | title = Williams textbook of endocrinology | publisher = Elsevier | location = Philadelphia, PA | year = 2016 | isbn = 978-0323297387 }}=</ref><ref name="pmid18118071">{{cite journal |vauthors=HENCH PS, KENDALL EC |title=The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis |journal=Proc Staff Meet Mayo Clin |volume=24 |issue=8 |pages=181–97 |year=1949 |pmid=18118071 |doi= |url=}}</ref><ref name="pmid4288776">{{cite journal |vauthors=Biglieri EG, Herron MA, Brust N |title=17-hydroxylation deficiency in man |journal=J. Clin. Invest. |volume=45 |issue=12 |pages=1946–54 |year=1966 |pmid=4288776 |pmc=292880 |doi=10.1172/JCI105499 |url=}}</ref> | |||
** In 1563, Eustachius described the [[Adrenal|adrenals]] and then published by Lancisi in 1714. | |||
** In 1849, [[Thomas Addison]], found on a bronzed appearance associated with the [[adrenal glands]] called [[melasma]] suprarenale while searching for the cause of [[pernicious anemia]]. | |||
** In 1855, [[Thomas Addison]] defined the clinical features and [[autopsy]] findings in 11 cases of diseases of the [[suprarenal]] capsules, and half of them were [[tuberculous]] in origin. | |||
** In 1856, In [[adrenalectomy]] experiments, [[Brown-Sequard syndrome|Brown-Séquard]] found that the [[adrenal glands]] are nessesary for life. | |||
** In 1896, [[William Osler]] prepared an oral glycerin extract derived from pig [[Adrenal|adrenals]] and showed that it had clinical benefit in patients with [[Addison disease]]. | |||
** In 1905, Bulloch and Sequeira described patients with [[congenital adrenal hyperplasia]]. | |||
** In 1936, Selye described the concept of stress and its effect on [[pituitary]]-[[adrenal]] function. | |||
** In 1937-1952, Kendall and Reichstein, defined the isolation and structural characterization of [[Adrenocortical hormone|adrenocortical hormones]]. | |||
** In 1943, Li and colleagues isolated [[adrenocorticotropic hormone]] from sheep [[pituitary]]. | |||
** In 1950, Hench, Kendall, and Reichstein shared the [[Nobel Prize in Medicine]] for describing the [[anti-inflammatory]] effects of [[cortisone]] in patients with [[rheumatoid arthritis]] | |||
** In 1956, Conn described [[primary aldosteronism]]. | |||
** In 1981, Vale defined characterization and synthesis of [[corticotropin-releasing hormone]]. | |||
** From 1980-present called the molecular era; highlights in this section are: | |||
*** Cloning and functional characterization of [[Steroid hormone receptor|steroid hormone receptors]] discovered. | |||
*** [[Steroidogenic]] [[enzymes]] described. | |||
*** [[Adrenal]] [[transcription factors]] were reported. | |||
*** [[Molecular]] basis for human adrenal diseases described. | |||
==Pathophisiology== | ==Pathophisiology== | ||
| Line 20: | Line 42: | ||
! align="center" style="background:#DCDCDC;" rowspan="2" colspan="2" |Disease | ! align="center" style="background:#DCDCDC;" rowspan="2" colspan="2" |Disease | ||
! align="center" style="background:#DCDCDC;" colspan="2" |History and symptoms | ! align="center" style="background:#DCDCDC;" colspan="2" |History and symptoms | ||
! align="center" style="background:#DCDCDC;" colspan=" | ! align="center" style="background:#DCDCDC;" colspan="3" |Laboratory findings | ||
! align="center" style="background:#DCDCDC;" |Defective gene | ! align="center" style="background:#DCDCDC;" |Defective gene | ||
|- | |- | ||
!Blood pressure | !Blood pressure | ||
!Genitalia | !Genitalia | ||
! | !Increased | ||
!Decreased | |||
!K levels | !K levels | ||
! | ! | ||
| Line 40: | Line 63: | ||
* Male: normal or scrotal pigmentation and large phallus | * Male: normal or scrotal pigmentation and large phallus | ||
| | | | ||
* [[Deoxycorticosterone]] | |||
* | * 11-Deoxy-[[cortisol]] | ||
* | * [[17-Hydroxyprogesterone|17-hydroxyprogesterone]], mild elevation | ||
| | |||
* [[Cortisol]] | |||
* [[Corticosterone]] | |||
* | * [[Aldosterone]] | ||
* Corticosterone | |||
* | |||
| | | | ||
* High in salt wasting type | * High in salt wasting type | ||
| Line 61: | Line 82: | ||
* Female: virilization after puberty | * Female: virilization after puberty | ||
* Male: normal appearance | * Male: normal appearance | ||
| | | | ||
* 17- | * [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | ||
* Exaggerated | * Exaggerated [[Androstenedione]], [[DHEA]], and [[17-Hydroxyprogesterone|17-hydroxyprogesterone]] | ||
response to ACTH | response to [[ACTH]] | ||
| | |||
| | | | ||
* Normal | * Normal | ||
| Line 70: | Line 92: | ||
* CYP21A1 and CYP21A2 gene | * CYP21A1 and CYP21A2 gene | ||
|- | |- | ||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" | | | align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |[[17 alpha-hydroxylase deficiency|17-α hydroxylase deficiency]] | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* Hypertension | * Hypertension | ||
| Line 77: | Line 99: | ||
* Male: ambiguous | * Male: ambiguous | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | * [[Deoxycorticosterone]] | ||
* [[Corticosterone]] | |||
* | * [[Progesterone]] | ||
| | |||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
| | | | ||
* Low | * Low | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | * CYP17A1 | ||
|- | |- | ||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |11β-hydroxylase deficiency | | align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |[[11β-hydroxylase deficiency|11-β hydroxylase deficiency]] | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* Hypertension | * Hypertension | ||
| Line 93: | Line 118: | ||
* Male: normal or scrotal pigmentation and large phallus | * Male: normal or scrotal pigmentation and large phallus | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | * [[Deoxycorticosterone]] | ||
* 11-Deoxy-[[cortisol]] | |||
* | * [[17-Hydroxyprogesterone|17-hydroxyprogesterone]], mild elevation | ||
| | |||
* [[Cortisol]] | |||
* [[Corticosterone]] | |||
* [[Aldosterone]] | |||
| | | | ||
* Low | * Low | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* | * CYP11B1 | ||
|- | |- | ||
| align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" | | | align="center" style="padding: 5px 5px; background: #DCDCDC;" colspan="2" |3β-Hydroxysteroid Dehydrogenase | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | |||
| | |||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
* [[Dehydroepiandrosterone]] | |||
* [[17-hydroxypregnenolone]] | |||
* [[Pregnenolone]] | |||
| | | | ||
* [[Cortisol]] | |||
* [[Aldosterone]] | |||
* Cortisol | |||
* Aldosterone | |||
| | | | ||
* High | * High | ||
| Line 119: | Line 148: | ||
| | | | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
| | |||
| | | | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
| Line 126: | Line 156: | ||
| | | | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
| | |||
| | | | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
| Line 133: | Line 164: | ||
| | | | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
| | |||
| | | | ||
| align="center" style="padding: 5px 5px; background: #F5F5F5;" | | | align="center" style="padding: 5px 5px; background: #F5F5F5;" | | ||
Revision as of 18:57, 1 August 2017
|
Congenital adrenal hyperplasia main page |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mehrian Jafarizade, M.D [2]
Synonyms and keywords: Congenital adrenal hyperplasia, CAH, Adrenal hyperplasia
Overview
Congenital adrenal hyperplasia (CAH) refers to any of several autosomal recessive conditions resulting from biochemical paths of the steroidogenesis of cortisol from cholesterol by the adrenal glands. Most of these conditions involve greater or lesser production of sex steroids and can alter development of primary or secondary sex characteristics in affected infants, children, and adults. Only a small minority of people with CAH can be said to have an intersex condition, but this attracted American public attention in the late 1990s and many accounts of varying accuracy have appeared in the popular media. Approximately 95% of cases of CAH are due to 21-hydroxylase deficiency. Prenatal diagnosis can be made in both of these disorders by chorionic villous sampling, but this can only be done at 8-10 weeks. In order to prevent the deleterious effect of excess androgens on genital (and brain!) development, therapy must be started earlier. This is most often considered if there is an affected sibling. Treatment is dexamethasone, which is not degraded by the placenta, but is associated with significant maternal weight gain, hypertension, and edema.
Historical Perspective
- Congenital adrenal hyperplasia first time seen in 1865 by Luigi De Crecchio, an Italian pathologist, in a man at autopsy, who had large adrenal glands and female internal organs.
- Important aspects of discovering adrenal hormones:[1][2][3][4]
- In 1563, Eustachius described the adrenals and then published by Lancisi in 1714.
- In 1849, Thomas Addison, found on a bronzed appearance associated with the adrenal glands called melasma suprarenale while searching for the cause of pernicious anemia.
- In 1855, Thomas Addison defined the clinical features and autopsy findings in 11 cases of diseases of the suprarenal capsules, and half of them were tuberculous in origin.
- In 1856, In adrenalectomy experiments, Brown-Séquard found that the adrenal glands are nessesary for life.
- In 1896, William Osler prepared an oral glycerin extract derived from pig adrenals and showed that it had clinical benefit in patients with Addison disease.
- In 1905, Bulloch and Sequeira described patients with congenital adrenal hyperplasia.
- In 1936, Selye described the concept of stress and its effect on pituitary-adrenal function.
- In 1937-1952, Kendall and Reichstein, defined the isolation and structural characterization of adrenocortical hormones.
- In 1943, Li and colleagues isolated adrenocorticotropic hormone from sheep pituitary.
- In 1950, Hench, Kendall, and Reichstein shared the Nobel Prize in Medicine for describing the anti-inflammatory effects of cortisone in patients with rheumatoid arthritis
- In 1956, Conn described primary aldosteronism.
- In 1981, Vale defined characterization and synthesis of corticotropin-releasing hormone.
- From 1980-present called the molecular era; highlights in this section are:
- Cloning and functional characterization of steroid hormone receptors discovered.
- Steroidogenic enzymes described.
- Adrenal transcription factors were reported.
- Molecular basis for human adrenal diseases described.
Pathophisiology
Classification
Congenital adrenal hyperplasia is classified into seven types based on the genetic causes that lead to hyperplasia and hormonal imbalance.
| Disease | History and symptoms | Laboratory findings | Defective gene | ||||
|---|---|---|---|---|---|---|---|
| Blood pressure | Genitalia | Increased | Decreased | K levels | |||
| 21-hydroxylase deficiency | Classic type |
|
|
|
|
| |
| Non-classic type |
|
|
response to ACTH |
|
| ||
| 17-α hydroxylase deficiency |
|
|
|
| |||
| 11-β hydroxylase deficiency |
|
|
|
|
| ||
| 3β-Hydroxysteroid Dehydrogenase |
|
||||||
| Cytochrome P450-oxidoreductase (POR) deficiency (ORD) | |||||||
| Congenital lipoid adrenal hyperplasia | |||||||
| Cholesterol side-chain cleavage enzyme deficiency | |||||||
Prevention
References
- ↑ Delle Piane L, Rinaudo PF, Miller WL (2015). "150 years of congenital adrenal hyperplasia: translation and commentary of De Crecchio's classic paper from 1865". Endocrinology. 156 (4): 1210–7. doi:10.1210/en.2014-1879. PMID 25635623.
- ↑ Melmed, Shlomo (2016). Williams textbook of endocrinology. Philadelphia, PA: Elsevier. ISBN 978-0323297387.=
- ↑ HENCH PS, KENDALL EC (1949). "The effect of a hormone of the adrenal cortex (17-hydroxy-11-dehydrocorticosterone; compound E) and of pituitary adrenocorticotropic hormone on rheumatoid arthritis". Proc Staff Meet Mayo Clin. 24 (8): 181–97. PMID 18118071.
- ↑ Biglieri EG, Herron MA, Brust N (1966). "17-hydroxylation deficiency in man". J. Clin. Invest. 45 (12): 1946–54. doi:10.1172/JCI105499. PMC 292880. PMID 4288776.