Chylothorax: Difference between revisions
| (58 intermediate revisions by the same user not shown) | |||
| Line 14: | Line 14: | ||
}} | }} | ||
{{SI}} | {{SI}} | ||
{{CMG}}''' Associate Editor:''' {{JE}} | |||
{{SK}} Chylothorax | |||
==Overview== | ==Overview== | ||
Chylothorax, a type of [[pleural effusion]] is the accumulation of [[chyle]] in the [[pleural cavity]] secondary to destruction or obstruction of the [[thoracic duct]] or its tributaries. It is an uncommon but established complication of [[thoracic surgery]]. Chylothorax is most commonly right-sided (50%) because of the anatomic location of the [[thoracic duct]], left-sided (33.3%), or bilateral (16.66%). [[Thoracic duct]] damage above the fifth [[Thoracic vertebrae|thoracic vertebra]] results in a left-sided chylothorax whereas damage to the [[thoracic duct]] below fifth [[Thoracic vertebrae|thoracic vertebra]] leads to a right-sided effusion. Some common symptoms of chylothorax include [[dyspnea]], [[cough]], and severe [[chest pain]]. Some physical exams finding include decreased [[breath sounds]] and dullness to [[percussion]] depending on the size and location of fluid. The definitive diagnosis of chylothorax is with [[thoracentesis]] and analysis of the [[Pleural effusion|pleural fluid]] showing a reduced concentration of [[cholesterol]] <200mg/dl, and an elevated concentration of [[triglyceride]] >110 mg/dl. Management of chylothorax may be conservative or surgical. Conservative management include [[total parenteral nutrition]], oral low-fat medium-chain [[triglyceride]], and [[octreotide injection]]s. Surgical management include [[Chest tube|tube thoracostomy]], [[pleurodesis]], pleurectomy, pleuroperitoneal shunt, and [[thoracic duct]] ligation. | Chylothorax, a type of [[ pleural effusion]] is the accumulation of [[chyle]] in the [[pleural cavity]] secondary to destruction or obstruction of the [[thoracic duct]] or its tributaries. Depending on the etiology, chylothorax could be [[Pleural effusion classification|exudative]] ( [[tuberculosis]]) or [[Pleural effusion classification|transudative]] ([[Superior vena cava syndrome|svc obstruction]]). It is an uncommon but established complication of [[thoracic surgery]]. Chylothorax is most commonly right-sided (50%) because of the anatomic location of the [[thoracic duct]], left-sided (33.3%), or bilateral (16.66%). [[Thoracic duct]] damage above the fifth [[Thoracic vertebrae|thoracic vertebra]] results in a left-sided chylothorax whereas damage to the [[thoracic duct]] below fifth [[Thoracic vertebrae|thoracic vertebra]] leads to a right-sided effusion. Some common symptoms of chylothorax include [[dyspnea]], [[cough]], and severe [[chest pain]]. Some physical exams finding include decreased [[breath sounds]] and dullness to [[percussion]] depending on the size and location of fluid. The definitive diagnosis of chylothorax is with [[thoracentesis]] and analysis of the [[Pleural effusion|pleural fluid]] showing a reduced concentration of [[cholesterol]] <200mg/dl, and an elevated concentration of [[triglyceride]] >110 mg/dl. Management of chylothorax may be conservative or surgical. Conservative management include [[total parenteral nutrition]], oral low-fat medium-chain [[triglyceride]], and [[octreotide injection]]s. Surgical management include [[Chest tube|tube thoracostomy]], [[pleurodesis]], pleurectomy, pleuroperitoneal shunt, and [[thoracic duct]] ligation. | ||
==Historical Perspective== | ==Historical Perspective== | ||
| Line 84: | Line 87: | ||
==Pathophysiology== | ==Pathophysiology== | ||
It is thought that chylothorax is the result of leakage of [[chyle]] | *It is thought that chylothorax is the result of obstruction, difficulty in drainage of [[Lymphatic system|lymph]], [[Lymphatic system|lymphatic malformation]] or laceration of the [[thoracic duct]] leading to leakage of [[chyle]] into the [[pleural cavity]].<ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
*Chylothorax as a result of [[tuberculosis]] is thought to be | *Chylothorax as a result of [[tuberculosis]] is thought to be produced by the enlargement of the [[Lumbar lymph nodes|lumbar]] and the [[iliac lymph node]]s producing obstruction of the [[cisterna chyli]] and [[thoracic duct]]. This leads to dilatation of the [[Lumbar lymph nodes|lumbar]] channels, followed by the opening of collateral [[anastomosis]]. With the many lymphaticovenous [[anastomosis]] existing between the [[thoracic duct]], and the [[Azygos vein|azygos]], [[Intercostal veins|intercostal]], and [[Lumbar veins]]. The increased pressure in the system results in the transudation of [[chyle]] into the [[pleural cavity]].<ref name="pmid21654988">{{cite journal| author=Kant S, Verma SK, Anand SC, Prasad R, Verma RK| title=Development of bilateral chylothorax in a younger female secondary to tuberculosis. | journal=Lung India | year= 2011 | volume= 28 | issue= 1 | pages= 56-9 | pmid=21654988 | doi=10.4103/0970-2113.76303 | pmc=3099513 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21654988 }} </ref> | ||
==Causes== | ==Causes== | ||
*Common causes of chylothorax include<ref name="pmid21654988">{{cite journal| author=Kant S, Verma SK, Anand SC, Prasad R, Verma RK| title=Development of bilateral chylothorax in a younger female secondary to tuberculosis. | journal=Lung India | year= 2011 | volume= 28 | issue= 1 | pages= 56-9 | pmid=21654988 | doi=10.4103/0970-2113.76303 | pmc=3099513 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21654988 }} </ref><ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid29316546">{{cite journal| author=Rajagopala S, Kancherla R, Ramanathan RP| title=Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature. | journal=Respiration | year= 2018 | volume= 95 | issue= 4 | pages= 260-268 | pmid=29316546 | doi=10.1159/000484694 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29316546 }} </ref> | *Common causes of chylothorax include<ref name="pmid21654988">{{cite journal| author=Kant S, Verma SK, Anand SC, Prasad R, Verma RK| title=Development of bilateral chylothorax in a younger female secondary to tuberculosis. | journal=Lung India | year= 2011 | volume= 28 | issue= 1 | pages= 56-9 | pmid=21654988 | doi=10.4103/0970-2113.76303 | pmc=3099513 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21654988 }} </ref><ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref><ref name="pmid29316546">{{cite journal| author=Rajagopala S, Kancherla R, Ramanathan RP| title=Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature. | journal=Respiration | year= 2018 | volume= 95 | issue= 4 | pages= 260-268 | pmid=29316546 | doi=10.1159/000484694 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29316546 }} </ref><ref name="pmid19882503">{{cite journal| author=Waterfield T, Lakhoo K| title=Challenges in the management of refractory bilateral idiopathic congenital chylothoraces in a newborn. | journal=Eur J Pediatr Surg | year= 2010 | volume= 20 | issue= 3 | pages= 198-201 | pmid=19882503 | doi=10.1055/s-0029-1241874 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19882503 }} </ref><ref name="pmid31338288">{{cite journal| author=Austin A, Al-Faris F, Modi A, Chopra A| title=A transudative chylothorax associated with superior vena cava syndrome. | journal=Respir Med Case Rep | year= 2019 | volume= 28 | issue= | pages= 100898 | pmid=31338288 | doi=10.1016/j.rmcr.2019.100898 | pmc=6626116 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31338288 }} </ref> | ||
**[[Congenital disorder|Congenital]] | |||
***[[Down syndrome]] | |||
***[[Noonan syndrome]] | |||
***[[Turner syndrome]] | |||
**[[Cancer|Malignacy]] | **[[Cancer|Malignacy]] | ||
**[[Sarcoidosis]] | **[[Sarcoidosis]] | ||
**[[Tuberculosis]] | **[[Tuberculosis]] | ||
**[[Cirrhosis]] | |||
**[[Congestive heart failure|Heart failure]] | **[[Congestive heart failure|Heart failure]] | ||
**[[Benign tumor]] | **[[Benign tumor]] | ||
| Line 103: | Line 111: | ||
== Differentiating chylothorax from other Diseasess == | == Differentiating chylothorax from other Diseasess == | ||
Chylothorax must be differentiated from<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref> <ref>Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016</ref> <ref>Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X</ref> | Chylothorax must be differentiated from<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref> <ref>Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016</ref> <ref>Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X</ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
*[[Empyema]] | *[[Empyema]] | ||
*Pseudochylothorax | *Pseudochylothorax | ||
*[[Cholesterol]] [[pleural effusion]]s | |||
*[[Tuberculosis]] | *[[Tuberculosis]] | ||
*Chronic [[pneumothorax]] | *Chronic [[pneumothorax]] | ||
| Line 119: | Line 128: | ||
* The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide. | * The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide. | ||
*In 2011, the incidence of pediatric chylothorax was estimated to be 3.7%<ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref> <ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | *In 2011, the incidence of pediatric chylothorax was estimated to be 3.7%<ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref> <ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | ||
*Incidence post [[Cardiac surgery|cardiothoracic surgeries]] are between 0.9% and 6.6%. | |||
**Incidence post [[Congenital heart disease|congenital cardiac anomalies]] repair is 2.8%. | |||
*Incidence post [[esophageal]] surgeries range from 0.2% to 10%. | |||
===Age=== | ===Age=== | ||
| Line 127: | Line 136: | ||
===Gender=== | ===Gender=== | ||
* | *Chylothorax affects men and women equally. | ||
===Race=== | ===Race=== | ||
*There is no racial predilection for | *There is no racial predilection for chylothorax. | ||
==Risk Factors== | ==Risk Factors== | ||
Common risk factors in the development of Chylothorax] are<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid29249497">{{cite journal| author=Lo Rito M, Al-Radi OO, Saedi A, Kotani Y, Ben Sivarajan V, Russell JL | display-authors=etal| title=Chylothorax and pleural effusion in contemporary extracardiac fenestrated fontan completion. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 5 | pages= 2069-2077 | pmid=29249497 | doi=10.1016/j.jtcvs.2017.11.046 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29249497 }} </ref><ref name="pmid31292394">{{cite journal| author=Sasaki H, Kimizuka Y, Ogata H, Okada Y, Ota S, Sano T | display-authors=etal| title=Successful Control of Dasatinib-related Chylothorax by the Japanese Herbal Medicine "Goreisan". | journal=Intern Med | year= 2019 | volume= 58 | issue= 21 | pages= 3139-3141 | pmid=31292394 | doi=10.2169/internalmedicine.3002-19 | pmc=6875454 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31292394 }} </ref><ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref><ref name="pmid29106894">{{cite journal| author=Nicastri DG, Flores RM| title=Chylothorax: Abdominal approach. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 814 | pmid=29106894 | doi=10.1016/j.jtcvs.2017.09.111 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29106894 }} </ref><ref name="pmid17251600">{{cite journal| author=Townshend AP, Speake W, Brooks A| title=Chylothorax. | journal=Emerg Med J | year= 2007 | volume= 24 | issue= 2 | pages= e11 | pmid=17251600 | doi=10.1136/emj.2006.042028 | pmc=2658219 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17251600 }} </ref><ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid30626415">{{cite journal| author=Pospiskova J, Smolej L, Belada D, Simkovic M, Motyckova M, Sykorova A | display-authors=etal| title=Experiences in the treatment of refractory chylothorax associated with lymphoproliferative disorders. | journal=Orphanet J Rare Dis | year= 2019 | volume= 14 | issue= 1 | pages= 9 | pmid=30626415 | doi=10.1186/s13023-018-0991-3 | pmc=6327395 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30626415 }} </ref><ref name="pmid29316546">{{cite journal| author=Rajagopala S, Kancherla R, Ramanathan RP| title=Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature. | journal=Respiration | year= 2018 | volume= 95 | issue= 4 | pages= 260-268 | pmid=29316546 | doi=10.1159/000484694 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29316546 }} </ref> | Common risk factors in the development of Chylothorax] are<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid29249497">{{cite journal| author=Lo Rito M, Al-Radi OO, Saedi A, Kotani Y, Ben Sivarajan V, Russell JL | display-authors=etal| title=Chylothorax and pleural effusion in contemporary extracardiac fenestrated fontan completion. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 5 | pages= 2069-2077 | pmid=29249497 | doi=10.1016/j.jtcvs.2017.11.046 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29249497 }} </ref><ref name="pmid31292394">{{cite journal| author=Sasaki H, Kimizuka Y, Ogata H, Okada Y, Ota S, Sano T | display-authors=etal| title=Successful Control of Dasatinib-related Chylothorax by the Japanese Herbal Medicine "Goreisan". | journal=Intern Med | year= 2019 | volume= 58 | issue= 21 | pages= 3139-3141 | pmid=31292394 | doi=10.2169/internalmedicine.3002-19 | pmc=6875454 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31292394 }} </ref><ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref><ref name="pmid29106894">{{cite journal| author=Nicastri DG, Flores RM| title=Chylothorax: Abdominal approach. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 814 | pmid=29106894 | doi=10.1016/j.jtcvs.2017.09.111 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29106894 }} </ref><ref name="pmid17251600">{{cite journal| author=Townshend AP, Speake W, Brooks A| title=Chylothorax. | journal=Emerg Med J | year= 2007 | volume= 24 | issue= 2 | pages= e11 | pmid=17251600 | doi=10.1136/emj.2006.042028 | pmc=2658219 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17251600 }} </ref><ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid30626415">{{cite journal| author=Pospiskova J, Smolej L, Belada D, Simkovic M, Motyckova M, Sykorova A | display-authors=etal| title=Experiences in the treatment of refractory chylothorax associated with lymphoproliferative disorders. | journal=Orphanet J Rare Dis | year= 2019 | volume= 14 | issue= 1 | pages= 9 | pmid=30626415 | doi=10.1186/s13023-018-0991-3 | pmc=6327395 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30626415 }} </ref><ref name="pmid29316546">{{cite journal| author=Rajagopala S, Kancherla R, Ramanathan RP| title=Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature. | journal=Respiration | year= 2018 | volume= 95 | issue= 4 | pages= 260-268 | pmid=29316546 | doi=10.1159/000484694 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29316546 }} </ref><ref name="pmid31341753">{{cite journal| author=Jacob S, Meneses A, Landolfo K, El-Sayed Ahmed M, Makey IA, Pham SM | display-authors=etal| title=Incidence, Management, and Outcomes of Chylothorax after Lung Transplantation: A Single-center Experience. | journal=Cureus | year= 2019 | volume= 11 | issue= 7 | pages= e5190 | pmid=31341753 | doi=10.7759/cureus.5190 | pmc=6649881 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31341753 }} </ref><ref name="pmid31292374">{{cite journal| author=Nagano N, Suzuki M, Tamura K, Kobayashi S, Kojima Y, Naka G | display-authors=etal| title=Refractory Chylothorax and Lymphedema Caused by Advanced Gastric Cancer. | journal=Intern Med | year= 2019 | volume= 58 | issue= 21 | pages= 3143-3148 | pmid=31292374 | doi=10.2169/internalmedicine.2351-18 | pmc=6875443 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31292374 }} </ref> | ||
*[[Hepatectomy]] | *[[Surgery]] | ||
*[[Esophagectomy]] | **[[Hepatectomy]] | ||
*[[Lung]] surgery | **[[Esophagectomy]] | ||
*[[Cardiac surgery]] | **[[Lung]] surgery | ||
*[[Fontan procedure]] | **[[Cardiac surgery]] | ||
*[[Retroperitoneum|Retroperitoneal]] surgery around the [[cisterna chyli]], example [[abdominal aortic aneurysm surgery|AAA repair]] | **[[Fontan procedure]] | ||
**[[Retroperitoneum|Retroperitoneal]] surgery around the [[cisterna chyli]], example [[abdominal aortic aneurysm surgery|AAA repair]] | |||
*[[Dasatinib]] therapy | *[[Dasatinib]] therapy | ||
*[[Rib fracture]] | *[[Rib fracture]] | ||
*[[Tuberculosis]] | *[[Tuberculosis]] | ||
*[[Stomach cancer|Gastric cancer]] | |||
*Malignant pleural [[mesothelioma]] | *Malignant pleural [[mesothelioma]] | ||
*Malignant [[lymphoproliferative disorders]] | *Malignant [[lymphoproliferative disorders]] | ||
==Screening== | ==Screening== | ||
*There is insufficient evidence to recommend routine screening for chylothorax. | |||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*If left untreated, 100% of patients with chylothorax may progress to develop<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref> | *If left untreated, 100% of patients with chylothorax may progress to develop<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref> | ||
**[[Hypovolaemia]] | **[[Hypovolaemia]] | ||
*[[Hypoalbuminemia]] | **[[Hypoalbuminemia]] | ||
**[[Malnutrition]]; as a result of [[protein]], [[fats]] and [[vitamin]]s loss with [[weight loss]] and [[Muscle atrophy|muscle wasting]]. | **[[Malnutrition]]; as a result of [[protein]], [[fats]] and [[vitamin]]s loss with [[weight loss]] and [[Muscle atrophy|muscle wasting]]. | ||
**[[Hyponatremia]] and [[hypocalcemia]] due to [[Electrolyte disturbance|electrolyte loss]]. | **[[Hyponatremia]] and [[hypocalcemia]] due to [[Electrolyte disturbance|electrolyte loss]]. | ||
**[[Opportunistic infection]]s as a result of [[Antibody|immunoglobulins]] loss. | **[[Opportunistic infection]]s as a result of [[Antibody|immunoglobulins]] loss. | ||
**Subtherapeutic effects of medications like [[digoxin]] and [[amiodarone]] as they are lost through the leaking [[chyle]]. | **Subtherapeutic effects of medications like [[digoxin]] and [[amiodarone]] as they are lost through the leaking [[chyle]]. | ||
*Common complications of chylothorax include [[malnutrition]], [[immunosuppression]] and [[respiratory distress]].<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref> | *Common complications of chylothorax include [[malnutrition]], [[immunosuppression]] and [[respiratory distress]].<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
*Prognosis is generally good and the [[mortality rate]] from chylothorax has considerably improved from approximately 50% as described in 1948. This is due to the more aggressive management plans implemented. Currently, the worst prognosis is seen in malignant and bilateral chylothoraces.<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid29106894">{{cite journal| author=Nicastri DG, Flores RM| title=Chylothorax: Abdominal approach. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 814 | pmid=29106894 | doi=10.1016/j.jtcvs.2017.09.111 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29106894 }} </ref> | *Prognosis is generally good and the [[mortality rate]] from chylothorax has considerably improved from approximately 50% as described in 1948. This is due to the more aggressive management plans implemented. Currently, the worst prognosis is seen in malignant and bilateral chylothoraces.<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref><ref name="pmid29106894">{{cite journal| author=Nicastri DG, Flores RM| title=Chylothorax: Abdominal approach. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 814 | pmid=29106894 | doi=10.1016/j.jtcvs.2017.09.111 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29106894 }} </ref> | ||
== Diagnosis == | == Diagnosis == | ||
===Diagnostic Study of Choice=== | ===Diagnostic Study of Choice=== | ||
*The diagnosis of chylothorax is with [[thoracentesis]] and analysis of the [[Pleural effusion|pleural fluid]] showing a reduced concentration of [[cholesterol]] <200mg/dl, and an elevated concentration of [[triglyceride]] >110 mg/dl. In centres with available facilities, [[lipoprotein]] analysis showing the presence of [[chylomicron]]s is the gold standard.<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref> | *The diagnosis of chylothorax is with [[thoracentesis]] and analysis of the [[Pleural effusion|pleural fluid]] showing a reduced concentration of [[cholesterol]] <200mg/dl, and an elevated concentration of [[triglyceride]] >110 mg/dl. In centres with available facilities, [[lipoprotein]] analysis showing the presence of [[chylomicron]]s is the gold standard.<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid21654988">{{cite journal| author=Kant S, Verma SK, Anand SC, Prasad R, Verma RK| title=Development of bilateral chylothorax in a younger female secondary to tuberculosis. | journal=Lung India | year= 2011 | volume= 28 | issue= 1 | pages= 56-9 | pmid=21654988 | doi=10.4103/0970-2113.76303 | pmc=3099513 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21654988 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
===History and Symptoms === | ===History and Symptoms === | ||
*Symptoms of | *Symptoms of chylothorax depends on the rate of [[chyle]] accumulation and [[etiology]]. In traumatic or surgically induced chylothorax, there is usually a [[Incubation period|latency period]] of two to ten days before symptoms become clinically evident. This is due to the restricted diet offered to critically ill or surgical patients, thereby reducing the [[Lymphatic system|lymphatic]] flow through the [[thoracic duct]]. | ||
*Symptoms may include the following<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid29316546">{{cite journal| author=Rajagopala S, Kancherla R, Ramanathan RP| title=Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature. | journal=Respiration | year= 2018 | volume= 95 | issue= 4 | pages= 260-268 | pmid=29316546 | doi=10.1159/000484694 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29316546 }} </ref><ref name="pmid31292374">{{cite journal| author=Nagano N, Suzuki M, Tamura K, Kobayashi S, Kojima Y, Naka G | display-authors=etal| title=Refractory Chylothorax and Lymphedema Caused by Advanced Gastric Cancer. | journal=Intern Med | year= 2019 | volume= 58 | issue= 21 | pages= 3143-3148 | pmid=31292374 | doi=10.2169/internalmedicine.2351-18 | pmc=6875443 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31292374 }} </ref> | |||
*[[Dyspnea]] | *[[Dyspnea]] | ||
*[[Cough]] | *[[Cough]] | ||
| Line 184: | Line 191: | ||
=== Physical Examination === | === Physical Examination === | ||
*Patients with chylothorax usually appear to be in [[Respiratory failure|respiratory distress]] | *Patients with chylothorax usually appear to be in [[Respiratory failure|respiratory distress]] | ||
*Physical examination may be remarkable for<ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | *Physical examination may be remarkable for<ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref><ref name="pmid31292374">{{cite journal| author=Nagano N, Suzuki M, Tamura K, Kobayashi S, Kojima Y, Naka G | display-authors=etal| title=Refractory Chylothorax and Lymphedema Caused by Advanced Gastric Cancer. | journal=Intern Med | year= 2019 | volume= 58 | issue= 21 | pages= 3143-3148 | pmid=31292374 | doi=10.2169/internalmedicine.2351-18 | pmc=6875443 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31292374 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
*Decreased [[breath sounds]] on the affected side | *Decreased [[breath sounds]] on the affected side | ||
*[[Tachypnea]] | |||
*[[Apnea|Apneic]] episodes | *[[Apnea|Apneic]] episodes | ||
*[[Tachycardia]] | *[[Tachycardia]] | ||
*[ | *[[Hypotension]] | ||
*[ | *Enlarged [[axillary lymph nodes]] | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
*An elevated concentration of [[Pleural effusion|pleural fluid]] [[triglyceride]] >110 mg/dL is diagnostic of chylothorax.<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref> | *An elevated concentration of [[Pleural effusion|pleural fluid]] [[triglyceride]] >110 mg/dL is diagnostic of chylothorax.<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
*A reduced concentration of [[cholesterol]] <200mg/dl is diagnostic of chylothorax.<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref> | *A reduced concentration of [[cholesterol]] <200mg/dl is diagnostic of chylothorax.<ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref> | ||
*[[Leukocyte]] cell count ˃1000, with > 90% lymphocytic predominance.<ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | *[[Leukocyte]] cell count ˃1000, with > 90% lymphocytic predominance.<ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | ||
| Line 202: | Line 209: | ||
===X-ray=== | ===X-ray=== | ||
*An [[Chest X-ray|x-ray]] may be helpful in the diagnosis of chylothorax. Findings on an [[Chest X-ray|x-ray]] suggestive | *An [[Chest X-ray|x-ray]] may be helpful in the diagnosis of chylothorax. Findings on an [[Chest X-ray|x-ray]] suggestive of chylothorax include.<ref name="pmid30402386">{{cite journal| author=Benninger LA, Ross JA, Leon ME, Reddy R| title=An unusual case of chylothorax. | journal=Respir Med Case Rep | year= 2018 | volume= 25 | issue= | pages= 318-322 | pmid=30402386 | doi=10.1016/j.rmcr.2018.10.020 | pmc=6205929 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30402386 }} </ref><ref name="pmid29316546">{{cite journal| author=Rajagopala S, Kancherla R, Ramanathan RP| title=Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature. | journal=Respiration | year= 2018 | volume= 95 | issue= 4 | pages= 260-268 | pmid=29316546 | doi=10.1159/000484694 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29316546 }} </ref><ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | ||
*[[Pleural effusion]] | *[[Pleural effusion]] | ||
*[[Pleural]] thickening | *[[Pleural]] thickening | ||
*Blunting of the [[Costophrenic angle]] | *Blunting of the [[Costophrenic angle]] | ||
[[File:Xray chylothorax.png|400px|left|thumb|X-ray showing bilateral chylothorax post [[mastectomy]] (Image B). Normal preop Xray (image A) showing [[costophrenic angle]] (yellow arrowhead), Image C shows post chylothorax management and restoration of the [[costophrenic angle]] (yellow arrow) (Picture courtesy: [https://openi.nlm.nih.gov/detailedresult?img=PMC4059869_cjc-33-06-317-g001&query=chylothorax&it=xg&req=4&npos=12 National Library of Medicine])]] | |||
<br style="clear:left"> | |||
===Ultrasound=== | ===Ultrasound=== | ||
Transthoracic [[ultrasound]] may be helpful in the diagnosis of chylothorax | Transthoracic [[ultrasound]] may be helpful in the diagnosis of chylothorax. Finding loculated fluid collection is suggestive of chylothorax. <ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref> | ||
===CT scan=== | ===CT scan=== | ||
Thoracic [[Computed tomography|CT scan]] may be helpful in the diagnosis of chylothorax. Findings on [[Computed tomography|CT scan]] suggestive of | Thoracic [[Computed tomography|CT scan]] may be helpful in the diagnosis of chylothorax.[[Computed tomography|CT scan]] is valuable in the location and treatment decision of chylothorax Findings on [[Computed tomography|CT scan]] suggestive of chylothorax include<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref> [[pleural effusion]] | ||
[[File:CT Chylothorax.gif|400px|left|thumb|Non-contrast [[computerized tomography|CT]] showing [[chyle]] collection. (Picture courtesy: [https://openi.nlm.nih.gov/detailedresult?img=PMC3904686_1749-8090-9-8-1&query=chylothorax&it=xg&req=4&npos=4 National Library of Medicine])]] | |||
<br style="clear:left"> | |||
===MRI=== | ===MRI=== | ||
*There are no MRI findings associated with chylothorax. | |||
===Other Imaging Findings=== | ===Other Imaging Findings=== | ||
Other diagnostic studies for chylothorax include | Other diagnostic studies for chylothorax include | ||
*[[Lymphangiography]] with [[Lipiodol]] ([[ethiodized oil]]) <ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref> which demonstrates the site of extravasation into the [[pleural cavity]]. | *[[Lymphangiography]] with [[Lipiodol]] ([[ethiodized oil]]) <ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref> which demonstrates the site of extravasation into the [[pleural cavity]]. | ||
*lymphoscintigraphy; identify [[chyle]] leakage but not the exact site.<ref name="pmid29106894">{{cite journal| author=Nicastri DG, Flores RM| title=Chylothorax: Abdominal approach. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 814 | pmid=29106894 | doi=10.1016/j.jtcvs.2017.09.111 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29106894 }} </ref><ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref><ref name="pmid29438003">{{cite journal| author=Turpin S, Lambert R| title=Lymphoscintigraphy of Chylous Anomalies: Chylothorax, Chyloperitoneum, Chyluria, and Lymphangiomatosis-15-Year Experience in a Pediatric Setting and Review of the Literature. | journal=J Nucl Med Technol | year= 2018 | volume= 46 | issue= 2 | pages= 123-128 | pmid=29438003 | doi=10.2967/jnmt.117.203281 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29438003 }} </ref> | *lymphoscintigraphy; identify [[chyle]] leakage but not the exact site.<ref name="pmid29106894">{{cite journal| author=Nicastri DG, Flores RM| title=Chylothorax: Abdominal approach. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 814 | pmid=29106894 | doi=10.1016/j.jtcvs.2017.09.111 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29106894 }} </ref><ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref><ref name="pmid29438003">{{cite journal| author=Turpin S, Lambert R| title=Lymphoscintigraphy of Chylous Anomalies: Chylothorax, Chyloperitoneum, Chyluria, and Lymphangiomatosis-15-Year Experience in a Pediatric Setting and Review of the Literature. | journal=J Nucl Med Technol | year= 2018 | volume= 46 | issue= 2 | pages= 123-128 | pmid=29438003 | doi=10.2967/jnmt.117.203281 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29438003 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
| Line 227: | Line 239: | ||
=== Medical Therapy === | === Medical Therapy === | ||
Chylothorax is a medical emergency and requires prompt treatment. | Chylothorax is a medical emergency and requires prompt treatment. | ||
Medical therapy for chylothorax include<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref> Conservative therapy aims at minimizing [[Lymphatic system|lymph flow]] through the damaged [[thoracic duct]].<ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref><ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref><ref name=" | Medical therapy for chylothorax include<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref><ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref> Conservative therapy aims at minimizing [[Lymphatic system|lymph flow]] through the damaged [[thoracic duct]].<ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref><ref name="pmid29703801">{{cite journal| author=Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY| title=Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients. | journal=Pediatrics | year= 2018 | volume= 141 | issue= 5 | pages= | pmid=29703801 | doi=10.1542/peds.2016-3309 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29703801 }} </ref><ref name="pmid19882503">{{cite journal| author=Waterfield T, Lakhoo K| title=Challenges in the management of refractory bilateral idiopathic congenital chylothoraces in a newborn. | journal=Eur J Pediatr Surg | year= 2010 | volume= 20 | issue= 3 | pages= 198-201 | pmid=19882503 | doi=10.1055/s-0029-1241874 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19882503 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref> | ||
*[[Total parenteral nutrition]] | *[[Total parenteral nutrition]] with oral fasting | ||
*Oral low-fat medium-chain [[triglyceride]] | *Oral low-fat medium-chain [[triglyceride]] | ||
*[[Octreotide injection]]s | *[[Octreotide injection]]s | ||
*Treatment of the underlying condition | *Treatment of the underlying condition | ||
**[[Sarcoidosis]] with [[steroid]]s | **[[Sarcoidosis]] with [[steroid]]s | ||
**[[Tuberculosis]] with [[Tuberculosis medical therapy|RIPE]] | |||
**[[Congestive heart failure]] with [[diuretic]]s | **[[Congestive heart failure]] with [[diuretic]]s | ||
*Intravenous [[etilefrine]] | *Intravenous [[etilefrine]] | ||
=== Surgery === | === Surgery === | ||
Surgery is the mainstay of therapy for chylothorax. Surgery is recommended where despite conservative management, patient drains more than 1.5 l/day in an adult or >100 ml/kg body weight per day in a child, leaks [[chyle]] at >1 l/day× 5 days or has persistent [[chyle]] flow for >2 weeks. It is also recommended if there is a rapid decline in nutritional status despite conservative management.<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref> <ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid29249497">{{cite journal| author=Lo Rito M, Al-Radi OO, Saedi A, Kotani Y, Ben Sivarajan V, Russell JL | display-authors=etal| title=Chylothorax and pleural effusion in contemporary extracardiac fenestrated fontan completion. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 5 | pages= 2069-2077 | pmid=29249497 | doi=10.1016/j.jtcvs.2017.11.046 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29249497 }} </ref><ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref><ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref><ref name="pmid17251600">{{cite journal| author=Townshend AP, Speake W, Brooks A| title=Chylothorax. | journal=Emerg Med J | year= 2007 | volume= 24 | issue= 2 | pages= e11 | pmid=17251600 | doi=10.1136/emj.2006.042028 | pmc=2658219 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17251600 }} </ref> | Surgery is the mainstay of therapy for chylothorax. Surgery is recommended where despite conservative management, patient drains more than 1.5 l/day in an adult or >100 ml/kg body weight per day in a child, leaks [[chyle]] at >1 l/day× 5 days or has persistent [[chyle]] flow for >2 weeks. It is also recommended if there is a rapid decline in nutritional status despite conservative management.<ref name="pmid30474568">{{cite journal| author=Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S| title=Chylothorax after hepatectomy: a case report. | journal=J Med Case Rep | year= 2018 | volume= 12 | issue= 1 | pages= 347 | pmid=30474568 | doi=10.1186/s13256-018-1882-x | pmc=6260677 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30474568 }} </ref> <ref name="pmid19766473">{{cite journal| author=McGrath EE, Blades Z, Anderson PB| title=Chylothorax: aetiology, diagnosis and therapeutic options. | journal=Respir Med | year= 2010 | volume= 104 | issue= 1 | pages= 1-8 | pmid=19766473 | doi=10.1016/j.rmed.2009.08.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19766473 }} </ref><ref name="pmid17273624">{{cite journal| author=Vaz MA, Fernandes PP| title=[Chylothorax]. | journal=J Bras Pneumol | year= 2006 | volume= 32 Suppl 4 | issue= | pages= S197-203 | pmid=17273624 | doi=10.1590/s1806-37132006000900006 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17273624 }} </ref><ref name="pmid29249497">{{cite journal| author=Lo Rito M, Al-Radi OO, Saedi A, Kotani Y, Ben Sivarajan V, Russell JL | display-authors=etal| title=Chylothorax and pleural effusion in contemporary extracardiac fenestrated fontan completion. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 5 | pages= 2069-2077 | pmid=29249497 | doi=10.1016/j.jtcvs.2017.11.046 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29249497 }} </ref><ref name="pmid28494978">{{cite journal| author=Savla JJ, Itkin M, Rossano JW, Dori Y| title=Post-Operative Chylothorax in Patients With Congenital Heart Disease. | journal=J Am Coll Cardiol | year= 2017 | volume= 69 | issue= 19 | pages= 2410-2422 | pmid=28494978 | doi=10.1016/j.jacc.2017.03.021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28494978 }} </ref><ref name="pmid25829744">{{cite journal| author=Das J, Thambudorai R, Ray S| title=Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax. | journal=Indian J Nucl Med | year= 2015 | volume= 30 | issue= 2 | pages= 177-9 | pmid=25829744 | doi=10.4103/0972-3919.152988 | pmc=4379685 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25829744 }} </ref><ref name="pmid17251600">{{cite journal| author=Townshend AP, Speake W, Brooks A| title=Chylothorax. | journal=Emerg Med J | year= 2007 | volume= 24 | issue= 2 | pages= e11 | pmid=17251600 | doi=10.1136/emj.2006.042028 | pmc=2658219 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17251600 }} </ref><ref name="pmid19882503">{{cite journal| author=Waterfield T, Lakhoo K| title=Challenges in the management of refractory bilateral idiopathic congenital chylothoraces in a newborn. | journal=Eur J Pediatr Surg | year= 2010 | volume= 20 | issue= 3 | pages= 198-201 | pmid=19882503 | doi=10.1055/s-0029-1241874 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19882503 }} </ref><ref name="pmid31341753">{{cite journal| author=Jacob S, Meneses A, Landolfo K, El-Sayed Ahmed M, Makey IA, Pham SM | display-authors=etal| title=Incidence, Management, and Outcomes of Chylothorax after Lung Transplantation: A Single-center Experience. | journal=Cureus | year= 2019 | volume= 11 | issue= 7 | pages= e5190 | pmid=31341753 | doi=10.7759/cureus.5190 | pmc=6649881 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31341753 }} </ref><ref name="pmid29129424">{{cite journal| author=Diaz-Gutierrez I, Rao MV, Andrade RS| title=Laparoscopic ligation of cisterna chyli for refractory chylothorax: A case series and review of the literature. | journal=J Thorac Cardiovasc Surg | year= 2018 | volume= 155 | issue= 2 | pages= 815-819 | pmid=29129424 | doi=10.1016/j.jtcvs.2017.08.140 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29129424 }} </ref> | ||
*[[Thoracentesis]] | *[[Thoracentesis]] | ||
*[[Chest tube|Tube thoracostomy]] | *[[Chest tube|Tube thoracostomy]] | ||
| Line 249: | Line 262: | ||
*pleuroperitoneal shunt | *pleuroperitoneal shunt | ||
*[[Thoracic duct]] ligation | *[[Thoracic duct]] ligation | ||
*Ligation of [[cisterna chyli]] | |||
*Lymphatic [[Therapeutic embolization|embolization]] | *Lymphatic [[Therapeutic embolization|embolization]] | ||
Latest revision as of 02:02, 31 July 2020
| Chylothorax | |
| ICD-10 | I89.8, J91 |
|---|---|
| ICD-9 | 457.8, 511.9 |
| DiseasesDB | 29612 |
| eMedicine | med/381 |
| MeSH | D002916 |
|
WikiDoc Resources for Chylothorax |
|
Articles |
|---|
|
Most recent articles on Chylothorax Most cited articles on Chylothorax |
|
Media |
|
Powerpoint slides on Chylothorax |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Chylothorax at Clinical Trials.gov Clinical Trials on Chylothorax at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Chylothorax
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Chylothorax Discussion groups on Chylothorax Patient Handouts on Chylothorax Directions to Hospitals Treating Chylothorax Risk calculators and risk factors for Chylothorax
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Chylothorax |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor: Joanna Ekabua, M.D. [2]
Synonyms and keywords: Chylothorax
Overview
Chylothorax, a type of pleural effusion is the accumulation of chyle in the pleural cavity secondary to destruction or obstruction of the thoracic duct or its tributaries. Depending on the etiology, chylothorax could be exudative ( tuberculosis) or transudative (svc obstruction). It is an uncommon but established complication of thoracic surgery. Chylothorax is most commonly right-sided (50%) because of the anatomic location of the thoracic duct, left-sided (33.3%), or bilateral (16.66%). Thoracic duct damage above the fifth thoracic vertebra results in a left-sided chylothorax whereas damage to the thoracic duct below fifth thoracic vertebra leads to a right-sided effusion. Some common symptoms of chylothorax include dyspnea, cough, and severe chest pain. Some physical exams finding include decreased breath sounds and dullness to percussion depending on the size and location of fluid. The definitive diagnosis of chylothorax is with thoracentesis and analysis of the pleural fluid showing a reduced concentration of cholesterol <200mg/dl, and an elevated concentration of triglyceride >110 mg/dl. Management of chylothorax may be conservative or surgical. Conservative management include total parenteral nutrition, oral low-fat medium-chain triglyceride, and octreotide injections. Surgical management include tube thoracostomy, pleurodesis, pleurectomy, pleuroperitoneal shunt, and thoracic duct ligation.
Historical Perspective
- Chylothorax was first described in 1633 by Bartolet, and Quincke reported the first case in 1875. [1]
- In 1917, Brandt was the first to discover the association between tuberculosis and the development of chylothorax. [1]
Classification
Chylothorax may be classified as[2][3]
- Non-traumatic
- Malignacy
- Idopathic
- Disease
- Sarcoidosis
- Haemangiomatosis
- Tuberculosis
- Heart failure
- Benign tumor
- Amyloidosis
- Lymphangioleiomyomatosis
- Filariasis
- Transdiaphrgmatic movement of chylous ascitic fluid
- SVC obstruction
- Traumatic
- Iatrogenic
- Non-iatrogenic
- Knife injury
- Childbirth
- Forceful cough or emesis
- Blunt trauma to the thorax
- Bullet wound
| Chylothorax | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Non-traumatic | Traumatic | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Malignancy | Diseases | Idopathic | Non- Iatrogenic | Iatrogenic | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| - Sarcoidosis
- Haemangiomatosis - Tuberculosis - Heart failure -Benign tumor - Amyloidosis -Lymphangiolei -omyomatosis - Filariasis - Transdiaphrgmatic movement of chylous ascitic fluid - SVC obstruction | - Knife injury
- Childbirth - Forceful cough or emesis - Blunt trauma to the thorax - Bullet wound | - Radiation
- Thoracic surgery - Head and neck surgery | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Pathophysiology
- It is thought that chylothorax is the result of obstruction, difficulty in drainage of lymph, lymphatic malformation or laceration of the thoracic duct leading to leakage of chyle into the pleural cavity.[4]
- Chylothorax as a result of tuberculosis is thought to be produced by the enlargement of the lumbar and the iliac lymph nodes producing obstruction of the cisterna chyli and thoracic duct. This leads to dilatation of the lumbar channels, followed by the opening of collateral anastomosis. With the many lymphaticovenous anastomosis existing between the thoracic duct, and the azygos, intercostal, and Lumbar veins. The increased pressure in the system results in the transudation of chyle into the pleural cavity.[1]
Causes
- Common causes of chylothorax include[1][2][3][4][5][6][7]
- Congenital
- Malignacy
- Sarcoidosis
- Tuberculosis
- Cirrhosis
- Heart failure
- Benign tumor
- SVC obstruction
- Thoracic surgery
- Knife injury
- Bullet wound
- Blunt trauma to the thorax
- Head and neck surgery
- Transdiaphrgmatic movement of chylous ascitic fluid
Differentiating chylothorax from other Diseasess
Chylothorax must be differentiated from[3] [8] [9][4]
- Empyema
- Pseudochylothorax
- Cholesterol pleural effusions
- Tuberculosis
- Chronic pneumothorax
- Rheumatoid pleurisy
- Chronic hemothorax
- Cirrhosis
- Nephrotic syndrome
- Lymphoma
- Congestive heart failure
- Constrictive pericarditis
Epidemiology and Demographics
- The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide.
- In 2011, the incidence of pediatric chylothorax was estimated to be 3.7%[10] [11]
- Incidence post cardiothoracic surgeries are between 0.9% and 6.6%.
- Incidence post congenital cardiac anomalies repair is 2.8%.
- Incidence post esophageal surgeries range from 0.2% to 10%.
Age
Gender
- Chylothorax affects men and women equally.
Race
- There is no racial predilection for chylothorax.
Risk Factors
Common risk factors in the development of Chylothorax] are[2][3][12][13][10][14][15][16][17][5][18][19]
- Surgery
- Hepatectomy
- Esophagectomy
- Lung surgery
- Cardiac surgery
- Fontan procedure
- Retroperitoneal surgery around the cisterna chyli, example AAA repair
- Dasatinib therapy
- Rib fracture
- Tuberculosis
- Gastric cancer
- Malignant pleural mesothelioma
- Malignant lymphoproliferative disorders
Screening
- There is insufficient evidence to recommend routine screening for chylothorax.
Natural History, Complications and Prognosis
- If left untreated, 100% of patients with chylothorax may progress to develop[3][20]
- Hypovolaemia
- Hypoalbuminemia
- Malnutrition; as a result of protein, fats and vitamins loss with weight loss and muscle wasting.
- Hyponatremia and hypocalcemia due to electrolyte loss.
- Opportunistic infections as a result of immunoglobulins loss.
- Subtherapeutic effects of medications like digoxin and amiodarone as they are lost through the leaking chyle.
- Common complications of chylothorax include malnutrition, immunosuppression and respiratory distress.[3][4]
- Prognosis is generally good and the mortality rate from chylothorax has considerably improved from approximately 50% as described in 1948. This is due to the more aggressive management plans implemented. Currently, the worst prognosis is seen in malignant and bilateral chylothoraces.[3][4][14]
Diagnosis
Diagnostic Study of Choice
- The diagnosis of chylothorax is with thoracentesis and analysis of the pleural fluid showing a reduced concentration of cholesterol <200mg/dl, and an elevated concentration of triglyceride >110 mg/dl. In centres with available facilities, lipoprotein analysis showing the presence of chylomicrons is the gold standard.[2][3][16][1][4]
History and Symptoms
- Symptoms of chylothorax depends on the rate of chyle accumulation and etiology. In traumatic or surgically induced chylothorax, there is usually a latency period of two to ten days before symptoms become clinically evident. This is due to the restricted diet offered to critically ill or surgical patients, thereby reducing the lymphatic flow through the thoracic duct.
- Symptoms may include the following[2][3][5][19]
- Dyspnea
- Cough
- Pleuritic chest pain
- Fever
- Swelling in the supraclavicular fossa
- Weight loss
- Muscle wasting
- Immunodeficiency
- Malnutrition
Physical Examination
- Patients with chylothorax usually appear to be in respiratory distress
- Physical examination may be remarkable for[16][11][19][4]
- Decreased breath sounds on the affected side
- Tachypnea
- Apneic episodes
- Tachycardia
- Hypotension
- Enlarged axillary lymph nodes
Laboratory Findings
- An elevated concentration of pleural fluid triglyceride >110 mg/dL is diagnostic of chylothorax.[2][3][16][4]
- A reduced concentration of cholesterol <200mg/dl is diagnostic of chylothorax.[3]
- Leukocyte cell count ˃1000, with > 90% lymphocytic predominance.[11]
- Hypoalbuminemia[1]
Electrocardiogram
- There are no ECG findings associated with chylothorax.
X-ray
- An x-ray may be helpful in the diagnosis of chylothorax. Findings on an x-ray suggestive of chylothorax include.[16][5][11]
- Pleural effusion
- Pleural thickening
- Blunting of the Costophrenic angle
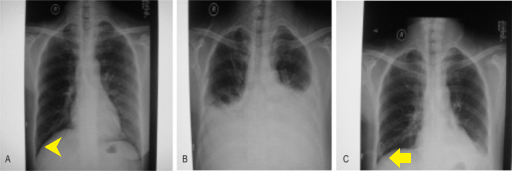
Ultrasound
Transthoracic ultrasound may be helpful in the diagnosis of chylothorax. Finding loculated fluid collection is suggestive of chylothorax. [11]
CT scan
Thoracic CT scan may be helpful in the diagnosis of chylothorax.CT scan is valuable in the location and treatment decision of chylothorax Findings on CT scan suggestive of chylothorax include[2] pleural effusion

MRI
- There are no MRI findings associated with chylothorax.
Other Imaging Findings
Other diagnostic studies for chylothorax include
- Lymphangiography with Lipiodol (ethiodized oil) [2] which demonstrates the site of extravasation into the pleural cavity.
- lymphoscintigraphy; identify chyle leakage but not the exact site.[14][20][21][4]
Other Diagnostic Studies
- There are no other diagnostic studies associated with chylothorax.
Treatment
Medical Therapy
Chylothorax is a medical emergency and requires prompt treatment. Medical therapy for chylothorax include[2][3][10] Conservative therapy aims at minimizing lymph flow through the damaged thoracic duct.[20][11][6][4]
- Total parenteral nutrition with oral fasting
- Oral low-fat medium-chain triglyceride
- Octreotide injections
- Treatment of the underlying condition
- Sarcoidosis with steroids
- Tuberculosis with RIPE
- Congestive heart failure with diuretics
- Intravenous etilefrine
Surgery
Surgery is the mainstay of therapy for chylothorax. Surgery is recommended where despite conservative management, patient drains more than 1.5 l/day in an adult or >100 ml/kg body weight per day in a child, leaks chyle at >1 l/day× 5 days or has persistent chyle flow for >2 weeks. It is also recommended if there is a rapid decline in nutritional status despite conservative management.[2] [3][4][12][10][20][15][6][18][22]
- Thoracentesis
- Tube thoracostomy
- Thoracoscopy
- Pleurodesis with
- Pleurectomy
- pleuroperitoneal shunt
- Thoracic duct ligation
- Ligation of cisterna chyli
- Lymphatic embolization
Primary Prevention
- There are no established measures for the primary prevention of chylothorax.
Secondary Prevention
- There are no established measures for the secondary prevention of chylothorax.
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Kant S, Verma SK, Anand SC, Prasad R, Verma RK (2011). "Development of bilateral chylothorax in a younger female secondary to tuberculosis". Lung India. 28 (1): 56–9. doi:10.4103/0970-2113.76303. PMC 3099513. PMID 21654988.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Yamamoto R, Mokuno Y, Matsubara H, Kaneko H, Sato Y, Iyomasa S (2018). "Chylothorax after hepatectomy: a case report". J Med Case Rep. 12 (1): 347. doi:10.1186/s13256-018-1882-x. PMC 6260677. PMID 30474568.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 McGrath EE, Blades Z, Anderson PB (2010). "Chylothorax: aetiology, diagnosis and therapeutic options". Respir Med. 104 (1): 1–8. doi:10.1016/j.rmed.2009.08.010. PMID 19766473.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Vaz MA, Fernandes PP (2006). "[Chylothorax]". J Bras Pneumol. 32 Suppl 4: S197–203. doi:10.1590/s1806-37132006000900006. PMID 17273624.
- ↑ 5.0 5.1 5.2 5.3 Rajagopala S, Kancherla R, Ramanathan RP (2018). "Tuberculosis-Associated Chylothorax: Case Report and Systematic Review of the Literature". Respiration. 95 (4): 260–268. doi:10.1159/000484694. PMID 29316546.
- ↑ 6.0 6.1 6.2 Waterfield T, Lakhoo K (2010). "Challenges in the management of refractory bilateral idiopathic congenital chylothoraces in a newborn". Eur J Pediatr Surg. 20 (3): 198–201. doi:10.1055/s-0029-1241874. PMID 19882503.
- ↑ Austin A, Al-Faris F, Modi A, Chopra A (2019). "A transudative chylothorax associated with superior vena cava syndrome". Respir Med Case Rep. 28: 100898. doi:10.1016/j.rmcr.2019.100898. PMC 6626116 Check
|pmc=value (help). PMID 31338288. - ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ 10.0 10.1 10.2 10.3 10.4 Savla JJ, Itkin M, Rossano JW, Dori Y (2017). "Post-Operative Chylothorax in Patients With Congenital Heart Disease". J Am Coll Cardiol. 69 (19): 2410–2422. doi:10.1016/j.jacc.2017.03.021. PMID 28494978.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Muniz G, Hidalgo-Campos J, Valdivia-Tapia MDC, Shaikh N, Carreazo NY (2018). "Successful Management of Chylothorax With Etilefrine: Case Report in 2 Pediatric Patients". Pediatrics. 141 (5). doi:10.1542/peds.2016-3309. PMID 29703801.
- ↑ 12.0 12.1 Lo Rito M, Al-Radi OO, Saedi A, Kotani Y, Ben Sivarajan V, Russell JL; et al. (2018). "Chylothorax and pleural effusion in contemporary extracardiac fenestrated fontan completion". J Thorac Cardiovasc Surg. 155 (5): 2069–2077. doi:10.1016/j.jtcvs.2017.11.046. PMID 29249497.
- ↑ Sasaki H, Kimizuka Y, Ogata H, Okada Y, Ota S, Sano T; et al. (2019). "Successful Control of Dasatinib-related Chylothorax by the Japanese Herbal Medicine "Goreisan"". Intern Med. 58 (21): 3139–3141. doi:10.2169/internalmedicine.3002-19. PMC 6875454 Check
|pmc=value (help). PMID 31292394. - ↑ 14.0 14.1 14.2 Nicastri DG, Flores RM (2018). "Chylothorax: Abdominal approach". J Thorac Cardiovasc Surg. 155 (2): 814. doi:10.1016/j.jtcvs.2017.09.111. PMID 29106894.
- ↑ 15.0 15.1 Townshend AP, Speake W, Brooks A (2007). "Chylothorax". Emerg Med J. 24 (2): e11. doi:10.1136/emj.2006.042028. PMC 2658219. PMID 17251600.
- ↑ 16.0 16.1 16.2 16.3 16.4 Benninger LA, Ross JA, Leon ME, Reddy R (2018). "An unusual case of chylothorax". Respir Med Case Rep. 25: 318–322. doi:10.1016/j.rmcr.2018.10.020. PMC 6205929. PMID 30402386.
- ↑ Pospiskova J, Smolej L, Belada D, Simkovic M, Motyckova M, Sykorova A; et al. (2019). "Experiences in the treatment of refractory chylothorax associated with lymphoproliferative disorders". Orphanet J Rare Dis. 14 (1): 9. doi:10.1186/s13023-018-0991-3. PMC 6327395. PMID 30626415.
- ↑ 18.0 18.1 Jacob S, Meneses A, Landolfo K, El-Sayed Ahmed M, Makey IA, Pham SM; et al. (2019). "Incidence, Management, and Outcomes of Chylothorax after Lung Transplantation: A Single-center Experience". Cureus. 11 (7): e5190. doi:10.7759/cureus.5190. PMC 6649881 Check
|pmc=value (help). PMID 31341753. - ↑ 19.0 19.1 19.2 Nagano N, Suzuki M, Tamura K, Kobayashi S, Kojima Y, Naka G; et al. (2019). "Refractory Chylothorax and Lymphedema Caused by Advanced Gastric Cancer". Intern Med. 58 (21): 3143–3148. doi:10.2169/internalmedicine.2351-18. PMC 6875443 Check
|pmc=value (help). PMID 31292374. - ↑ 20.0 20.1 20.2 20.3 Das J, Thambudorai R, Ray S (2015). "Lymphoscintigraphy combined with single-photon emission computed tomography-computed tomography (SPECT-CT): A very effective imaging approach for identification of the site of leak in postoperative chylothorax". Indian J Nucl Med. 30 (2): 177–9. doi:10.4103/0972-3919.152988. PMC 4379685. PMID 25829744.
- ↑ Turpin S, Lambert R (2018). "Lymphoscintigraphy of Chylous Anomalies: Chylothorax, Chyloperitoneum, Chyluria, and Lymphangiomatosis-15-Year Experience in a Pediatric Setting and Review of the Literature". J Nucl Med Technol. 46 (2): 123–128. doi:10.2967/jnmt.117.203281. PMID 29438003.
- ↑ Diaz-Gutierrez I, Rao MV, Andrade RS (2018). "Laparoscopic ligation of cisterna chyli for refractory chylothorax: A case series and review of the literature". J Thorac Cardiovasc Surg. 155 (2): 815–819. doi:10.1016/j.jtcvs.2017.08.140. PMID 29129424.