COVID-19-associated pneumonia: Difference between revisions
(English edits) |
|||
| (21 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{COVID-19}} | {{Main article|COVID-19}} | ||
{{SI}} | |||
'''For COVID-19 frequently asked inpatient questions, click [[COVID-19 frequently asked inpatient questions|here]]'''<br> | |||
'''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]'''<br>'''For COVID-19 patient information, click [[COVID-19 (patient information)|here]]''' | |||
{{CMG}}; {{AE}} {{Usman Ali Akbar}} | {{CMG}}; {{AE}} {{Usman Ali Akbar}} | ||
{{SK}}2019 novel coronavirus disease, COVID19,Wuhan virus, L type COVID pneumonia, H type Pneumonia | {{SK}}2019 novel coronavirus disease, COVID19, Wuhan virus, L type COVID pneumonia, H type Pneumonia | ||
==Overview== | ==Overview== | ||
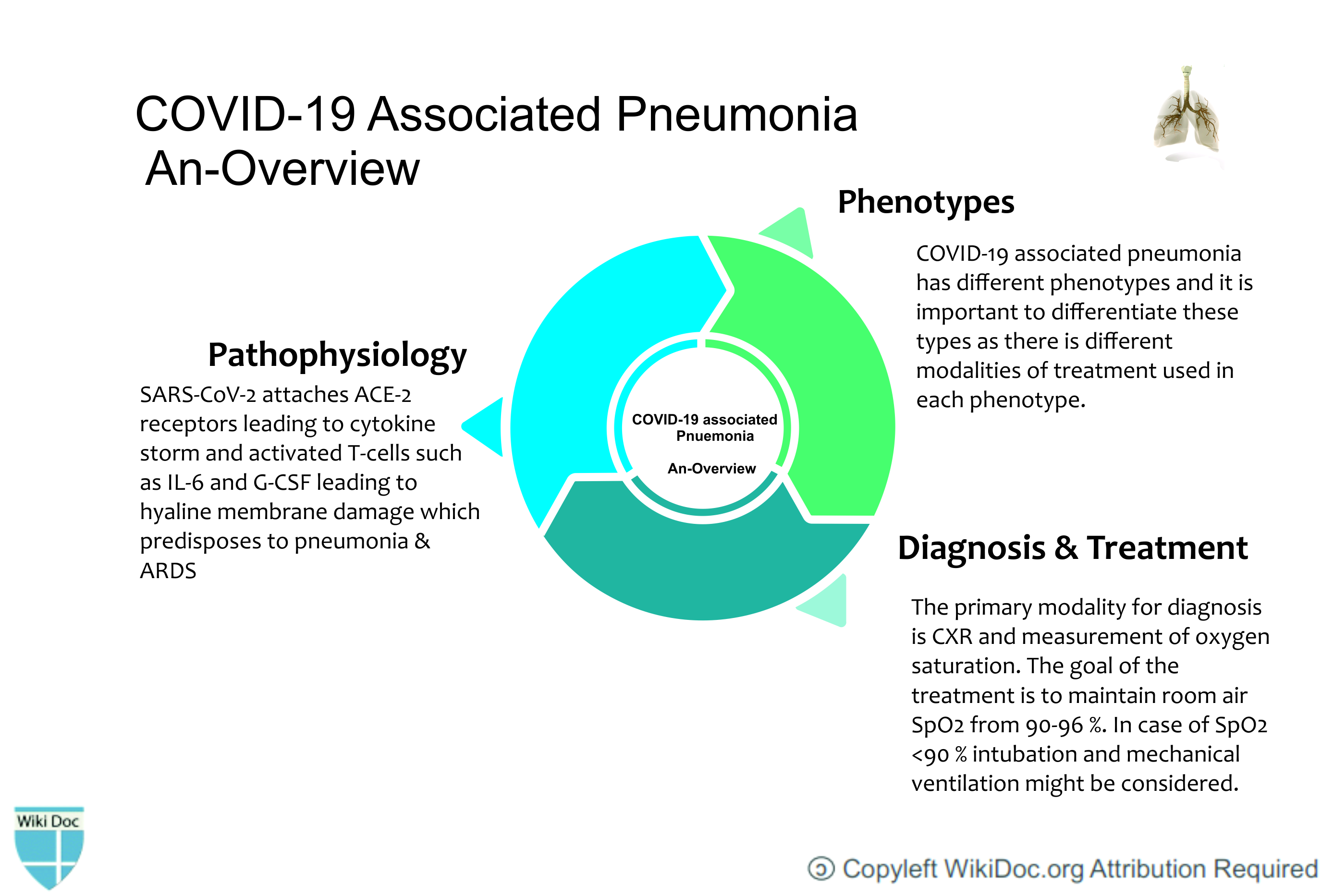
In December 2019, a novel coronavirus was detected in [[pneumonia]] patients in the Chinese city of Wuhan. The novel coronavirus was later named as [[2019-nCoV|2019-nCoV.]] Since it was identified, [[pneumonia]] appears to be the most frequent manifestation of infection. Despite mimicking the symptoms and criteria of Berlin's definition of [[Acute respiratory distress syndrome|ARDS]], COVID-19 pneumonia is a distinct disease with features including severe [[hypoxemia]] often associated with the normal or near-normal respiratory system [[compliance]]. | |||
[[File:Overview-pneumonia.jpg|600px|center]] | |||
==Historical Perspective== | ==Historical Perspective== | ||
| Line 61: | Line 66: | ||
* Vasoplegia results which further accounts for severe [[Hypoxemia|hypoxemia.]] | * Vasoplegia results which further accounts for severe [[Hypoxemia|hypoxemia.]] | ||
[[File: | [[File:COVID-pneumonia-wikidoc.jpg|600px|center]] | ||
==Differentiating COVID-19-associated pneumonia from other Diseases== | ==Differentiating COVID-19-associated pneumonia from other Diseases== | ||
*For further information on COVID-19-associated pneumonia [[COVID-19-associated pneumonia differential diagnosis|click here]]. | |||
*To view the COVID-19 differential diagnosis [[COVID-19-associated differential diagnosis|click here]]. | |||
* | |||
| | |||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Incidence/Prevalence of COVID-19 Associated Pneumonia | |+Incidence/Prevalence of COVID-19 Associated Pneumonia | ||
!Date Published | !style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Date Published}} | ||
!Author | !style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Author}} | ||
!Country | !style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Country}} | ||
!Total Number Of Patients | !style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Total Number Of Patients}} | ||
!Incidence/Prevalence | !style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Incidence/Prevalence}} | ||
|- | |- | ||
|01 June,2020 | |01 June,2020 | ||
| Line 151: | Line 98: | ||
|3600 | |3600 | ||
|73.2 % | |73.2 % | ||
|} | |} | ||
=== Age === | === Age === | ||
*In another study it was reported that the mean age of the [[population]] was 45 years, and 307 (79%) of 391 cases were adults aged 30–69 years. At the time of the first clinical assessment, most cases were mild (102 [26%] of 391) or moderate (254 [65%] of 391), and only 35 (9%) were severe.<ref name="Bi Wu Mei Ye 2020 p. ">{{cite journal | last=Bi | first=Qifang | last2=Wu | first2=Yongsheng | last3=Mei | first3=Shujiang | last4=Ye | first4=Chenfei | last5=Zou | first5=Xuan | last6=Zhang | first6=Zhen | last7=Liu | first7=Xiaojian | last8=Wei | first8=Lan | last9=Truelove | first9=Shaun A | last10=Zhang | first10=Tong | last11=Gao | first11=Wei | last12=Cheng | first12=Cong | last13=Tang | first13=Xiujuan | last14=Wu | first14=Xiaoliang | last15=Wu | first15=Yu | last16=Sun | first16=Binbin | last17=Huang | first17=Suli | last18=Sun | first18=Yu | last19=Zhang | first19=Juncen | last20=Ma | first20=Ting | last21=Lessler | first21=Justin | last22=Feng | first22=Tiejian | title=Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study | journal=The Lancet Infectious Diseases | publisher=Elsevier BV | year=2020 | issn=1473-3099 | doi=10.1016/s1473-3099(20)30287-5 | page=}}</ref> | *In another study it was reported that the mean age of the [[population]] was 45 years, and 307 (79%) of 391 cases were adults aged 30–69 years. | ||
*At the time of the first clinical assessment, most cases were mild (102 [26%] of 391) or moderate (254 [65%] of 391), and only 35 (9%) were severe.<ref name="Bi Wu Mei Ye 2020 p.">{{cite journal | last=Bi | first=Qifang | last2=Wu | first2=Yongsheng | last3=Mei | first3=Shujiang | last4=Ye | first4=Chenfei | last5=Zou | first5=Xuan | last6=Zhang | first6=Zhen | last7=Liu | first7=Xiaojian | last8=Wei | first8=Lan | last9=Truelove | first9=Shaun A | last10=Zhang | first10=Tong | last11=Gao | first11=Wei | last12=Cheng | first12=Cong | last13=Tang | first13=Xiujuan | last14=Wu | first14=Xiaoliang | last15=Wu | first15=Yu | last16=Sun | first16=Binbin | last17=Huang | first17=Suli | last18=Sun | first18=Yu | last19=Zhang | first19=Juncen | last20=Ma | first20=Ting | last21=Lessler | first21=Justin | last22=Feng | first22=Tiejian | title=Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study | journal=The Lancet Infectious Diseases | publisher=Elsevier BV | year=2020 | issn=1473-3099 | doi=10.1016/s1473-3099(20)30287-5 | page=}}</ref> | |||
=== Gender === | === Gender === | ||
| Line 163: | Line 111: | ||
=== Race === | === Race === | ||
*There is no significant data reporting specific race predilection for the patients developing COVID-19 associated pneumonia | *There is no significant data reporting specific race predilection for the patients developing COVID-19 associated pneumonia. | ||
==Risk Factors== | ==Risk Factors== | ||
| Line 177: | Line 125: | ||
==Screening== | ==Screening== | ||
* There is | * There is insufficient evidence to recommend routine screening for COVID-19 associated pneumonia. | ||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
| Line 185: | Line 133: | ||
* This is based on experimental observation by Barach and Mascheroni. This has been termed as patient self-inflicted lung injury. Over time the increased [[edema]] causes lung weight to increase. | * This is based on experimental observation by Barach and Mascheroni. This has been termed as patient self-inflicted lung injury. Over time the increased [[edema]] causes lung weight to increase. | ||
* There is superimposed pressure and dependent [[atelectasis]] that develops over the progression of time. | * There is superimposed pressure and dependent [[atelectasis]] that develops over the progression of time. | ||
* When the lung [[edema]] increases massively, the lung's gas volume decreases and then [[Tidal volume|tidal volumes]] that | * When the lung [[edema]] increases massively, the lung's gas volume decreases and then [[Tidal volume|tidal volumes]] that are usually generated for a given pressure also decreases. | ||
* This leads to the development of [[dyspnea]] and worsening of the patient's self-inflicted lung injury.<ref name="Robba Battaglini Ball Patroniti 2020 p=103455">{{cite journal | last=Robba | first=Chiara | last2=Battaglini | first2=Denise | last3=Ball | first3=Lorenzo | last4=Patroniti | first4=Nicolo’ | last5=Loconte | first5=Maurizio | last6=Brunetti | first6=Iole | last7=Vena | first7=Antonio | last8=Giacobbe | first8=Daniele Roberto | last9=Bassetti | first9=Matteo | last10=Rocco | first10=Patricia Rieken Macedo | last11=Pelosi | first11=Paolo | title=Distinct phenotypes require distinct respiratory management strategies in severe COVID-19 | journal=Respiratory Physiology & Neurobiology | publisher=Elsevier BV | volume=279 | year=2020 | issn=1569-9048 | doi=10.1016/j.resp.2020.103455 | page=103455}}</ref> | * This leads to the development of [[dyspnea]] and worsening of the patient's self-inflicted lung injury.<ref name="Robba Battaglini Ball Patroniti 2020 p=103455">{{cite journal | last=Robba | first=Chiara | last2=Battaglini | first2=Denise | last3=Ball | first3=Lorenzo | last4=Patroniti | first4=Nicolo’ | last5=Loconte | first5=Maurizio | last6=Brunetti | first6=Iole | last7=Vena | first7=Antonio | last8=Giacobbe | first8=Daniele Roberto | last9=Bassetti | first9=Matteo | last10=Rocco | first10=Patricia Rieken Macedo | last11=Pelosi | first11=Paolo | title=Distinct phenotypes require distinct respiratory management strategies in severe COVID-19 | journal=Respiratory Physiology & Neurobiology | publisher=Elsevier BV | volume=279 | year=2020 | issn=1569-9048 | doi=10.1016/j.resp.2020.103455 | page=103455}}</ref> | ||
| Line 206: | Line 154: | ||
* There is no established criteria for the [[diagnosis]] of COVID-19 associated pneumonia. | * There is no established criteria for the [[diagnosis]] of COVID-19 associated pneumonia. | ||
* Initial [[Chest X-ray|chest x-rays]] maybe normal. | * Initial [[Chest X-ray|chest x-rays]] maybe normal. | ||
* CT-scan chest is more sensitive than chest x-ray but there | * CT-scan chest is more sensitive than chest x-ray but there are no set criteria to diagnose COVID-19 associated [[pneumonia]] in COVID-19 patients. | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
| Line 294: | Line 242: | ||
* Bilateral and/or multilobar involvement is common. | * Bilateral and/or multilobar involvement is common. | ||
* CXR typically shows patchy or diffuse asymmetric airspace opacities which is also seen in other [[coronaviruses]] cases.<ref name="Chen Yang Yang Wang 2020 pp. 764–766">{{cite journal | last=Chen | first=Simiao | last2=Yang | first2=Juntao | last3=Yang | first3=Weizhong | last4=Wang | first4=Chen | last5=Bärnighausen | first5=Till | title=COVID-19 control in China during mass population movements at New Year | journal=The Lancet | publisher=Elsevier BV | volume=395 | issue=10226 | year=2020 | issn=0140-6736 | doi=10.1016/s0140-6736(20)30421-9 | pages=764–766}}</ref> | * CXR typically shows patchy or diffuse asymmetric airspace opacities which is also seen in other [[coronaviruses]] cases.<ref name="Chen Yang Yang Wang 2020 pp. 764–766">{{cite journal | last=Chen | first=Simiao | last2=Yang | first2=Juntao | last3=Yang | first3=Weizhong | last4=Wang | first4=Chen | last5=Bärnighausen | first5=Till | title=COVID-19 control in China during mass population movements at New Year | journal=The Lancet | publisher=Elsevier BV | volume=395 | issue=10226 | year=2020 | issn=0140-6736 | doi=10.1016/s0140-6736(20)30421-9 | pages=764–766}}</ref> | ||
[[File:Covid-19-pneumonia-42.jpeg|300px|thumb|none|Chest radiograph on admission demonstrates bilateral, almost symmetrical areas of peripheral consolidation with perihilar infiltrates and an indistinct left heart border. In an endemic area, appearances are highly suggestive of COVID-19. | |||
[[File:Covid-19-pneumonia-42.jpeg|300px|thumb|none|Chest radiograph on admission demonstrates bilateral, almost symmetrical areas of peripheral consolidation with perihilar infiltrates and an indistinct left heart border. In an endemic area, appearances are highly suggestive of COVID-19. [https://radiopaedia.org/cases/covid-19-pneumonia-42?lang=us Source: Dr. Roma Patel]]] | |||
===Echocardiography or Ultrasound=== | ===Echocardiography or Ultrasound=== | ||
| Line 308: | Line 257: | ||
**Traction [[bronchiectasis]] | **Traction [[bronchiectasis]] | ||
[[File:Covid-19-pneumonia-89.png|thumb|300px|none|Key findings: 1) two small areas of ground-glass opacity (GGO) on day 3 | [[File:Covid-19-pneumonia-89.png|thumb|300px|none|Key findings: 1) two small areas of ground-glass opacity (GGO) on day 3 2) extensive crazy-paving pattern (red arrowhead) and consolidations (blue arrowheads) and bilateral pleural effusions (red measurement) on day 15. [https://radiopaedia.org/cases/covid-19-pneumonia-89?lang=us Source: Dr. Joachim Feger]]] | ||
2) extensive crazy-paving pattern (red arrowhead) and consolidations (blue arrowheads) and bilateral pleural effusions (red measurement) on day 15 | |||
===Other Diagnostic Studies=== | ===Other Diagnostic Studies=== | ||
| Line 323: | Line 271: | ||
* For suspected [[bacterial]] co-infection which may depict as elevated [[WBC]], positive [[sputum culture]], positive urinary antigen and atypical chest imaging, administer empiric coverage for [[Community-acquired pneumonia|community-acquired]] or [[Hospital-acquired pneumonia|health-care associated pneumonia]]. | * For suspected [[bacterial]] co-infection which may depict as elevated [[WBC]], positive [[sputum culture]], positive urinary antigen and atypical chest imaging, administer empiric coverage for [[Community-acquired pneumonia|community-acquired]] or [[Hospital-acquired pneumonia|health-care associated pneumonia]]. | ||
* As there have been 3 distinct [[phenotypes]] of COVID-19 pneumonia, so there have been different treatment modalities for each of them. | * As there have been 3 distinct [[phenotypes]] of COVID-19 pneumonia, so there have been different treatment modalities for each of them. | ||
* The first step is to reverse [[hypoxemia]] which can be done through increase in [[FiO2|FiO<sub>2</sub>]]. This is well tolerated in patients with Type L pneumonia. | * The first step is to reverse [[hypoxemia]] which can be done through increase in [[FiO2|FiO<sub>2</sub>]]. This is well tolerated in patients with Type L pneumonia. | ||
| Line 334: | Line 281: | ||
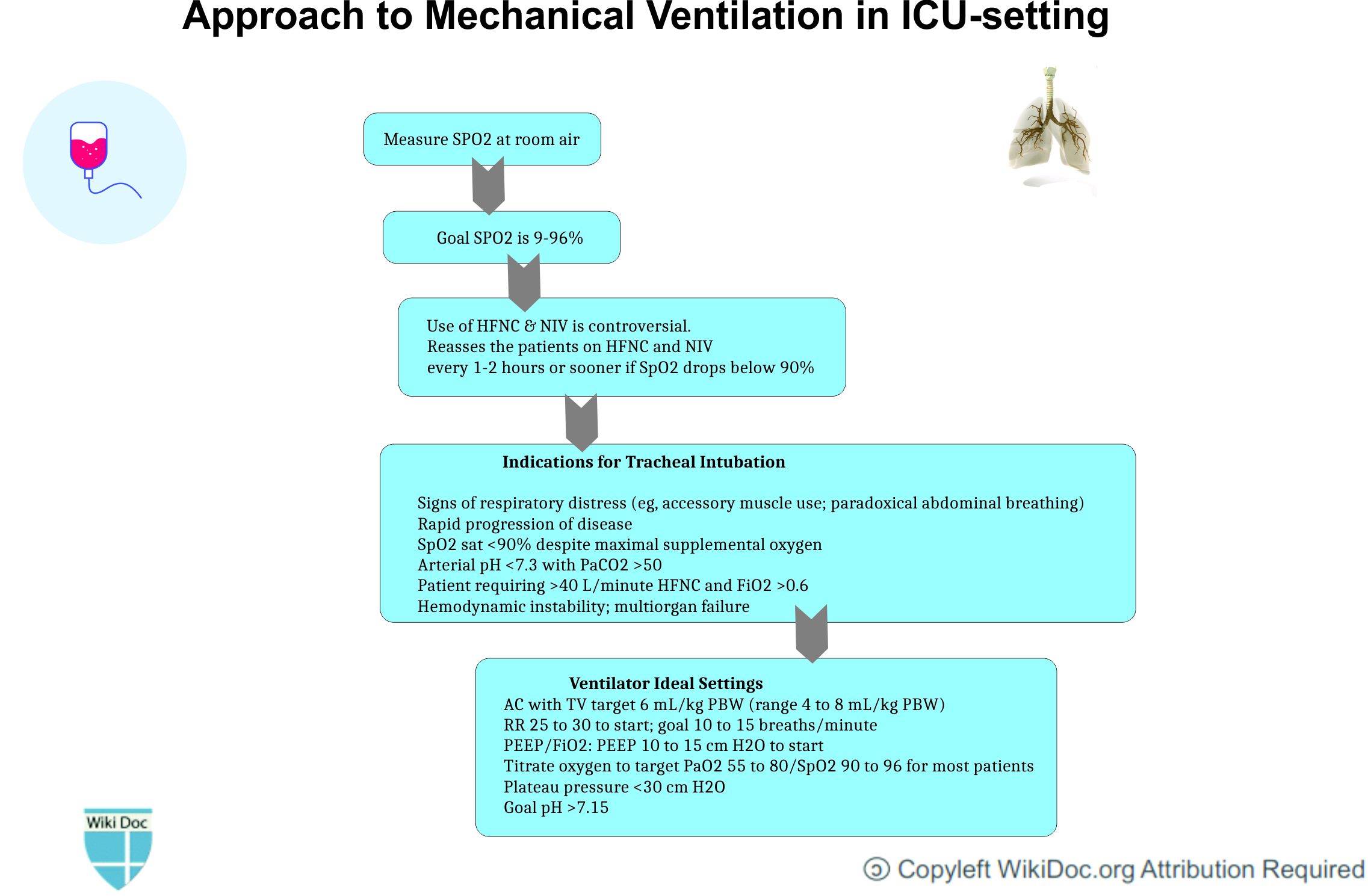
*[[Ventilation|Mechanical Ventilation]] should be instituted at the appropriate time. | *[[Ventilation|Mechanical Ventilation]] should be instituted at the appropriate time. | ||
[[File: | [[File:Corel-draw-pneumonia-mechanical vent-temp.jpg|800px|center]] | ||
===Primary Prevention=== | ===Primary Prevention=== | ||
*The best way to prevent being infected by COVID-19 is to avoid being exposed to this [[virus]] by adopting the following practices for [[infection]] control: | *The best way to prevent being infected by COVID-19 is to avoid being exposed to this [[virus]] by adopting the following practices for [[infection]] control: | ||
| Line 353: | Line 299: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Up-To-Date]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 18:56, 29 July 2020
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
For COVID-19 patient information, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Usman Ali Akbar, M.B.B.S.[2]
Synonyms and keywords:2019 novel coronavirus disease, COVID19, Wuhan virus, L type COVID pneumonia, H type Pneumonia
Overview
In December 2019, a novel coronavirus was detected in pneumonia patients in the Chinese city of Wuhan. The novel coronavirus was later named as 2019-nCoV. Since it was identified, pneumonia appears to be the most frequent manifestation of infection. Despite mimicking the symptoms and criteria of Berlin's definition of ARDS, COVID-19 pneumonia is a distinct disease with features including severe hypoxemia often associated with the normal or near-normal respiratory system compliance.
Historical Perspective
- In December 2019, there were case reports of a cluster of acute respiratory illness in the Wuhan, Hubei Province, China.
- In January 2020, novel coronavirus was identified in the samples of bronchoalveolar lavage fluid from a patient in Wuhan.[1]
- Later this has been confirmed as the cause of novel corona virus-infected pneumonia.
- The first cases were reported by Huang et al in which most of the patients had a history of exposure to the seafood wholesale market.
- There have been no effective therapies or vaccines available for NCIP as of yet.
- In May 2020, it was postulated that there is also a third distinctive type. This phenotype usually mimics the patchy ARDS phenotype.
Classification
- There is no established system for the classification of coronavirus infected pneumonia. Based on the detailed observation of case reports and case series, it has been found that COVID-19 patients differ in their presentation in the emergency department based upon the following three factors:
- The severity of infection, host immune response, preserved physiological reserve, and associated comorbidities.
- Response of patient to the hypoxemia in terms of ventilator
- the time between the presentation of patient to the emergency department and the onset of the disease.
- Based on these three factors, NCIP has been divided COVID-19 associated pneumonia into the following two different phenotypes[2] :
| COVID‑19 pneumonia, Type L | COVID‑19 pneumonia, Type H |
|---|---|
| Low elastance | High elastance |
| Low ventilation to perfusion ratio | High Left to right shunt |
| Low lung weight | High lung weight |
| Low lung recruitability. | High lung recruitability |
- The H type pattern has been reported to present in 20-30 % patients in one case series. It usually fits the criteria of severe ARDS or progresses rapidly towards ARDS.[2]
- In May 2020, it was postulated that there is also a third distinctive type. This phenotype usually mimics the patchy ARDS phenotype.
Pathophysiology
The exact pathogenesis behind COVID-19 associated pneumonia is not yet fully understood.
- COVID-19 usually express trans-membrane glycoproteins which are called "spike proteins" that allow the virus to attach itself to the target organ and enter into the cell [3]
- Spike proteins bind to surface angiotensin converting enzyme 2 (ACE2) receptors. Specifically, the RBD of the S protein of SARS-CoV-2 recognizes ACE2 receptors.
- ACE2 is predominately expressed on type II pneumocytes. Other proteins such as TMPRSS2 is also required for complete binding and transmissibility.
- TMPRSS2 cleaves the S protein and results into the fusion of the viral and host cell membrane.[4]
- The virus replicates itself in the target cell using RNA dependent RNA polymerase.
- Lungs seems to be more vulnerable to the SARS-CoV-2 because of the large surface area.
- Direct lung injury leading to release of various cytokines such as (IL)–1β, IL-2, IL-6, IL-7, IL-12, IL-18, tumor necrosis factor (TNF)–α, interferon (IFN)–γ, and granulocyte colony-stimulating factor (GCSF) initiates local inflammatory response and is responsible for the pulmonary manifestations of COVID-19.[5]
- This leads to a modest local subpleural interstitial edema (ground glass lesions) at the interfaces between lung structures
- Vasoplegia results which further accounts for severe hypoxemia.

Differentiating COVID-19-associated pneumonia from other Diseases
- For further information on COVID-19-associated pneumonia click here.
- To view the COVID-19 differential diagnosis click here.
Epidemiology and Demographics
| Date Published | Author | Country | Total Number Of Patients | Incidence/Prevalence |
|---|---|---|---|---|
| 01 June,2020 | San-Juan Rafael. [6] | Spain | 65 | 61.5 % |
| 21 April 2020 | Streng A. [7] | China | 2143 | 39–82% |
| 10 April 2020 | Fu Leiwen. et al [8] | China | 3600 | 73.2 % |
Age
- In another study it was reported that the mean age of the population was 45 years, and 307 (79%) of 391 cases were adults aged 30–69 years.
- At the time of the first clinical assessment, most cases were mild (102 [26%] of 391) or moderate (254 [65%] of 391), and only 35 (9%) were severe.[9]
Gender
- The attack rate was reported to be more among females than male cases.[9]
Race
- There is no significant data reporting specific race predilection for the patients developing COVID-19 associated pneumonia.
Risk Factors
- The risk factors for COVID-19 associated pneumonia have not been properly established. Multiple studies show following factors to be the key to the progression of disease severity:[10]
- Diarrhea
- Lymphocyte count ≤ 1000 microlitre
- Ferritin ≥ 430 ng/ml
- CRP ≥ 2.5 mg/dL
- Consolidation on CT-scan chest
- Declining Neutrophil count
- COPD history
Screening
- There is insufficient evidence to recommend routine screening for COVID-19 associated pneumonia.
Natural History, Complications, and Prognosis
- Due to the evolution of pneumonia and high stress ventilation given as a part of treatment,type L COVID-19 pneumonia may progress to type H pneumonia over time.
- The key feature that regulates this transition is the depth of the negative inspiratory intrathoracic pressure that is associated with increased tidal volume in spontaneous breathing.[11]
- This is based on experimental observation by Barach and Mascheroni. This has been termed as patient self-inflicted lung injury. Over time the increased edema causes lung weight to increase.
- There is superimposed pressure and dependent atelectasis that develops over the progression of time.
- When the lung edema increases massively, the lung's gas volume decreases and then tidal volumes that are usually generated for a given pressure also decreases.
- This leads to the development of dyspnea and worsening of the patient's self-inflicted lung injury.[12]
Complications
- Pneumonia due to SARS-CoV-2 can further lead to following complications:
- Worsening hypoxemia[11]
- ARDS
- Barotrauma due to mechanical breathing support
- Acute cor-pulmonale
- Ventilator associated pneumonia
Prognosis
- Generally the progression of L Type pneumonia to the H type co-relates to poor prognosis as it further rapidly progresses to ARDS.
- A study reported development of ARDS in 20% patients with a median of eight days after the onset of symptoms.[1]
Diagnosis
Diagnostic Study of Choice
- There is no established criteria for the diagnosis of COVID-19 associated pneumonia.
- Initial chest x-rays maybe normal.
- CT-scan chest is more sensitive than chest x-ray but there are no set criteria to diagnose COVID-19 associated pneumonia in COVID-19 patients.
History and Symptoms
- Exposure to SARS-CoV-2 can result into patients exhibiting following signs and symptoms:
- Most common signs and symptoms:
- Low to high-grade fever (98.6%)
- Generalized fatigue (69.6%)
- Non-productive/dry cough (59.4%)
- Myalgias (34.8%)
- Dyspnea (31.2%)
- Sore throat
- Rhinorrhea
- Other less common signs and symptoms:
- Most common signs and symptoms:
| Mild Illness | Moderate Pneumonia | Severe Pneumonia |
|---|---|---|
|
|
|
| ||
|
|
Physical Examination
- Common physical examination findings include the following:
- Fever (most common)
- Respiratory rate >24 breaths/minute (almost all patients)
- Pulse rate >100 beats/min.
- Audible crackles (on chest examination)
- Signs of consolidation can be present in as early signs of pneumonia in COVID-19 patients such as:
- Decreased or bronchial breath sounds
- Dullness to percussion
- Tactile fremitus
- Egophony
Laboratory Findings
- Common laboratory findings among hospitalized patients with COVID-19 include:
- Lymphopenia (lymphocyte count, 0.8 × 109/L [interquartile range {IQR}, 0.6-1.1])
- Elevated aminotransaminase levels
- Elevated lactate dehydrogenase levels
- Elevated ferritin
- Elevated CRP
- Elevated ESR
- Elevated procalcitonin levels in those requiring ICU care
Electrocardiogram
- There are no specific ECG findings associated with COVID-19 associated pneumonia.
X-ray
- Chest radiograph may show bilateral, almost symmetrical areas of peripheral consolidation with perihilar infiltrates. In an endemic area, these appearances are highly suggestive of infection with COVID-19.
- The primary findings of COVID-19 are those of atypical or organizing pneumonia.[13]
- Almost 18 % of the patients can have normal chest x-ray findings early in the disease course but only 3% in severe disease.[14]
- Bilateral and/or multilobar involvement is common.
- CXR typically shows patchy or diffuse asymmetric airspace opacities which is also seen in other coronaviruses cases.[15]

Echocardiography or Ultrasound
- There are no specific echocardiography/ultrasound findings associated with COVID-19 associated pneumonia.
CT scan
- CT-scan chest findings in a patient with COVID-19 pneumonia may show following abnormalities:[16]
- Ground-glass opacities
- Crazy paving appearance
- Air space consolidation
- Bronchovascular thickening in the lesion
- Traction bronchiectasis

Other Diagnostic Studies
Bronchoalveolar Lavage
- Bronchoalveolar lavage may not be useful in diagnosing COVID-19 pneumonia, however various case reports suggest a collection of BAL fluid when consecutive nasopharyngeal swabs are negative to confirm or exclude the diagnosis of COVID-19-associated pneumonia.[17]
Treatment
Medical Therapy
- The mainstay of treatment for COVID-19 associated pneumonia is supportive care and mechanical respiratory support.
- For suspected bacterial co-infection which may depict as elevated WBC, positive sputum culture, positive urinary antigen and atypical chest imaging, administer empiric coverage for community-acquired or health-care associated pneumonia.
- As there have been 3 distinct phenotypes of COVID-19 pneumonia, so there have been different treatment modalities for each of them.
- The first step is to reverse hypoxemia which can be done through increase in FiO2. This is well tolerated in patients with Type L pneumonia.
- For L Type with dyspnea, following different non-invasive options are available:
- High flow nasal cannula (HFNC)
- Continuous positive airway pressure (CPAP)
- Non-invasive ventilation (NIV)
- Esophageal manometry pressure is measured to prevent swings of central venous pressure.
- P0.1 and Pocclusion should be measured in intubated patient.
- Mechanical Ventilation should be instituted at the appropriate time.
Primary Prevention
- The best way to prevent being infected by COVID-19 is to avoid being exposed to this virus by adopting the following practices for infection control:
- Often wash hands with soap and water for at least 20 seconds.
- Use an alcohol-based hand sanitizer containing at least 60% alcohol in case soap and water are not available.
- Avoid touching the eyes, nose, and mouth without washing hands.
- Avoid being in close contact with people sick with COVID-19 infection.
- Stay home while being symptomatic to prevent spread to others.
- Cover mouth while coughing or sneezing with a tissue paper, and then throw the tissue in the trash.
- Clean and disinfect the objects and surfaces which are touched frequently.
- There is currently no vaccine available to prevent COVID-19.
Secondary Prevention
- The secondary prevention measures of Coronavirus disease 2019 (COVID-19) constitute protective measures to make sure that an infected individual does not transfer the disease to others by maintaining self-isolation at home or designated quarantine facilities.
References
- ↑ 1.0 1.1 1.2 Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020-03-17). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. American Medical Association (AMA). 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ 2.0 2.1 "COVID-19-associated pneumonia". wikidoc. 2020-03-17. Retrieved 2020-07-13.
- ↑ Yuki, Koichi; Fujiogi, Miho; Koutsogiannaki, Sophia (2020). "COVID-19 pathophysiology: A review". Clinical Immunology. Elsevier BV. 215: 108427. doi:10.1016/j.clim.2020.108427. ISSN 1521-6616.
- ↑ Glowacka, I.; Bertram, S.; Muller, M. A.; Allen, P.; Soilleux, E.; Pfefferle, S.; Steffen, I.; Tsegaye, T. S.; He, Y.; Gnirss, K.; Niemeyer, D.; Schneider, H.; Drosten, C.; Pohlmann, S. (2011-02-16). "Evidence that TMPRSS2 Activates the Severe Acute Respiratory Syndrome Coronavirus Spike Protein for Membrane Fusion and Reduces Viral Control by the Humoral Immune Response". Journal of Virology. American Society for Microbiology. 85 (9): 4122–4134. doi:10.1128/jvi.02232-10. ISSN 0022-538X.
- ↑ Costela-Ruiz, Víctor J.; Illescas-Montes, Rebeca; Puerta-Puerta, Jose M.; Ruiz, Concepción; Melguizo-Rodríguez, Lucia (2020). "SARS-CoV-2 infection: The role of cytokines in COVID-19 disease". Cytokine & Growth Factor Reviews. Elsevier BV. doi:10.1016/j.cytogfr.2020.06.001. ISSN 1359-6101.
- ↑ San-Juan, Rafael; Barbero, Patricia; Fernández-Ruiz, Mario; López-Medrano, Francisco; Lizasoáin, Manuel; Hernández-Jiménez, Pilar; Silva, José Tiago; Ruiz-Ruigómez, María; Corbella, Laura; Rodríguez-Goncer, Isabel; Folgueira, María Dolores; Lalueza, Antonio; Batllori, Emma; Mejía, Inma; Forcén, Laura; Lumbreras, Carlos; García-Burguillo, Antonio; Galindo, Alberto; Aguado, José María (2020). "Incidence and clinical profiles of COVID-19 pneumonia in pregnant women: A single-centre cohort study from Spain". EClinicalMedicine. Elsevier BV. 23: 100407. doi:10.1016/j.eclinm.2020.100407. ISSN 2589-5370.
- ↑ Streng, A.; Hartmann, K.; Armann, J.; Berner, R.; Liese, J. G. (2020-04-21). "COVID-19 bei hospitalisierten Kindern und Jugendlichen". Monatsschrift Kinderheilkunde (in Deutsch). Springer Science and Business Media LLC. 168 (7): 615–627. doi:10.1007/s00112-020-00919-7. ISSN 0026-9298.
- ↑ Fu, Leiwen; Wang, Bingyi; Yuan, Tanwei; Chen, Xiaoting; Ao, Yunlong; Fitzpatrick, Thomas; Li, Peiyang; Zhou, Yiguo; Lin, Yi-fan; Duan, Qibin; Luo, Ganfeng; Fan, Song; Lu, Yong; Feng, Anping; Zhan, Yuewei; Liang, Bowen; Cai, Weiping; Zhang, Lin; Du, Xiangjun; Li, Linghua; Shu, Yuelong; Zou, Huachun (2020). "Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis". Journal of Infection. Elsevier BV. 80 (6): 656–665. doi:10.1016/j.jinf.2020.03.041. ISSN 0163-4453.
- ↑ 9.0 9.1 Bi, Qifang; Wu, Yongsheng; Mei, Shujiang; Ye, Chenfei; Zou, Xuan; Zhang, Zhen; Liu, Xiaojian; Wei, Lan; Truelove, Shaun A; Zhang, Tong; Gao, Wei; Cheng, Cong; Tang, Xiujuan; Wu, Xiaoliang; Wu, Yu; Sun, Binbin; Huang, Suli; Sun, Yu; Zhang, Juncen; Ma, Ting; Lessler, Justin; Feng, Tiejian (2020). "Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study". The Lancet Infectious Diseases. Elsevier BV. doi:10.1016/s1473-3099(20)30287-5. ISSN 1473-3099.
- ↑ Wang, Chang‐Zheng; Hu, Shun‐Lin; Wang, Lin; Li, Min; Li, Huan‐Tian (2020-05-29). "Early risk factors of the exacerbation of Coronavirus disease 2019 pneumonia". Journal of Medical Virology. Wiley. doi:10.1002/jmv.26071. ISSN 0146-6615.
- ↑ 11.0 11.1 Gattinoni, Luciano; Chiumello, Davide; Caironi, Pietro; Busana, Mattia; Romitti, Federica; Brazzi, Luca; Camporota, Luigi (2020-04-14). "COVID-19 pneumonia: different respiratory treatments for different phenotypes?". Intensive Care Medicine. Springer Science and Business Media LLC. 46 (6): 1099–1102. doi:10.1007/s00134-020-06033-2. ISSN 0342-4642.
- ↑ Robba, Chiara; Battaglini, Denise; Ball, Lorenzo; Patroniti, Nicolo’; Loconte, Maurizio; Brunetti, Iole; Vena, Antonio; Giacobbe, Daniele Roberto; Bassetti, Matteo; Rocco, Patricia Rieken Macedo; Pelosi, Paolo (2020). "Distinct phenotypes require distinct respiratory management strategies in severe COVID-19". Respiratory Physiology & Neurobiology. Elsevier BV. 279: 103455. doi:10.1016/j.resp.2020.103455. ISSN 1569-9048.
- ↑ Rodrigues, J.C.L.; Hare, S.S.; Edey, A.; Devaraj, A.; Jacob, J.; Johnstone, A.; McStay, R.; Nair, A.; Robinson, G. (2020). "An update on COVID-19 for the radiologist - A British society of Thoracic Imaging statement". Clinical Radiology. Elsevier BV. 75 (5): 323–325. doi:10.1016/j.crad.2020.03.003. ISSN 0009-9260.
- ↑ Guan, Wei-jie; Ni, Zheng-yi; Hu, Yu; Liang, Wen-hua; Ou, Chun-quan; He, Jian-xing; Liu, Lei; Shan, Hong; Lei, Chun-liang; Hui, David S.C.; Du, Bin; Li, Lan-juan; Zeng, Guang; Yuen, Kwok-Yung; Chen, Ru-chong; Tang, Chun-li; Wang, Tao; Chen, Ping-yan; Xiang, Jie; Li, Shi-yue; Wang, Jin-lin; Liang, Zi-jing; Peng, Yi-xiang; Wei, Li; Liu, Yong; Hu, Ya-hua; Peng, Peng; Wang, Jian-ming; Liu, Ji-yang; Chen, Zhong; Li, Gang; Zheng, Zhi-jian; Qiu, Shao-qin; Luo, Jie; Ye, Chang-jiang; Zhu, Shao-yong; Zhong, Nan-shan (2020-04-30). "Clinical Characteristics of Coronavirus Disease 2019 in China". New England Journal of Medicine. Massachusetts Medical Society. 382 (18): 1708–1720. doi:10.1056/nejmoa2002032. ISSN 0028-4793.
- ↑ Chen, Simiao; Yang, Juntao; Yang, Weizhong; Wang, Chen; Bärnighausen, Till (2020). "COVID-19 control in China during mass population movements at New Year". The Lancet. Elsevier BV. 395 (10226): 764–766. doi:10.1016/s0140-6736(20)30421-9. ISSN 0140-6736.
- ↑ Bai, Harrison X.; Hsieh, Ben; Xiong, Zeng; Halsey, Kasey; Choi, Ji Whae; Tran, Thi My Linh; Pan, Ian; Shi, Lin-Bo; Wang, Dong-Cui; Mei, Ji; Jiang, Xiao-Long; Zeng, Qiu-Hua; Egglin, Thomas K.; Hu, Ping-Feng; Agarwal, Saurabh; Xie, Fangfang; Li, Sha; Healey, Terrance; Atalay, Michael K.; Liao, Wei-Hua (2020-03-10). "Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT". Radiology. Radiological Society of North America (RSNA): 200823. doi:10.1148/radiol.2020200823. ISSN 0033-8419.
- ↑ Gualano, Gina; Musso, Maria; Mosti, Silvia; Mencarini, Paola; Mastrobattista, Annelisa; Pareo, Carlo; Zaccarelli, Mauro; Migliorisi, Paolo; Vittozzi, Pietro; Zumla, Alimudin; Ippolito, Giuseppe; Palmieri, Fabrizio (2020). "Usefulness of bronchoalveolar lavage in the management of patients presenting with lung infiltrates and suspect COVID-19-associated pneumonia: A case report". International Journal of Infectious Diseases. Elsevier BV. 97: 174–176. doi:10.1016/j.ijid.2020.05.027. ISSN 1201-9712.