Barrett's esophagus pathophysiology
|
Barrett's Esophagus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Barrett's esophagus pathophysiology On the Web |
|
American Roentgen Ray Society Images of Barrett's esophagus pathophysiology |
|
Risk calculators and risk factors for Barrett's esophagus pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amresh Kumar MD [2]
Overview
Barrett's esophagus is marked by the presence of columnar epithelium in the lower esophagus, replacing the normal squamous cell epithelium; an example of metaplasia. The columnar epithelium is better able to withstand the erosive action of the gastric secretions; however, this metaplasia confers an increased cancer risk of the adenocarcinoma type.[1][2]
Pathophysiology
Pathogenesis
- The metaplastic columnar cells may be of two types: gastric similar to those in the stomach, which is NOT technically Barrett's esophagus) or colonic similar to cells in the intestine. A biopsy of the affected area will often contain a mixture of the two. Colonic-type metaplasia is the type of metaplasia associated with increased risk of malignancy in genetically susceptible people.
- The metaplasia of Barrett's esophagus is visible grossly through a gastroscope, but biopsy specimens must be examined under a microscope to determine whether cells are gastric or colonic in nature. Colonic metaplasia is usually identified by finding goblet cells in the epithelium and is necessary for the final diagnosis of Barrett's.
- There are many histological mimics of Barrett's esophagus (i.e. goblet cells occurring in the transitional epithelium of normal esophageal submucosal gland ducts, "pseudo goblet cells" in which abundant foveolar (gastric) type mucin simulates the acid mucin true goblet cells). Assessment of relationship to submucosal glands and transitional-type epithelium with examination of multiple levels through the tissue may allow the pathologist to reliably distinguish between goblet cells of submucosal gland ducts and true Barrett's esophagus (specialized columnar metaplasia). Use of the histochemical stain Alcian blue (with pH=2.5) is also frequently used to distinguish true intestinal-type mucin from their histological mimics. Recently, immunohistochemical analysis with antibodies to CDX-2 (specific for mid and hind-gut intestinal derivation) has also been utilized to identify true intestinal-type metaplastic cells.
- In the United States, it is estimated that 8 - 12% of patients who are diagnosed with Barrett's esophagus have been misdiagnosed. This significant diagnostic error may result in higher rates of medical and life insurance rates for those misdiagnosed; as well as enrollment of patients in unnecessary surveillance programs (i.e. annual endoscopic evaluation and biopsy to monitor for the development of Barrett's esophagus). Second (consulting) opinions on pathologic materials are easily available as slides and tissue blocks are retained for 10 and 20 years, respectively. To request a consultation opinion, patients may contact their gastroenterologist for referral to a GI pathology specialty center.
- After the initial diagnosis of Barrett's esophagus is rendered, affected persons undergo annual surveillance to detect changes that indicate higher risk to progression to cancer: development of dysplasia. There is considerable variability in assessment for dysplasia among pathologists. Recently, gastroenterology and GI pathology societies have recommended that any diagnosis of high grade dysplasia in Barrett's be confirmed by at least two fellowship trained GI pathologists prior to definitive treatment for patients.
- Recent evidence has pointed to a similar condition developing in the distal gut epithelium. Barrett's Anus is a metaplastic change in the distal rectum whose cellularity is similar to that of the gastric mucosa. While the condition is stable for many years, there has been recent evidence to show that it is the predisposing lesion to both anal teratoma and squamous cell carcinoma of the anus. Frequent bouts of steatorrhea are commonly cited as the most likely cause of Barrett's Anus, but much more research needs to be done in order to rule out causes such as HPV 8,13.
- It appears that chronic GE reflux is causes the injury – repair cycle that stimulates squamous metaplasia. The columnar cells are more resistant to acid injury than the squamous cells.
- Although one would think that BE develops over years, with slow replacement of squamous cells by columnar cells, it appears that this is not the case. BE tends to develop all at once with little or no progression. The reason for this is unknown.
Genetics
- The development of Barrett's esophagus is the result of multiple genetic mutations including mutations on chromosome 11p in European ancestry[3], genetic mutation of MGST1[4], mutations of genes GDF7 and TBX5[5] and polymorphisms in genes in the androgen pathway[6].
Associated Conditions
Gross Pathology
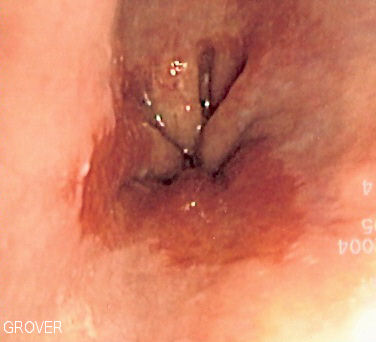
- Normally the mucosa of normal esophagus is light pink color as seen from underlying picture.
- On gross pathology, Barrett's esophagus looks like Red/light brown esophageal mucosa.
Microscopic Pathology
- On microscopic histopathological analysis, gastric junctional type epithelium, gastric fundus type epithelium and specialized intestinal columnar metaplasia are characteristic findings of Barrett's esophagus.[12]
- Paull et.al. described three types of columnar epithelium that can be seen in BE:
- Gastric junctional-type epithelium which has a pitted (foveolar) surface and mucus-secreting cells.
- Gastric fundus-type epithelium that also has a pitted surface lined by mucus-secreting cells, in addition to having a deeper glandular layer that contains chief and parietal cells.
- Specialized intestinal (columnar) metaplasia that has a villiform surface with mucus secreting columnar cells and goblet cells.

References
- ↑ Fléjou J (2005). "Barrett's oesophagus: from metaplasia to dysplasia and cancer". Gut. 54 Suppl 1: i6–12. PMID 15711008.
- ↑ Rumiato E, Boldrin E, Malacrida S, Realdon S, Fassan M, Morbin T; et al. (2017). "Detection of genetic alterations in cfDNA as a possible strategy to monitor the neoplastic progression of Barrett's esophagus". Transl Res. 190: 16–24.e1. doi:10.1016/j.trsl.2017.09.004. PMID 29066320.
- ↑ Sun X, Chandar AK, Canto MI, Thota PN, Brock M, Shaheen NJ; et al. (2017). "Genomic regions associated with susceptibility to Barrett's esophagus and esophageal adenocarcinoma in African Americans: The cross BETRNet admixture study". PLoS One. 12 (10): e0184962. doi:10.1371/journal.pone.0184962. PMC 5657624. PMID 29073141.
- ↑ Buas MF, He Q, Johnson LG, Onstad L, Levine DM, Thrift AP; et al. (2017). "Germline variation in inflammation-related pathways and risk of Barrett's oesophagus and oesophageal adenocarcinoma". Gut. 66 (10): 1739–1747. doi:10.1136/gutjnl-2016-311622. PMC 5296402. PMID 27486097.
- ↑ Becker J, May A, Gerges C, Anders M, Schmidt C, Veits L; et al. (2016). "The Barrett-associated variants at GDF7 and TBX5 also increase esophageal adenocarcinoma risk". Cancer Med. 5 (5): 888–91. doi:10.1002/cam4.641. PMC 4864818. PMID 26783083.
- ↑ Ek WE, Lagergren K, Cook M, Wu AH, Abnet CC, Levine D; et al. (2016). "Polymorphisms in genes in the androgen pathway and risk of Barrett's esophagus and esophageal adenocarcinoma". Int J Cancer. 138 (5): 1146–52. doi:10.1002/ijc.29863. PMC 4715576. PMID 26414697.
- ↑ von Schrenck T (2000). "[Diagnosis of gastroesophageal reflux and Barrett esophagus]". Zentralbl Chir. 125 (5): 414–23. PMID 10929625.
- ↑ Minacapelli CD, Bajpai M, Geng X, Cheng CL, Chouthai AA, Souza R; et al. (2017). "Barrett's metaplasia develops from cellular reprograming of esophageal squamous epithelium due to gastroesophageal reflux". Am J Physiol Gastrointest Liver Physiol. 312 (6): G615–G622. doi:10.1152/ajpgi.00268.2016. PMID 28336546.
- ↑ Wipff J, Allanore Y, Soussi F, Terris B, Abitbol V, Raymond J; et al. (2005). "Prevalence of Barrett's esophagus in systemic sclerosis". Arthritis Rheum. 52 (9): 2882–8. doi:10.1002/art.21261. PMID 16142744.
- ↑ Drahos J, Li L, Jick SS, Cook MB (2016). "Metabolic syndrome in relation to Barrett's esophagus and esophageal adenocarcinoma: Results from a large population-based case-control study in the Clinical Practice Research Datalink". Cancer Epidemiol. 42: 9–14. doi:10.1016/j.canep.2016.02.008. PMC 4899201. PMID 26972225.
- ↑ Drahos J, Ricker W, Parsons R, Pfeiffer RM, Warren JL, Cook MB (2015). "Metabolic syndrome increases risk of Barrett esophagus in the absence of gastroesophageal reflux: an analysis of SEER-Medicare Data". J Clin Gastroenterol. 49 (4): 282–8. doi:10.1097/MCG.0000000000000119. PMC 4176548. PMID 24671095.
- ↑ Booth CL, Thompson KS (2012). "Barrett's esophagus: A review of diagnostic criteria, clinical surveillance practices and new developments". J Gastrointest Oncol. 3 (3): 232–42. doi:10.3978/j.issn.2078-6891.2012.028. PMC 3418534. PMID 22943014.