Amoebic liver abscess pathophysiology: Difference between revisions
Ahmed Younes (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (4 intermediate revisions by 3 users not shown) | |||
| Line 42: | Line 42: | ||
====Variants of amoebic liver abscesses==== | ====Variants of amoebic liver abscesses==== | ||
*Solitary lesions (30%-70%) are more common [[amoebic liver abscess]]es and most commonly seen in [[Right lobe of liver|right lobe of the liver]]. | *Solitary lesions (30%-70%) are more common [[amoebic liver abscess]]es and most commonly seen in [[Right lobe of liver|right lobe of the liver]]. | ||
*The [[Right lobe of liver|right hepatic lobule]] is most commonly effected due to [[portal]] | *The [[Right lobe of liver|right hepatic lobule]] is most commonly effected due to [[Portal circulation|portal circulatory system]] of the [[colon|right colon]]. | ||
{| class="wikitable" style="text-align: Top;" | {| class="wikitable" style="text-align: Top;" | ||
!Multiple liver abscesses | !Multiple liver abscesses | ||
!Left lobe abscess | ![[Left lobe of liver|Left lobe]] abscess | ||
!Compression lesions | !Compression lesions | ||
!Extension of the abscess | !Extension of the abscess | ||
| Line 73: | Line 73: | ||
| | | | ||
*Compression lesions include posteriorly located right lobe abscess which compresses [[inferior vena cava]] or [[hepatic vein]] | *Compression lesions include posteriorly located [[Right lobe of liver|right lobe]] abscess which compresses [[inferior vena cava]] or [[hepatic vein]] | ||
*Presenting features include: | *Presenting features include: | ||
:*Bilateral [[pedal edema]] | :*Bilateral [[pedal edema]] | ||
:*[[Ascites]] | :*[[Ascites]] | ||
:*Visible [[veins]] on anterior and posterior abdominal wall | :*Visible [[veins]] on anterior and posterior [[abdominal wall]] | ||
*Symptoms disappear after [[aspiration]] of [[abscess]] | *Symptoms disappear after [[aspiration]] of [[abscess]] | ||
| | | | ||
| Line 88: | Line 88: | ||
====Gross pathology==== | ====Gross pathology==== | ||
*The amoebic liver abscesses are well circumscribed regions which contain [[necrosis|necrotic]] material (dead [[hepatocytes]], liquefied cells and cellular debris) and the surrounding fibrinous border. | *The amoebic liver abscesses are well circumscribed regions which contain [[necrosis|necrotic]] material (dead [[hepatocytes]], liquefied cells and cellular debris) and the surrounding [[fibrinous]] border. | ||
*The adjacent liver [[parenchyma]] is usually normal. | *The adjacent liver [[parenchyma]] is usually normal. | ||
*The [[abscess]]es are single or multiple. | *The [[abscess]]es are single or multiple. | ||
| Line 96: | Line 96: | ||
====Microscopic pathology==== | ====Microscopic pathology==== | ||
*Multiple [[neutrophil|neutrophilic]] abscess with areas of [[necrosis]] are seen in the liver [[parenchyma]]. | *Multiple [[neutrophil|neutrophilic]] abscess with areas of [[necrosis]] are seen in the liver [[parenchyma]]. | ||
*A rim of [[connective tissue]], with few inflammatory cells and amoebic [[trophozoites]] are clustered in the fibrin at the junction of viable and [[necrosis|necrotic]] tissue. | *A rim of [[connective tissue]], with few inflammatory cells and amoebic [[trophozoites]] are clustered in the [[fibrin]] at the junction of viable and [[necrosis|necrotic]] tissue. | ||
[[File:Microscopic_pathology.jpg|Amoebic liver abscess|300px]] | [[File:Microscopic_pathology.jpg|Amoebic liver abscess|300px]] | ||
| Line 103: | Line 103: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Gastroenterology]] | |||
[[Category:Surgery]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Infectious disease]] | |||
[[Category:Hepatology]] | |||
Latest revision as of 20:23, 29 July 2020
|
Amoebic liver abscess Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Amoebic liver abscess pathophysiology On the Web |
|
American Roentgen Ray Society Images of Amoebic liver abscess pathophysiology |
|
Risk calculators and risk factors for Amoebic liver abscess pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Yamuna Kondapally, M.B.B.S[2]
Overview
Ameoebic liver abscess is caused by a protozoan Entamoeba histolytica. It is the most common extraintestinal manifestation of amoebiasis. The mode of transmission of Entamoeba histolytica include fecal-oral route (ingestion of food and water contaminated with feces containing cysts), sexual transmission via oral-rectal route in homosexuals, vector transmission via flies, cockroaches, and rodents.[1][2] Hepatocyte programmed cell death induced by Entamoeba histolytica causes amoebic liver abscess. The infection is transmitted to liver by portal venous system.[3]
Pathophysiology
- Amoebic liver abscess is the most common extraintestinal manifestation of amoebiasis.
- There are two genetically different species of entamoeba.[4] They are
- The mode of transmission of Entamoeba histolytica include:[1][2]
- Fecal-oral route (ingestion of food and water contaminated with feces containing cysts)
- Sexual transmission via oral-rectal route in homosexuals
- Vector transmission via flies, cockroaches, and rodents.
- Hepatocyte programmed cell death induced by Entamoeba histolytica causes amoebic liver abscess.
- The infection is transmitted to liver by portal venous system.[3]
- Clinical syndromes associated with Entamoeba histolytica infection
| Entamoeba histolytica | |||||||||||||||||||||||||||||||||||||||||||||||
| Intestinal amoebiasis • Asymptomatic cyst passers • Acute amoebic colitis • Mucosal disease • Transmural disease • Ulcerative post dysentric colitis • Appendicitis • Amoeboma • Amoebic stricture | Extra intestinal amoebiasis • Amoebic liver abscess • Perforation and peritonitis • Pleuropulmonary amoebiasis • Amoebic pericarditis • Cutaneous amoebiasis | ||||||||||||||||||||||||||||||||||||||||||||||
Pathogenesis
- After ingestion of contaminated food and water, Entamoeba histolytica trophozoites adhere to epithelial cells of colon, through the galactose/N-acetylgalactosamine specific lectin.[5]
- After adhesion, the parasite releases cysteine proteinases which digest extracellular matrix proteins. This facilitate trophozoite invasion into submucosal tissue through amoebapore leading to activation of amoebic virulence program.[6][7]
- The extracellular amoebic cysteine proteinase converts pIL-1β (precursor interleukin 1β) to active IL-1β. The chemokines and cytokines released from epithelial cells attract macrophages and neutrophils to the site of infection.[8]
- Neutrophils transmigrating to the epithelial surface facilitate E histolytica invasion by creating channels. Cysteine proteinases digest extracellular matrix protein, causing epithelial cells to break from the villi, which also aid in the parasite's direct invasion into submucosal tissues.[9]
- The mediators released by the neutrophils cause more damage to adjacent intestinal epithelial cells.[10]
- The trophozoites penetrate the mucosa, submucosal tissues and even into the portal circulation where they encounter additional host defenses, including complement system.
- E. histolytica are covered by highly glycosylated and phosphorylated lipophosphoglycan which may serve as a physical barrier to complement components. The amoebic Gal/GalNAc lectin has a region with antigenic cross reactivity with CD59 which protect trophozoites against lysis.[11]
- The cysteine proteinases cleave and inactivate the anaphylatoxins C3a and C5a along with human IgA and IgG which provides further defense against host immune response.[12][13]
- The trophozoites which enter the liver through portal circulation leading to apoptosis of liver cells and abscess formation.
- Stages of abscess formation include:
- Acute inflammation
- Granuloma formation
- Necrosis with necrotic abscess or periportal fibrosis
Variants of amoebic liver abscesses
- Solitary lesions (30%-70%) are more common amoebic liver abscesses and most commonly seen in right lobe of the liver.
- The right hepatic lobule is most commonly effected due to portal circulatory system of the right colon.
| Multiple liver abscesses | Left lobe abscess | Compression lesions | Extension of the abscess |
|---|---|---|---|
|
Aspiration + anti-amoebic drugs |
|
|
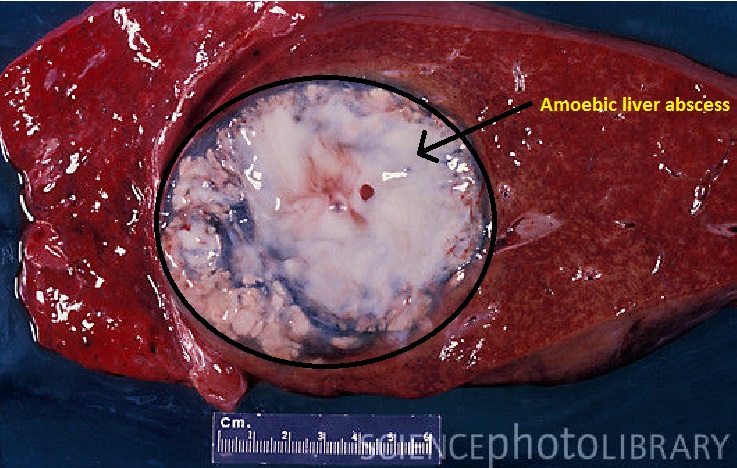
Gross pathology
- The amoebic liver abscesses are well circumscribed regions which contain necrotic material (dead hepatocytes, liquefied cells and cellular debris) and the surrounding fibrinous border.
- The adjacent liver parenchyma is usually normal.
- The abscesses are single or multiple.
- The abscess cavity may be filled with chocolate colored pasty material (anchovy sauce-like).
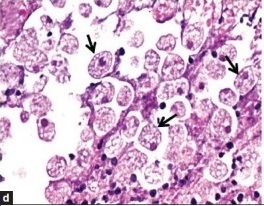
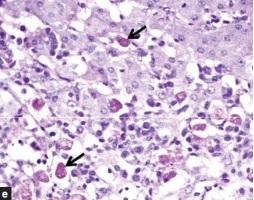
Microscopic pathology
- Multiple neutrophilic abscess with areas of necrosis are seen in the liver parenchyma.
- A rim of connective tissue, with few inflammatory cells and amoebic trophozoites are clustered in the fibrin at the junction of viable and necrotic tissue.
References
- ↑ 1.0 1.1 Fletcher SM, Stark D, Harkness J, Ellis J (2012). "Enteric protozoa in the developed world: a public health perspective". Clin Microbiol Rev. 25 (3): 420–49. doi:10.1128/CMR.05038-11. PMC 3416492. PMID 22763633.
- ↑ 2.0 2.1 Stanley SL (2003). "Amoebiasis". Lancet. 361 (9362): 1025–34. doi:10.1016/S0140-6736(03)12830-9. PMID 12660071.
- ↑ 3.0 3.1 Aikat BK, Bhusnurmath SR, Pal AK, Chhuttani PN, Datta DV (1979). "The pathology and pathogenesis of fatal hepatic amoebiasis--A study based on 79 autopsy cases". Trans. R. Soc. Trop. Med. Hyg. 73 (2): 188–92. PMID 473308.
- ↑ Gonin P, Trudel L (2003). "Detection and differentiation of Entamoeba histolytica and Entamoeba dispar isolates in clinical samples by PCR and enzyme-linked immunosorbent assay". J Clin Microbiol. 41 (1): 237–41. PMC 149615. PMID 12517854.
- ↑ Mann BJ (2002). "Structure and function of the Entamoeba histolytica Gal/GalNAc lectin". Int Rev Cytol. 216: 59–80. PMID 12049210.
- ↑ Leippe M, Andrä J, Nickel R, Tannich E, Müller-Eberhard HJ (1994). "Amoebapores, a family of membranolytic peptides from cytoplasmic granules of Entamoeba histolytica: isolation, primary structure, and pore formation in bacterial cytoplasmic membranes". Mol Microbiol. 14 (5): 895–904. PMID 7715451.
- ↑ Berninghausen O, Leippe M (1997). "Necrosis versus apoptosis as the mechanism of target cell death induced by Entamoeba histolytica". Infect Immun. 65 (9): 3615–21. PMC 175514. PMID 9284127.
- ↑ Seydel KB, Li E, Swanson PE, Stanley SL (1997). "Human intestinal epithelial cells produce proinflammatory cytokines in response to infection in a SCID mouse-human intestinal xenograft model of amebiasis". Infect Immun. 65 (5): 1631–9. PMC 175187. PMID 9125540.
- ↑ Que X, Reed SL (2000). "Cysteine proteinases and the pathogenesis of amebiasis". Clin Microbiol Rev. 13 (2): 196–206. PMC 100150. PMID 10755997.
- ↑ Salata RA, Pearson RD, Ravdin JI (1985). "Interaction of human leukocytes and Entamoeba histolytica. Killing of virulent amebae by the activated macrophage". J Clin Invest. 76 (2): 491–9. doi:10.1172/JCI111998. PMC 423849. PMID 2863284.
- ↑ Braga LL, Ninomiya H, McCoy JJ, Eacker S, Wiedmer T, Pham C; et al. (1992). "Inhibition of the complement membrane attack complex by the galactose-specific adhesion of Entamoeba histolytica". J Clin Invest. 90 (3): 1131–7. doi:10.1172/JCI115931. PMC 329975. PMID 1381719.
- ↑ Kelsall BL, Ravdin JI (1993). "Degradation of human IgA by Entamoeba histolytica". J Infect Dis. 168 (5): 1319–22. PMID 8228372.
- ↑ Reed SL, Keene WE, McKerrow JH, Gigli I (1989). "Cleavage of C3 by a neutral cysteine proteinase of Entamoeba histolytica". J Immunol. 143 (1): 189–95. PMID 2543700.