Amoebic liver abscess pathophysiology: Difference between revisions
No edit summary |
m (Bot: Removing from Primary care) |
||
| (35 intermediate revisions by 5 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
Ameoebic liver abscess is caused by a [[protozoan]] ''[[Entamoeba histolytica]]''. It is the most common extraintestinal manifestation of [[amoebiasis]]. The mode of transmission of ''[[Entamoeba histolytica]]'' include | [[Ameoebic liver abscess]] is caused by a [[protozoan]] ''[[Entamoeba histolytica]]''. It is the most common extraintestinal manifestation of [[amoebiasis]]. The mode of [[transmission]] of ''[[Entamoeba histolytica]]'' include [[fecal-oral route]] (ingestion of food and water contaminated with [[feces]] containing [[cysts]]), sexual transmission via oral-rectal route in [[Homosexual|homosexuals]], [[vector]] [[transmission]] via flies, cockroaches, and rodents.<ref name="pmid22763633">{{cite journal| author=Fletcher SM, Stark D, Harkness J, Ellis J| title=Enteric protozoa in the developed world: a public health perspective. | journal=Clin Microbiol Rev | year= 2012 | volume= 25 | issue= 3 | pages= 420-49 | pmid=22763633 | doi=10.1128/CMR.05038-11 | pmc=3416492 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22763633 }} </ref><ref name="pmid12660071">{{cite journal| author=Stanley SL| title=Amoebiasis. | journal=Lancet | year= 2003 | volume= 361 | issue= 9362 | pages= 1025-34 | pmid=12660071 | doi=10.1016/S0140-6736(03)12830-9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12660071 }} </ref> [[Hepatocyte]] programmed cell death induced by ''[[Entamoeba histolytica]]'' causes [[amoebic liver abscess]]. The [[infection]] is transmitted to [[liver]] by [[portal venous system]].<ref name="pmid473308">{{cite journal |vauthors=Aikat BK, Bhusnurmath SR, Pal AK, Chhuttani PN, Datta DV |title=The pathology and pathogenesis of fatal hepatic amoebiasis--A study based on 79 autopsy cases |journal=Trans. R. Soc. Trop. Med. Hyg. |volume=73 |issue=2 |pages=188–92 |year=1979 |pmid=473308 |doi= |url=}}</ref> | ||
==Pathophysiology== | ==Pathophysiology== | ||
*Amoebic liver abscess is the most common extraintestinal manifestation of [[amoebiasis]]. | *[[Amoebic liver abscess]] is the most common [[extraintestinal]] manifestation of [[amoebiasis]]. | ||
*There are two genetically different species of [[entamoeba]].<ref name="pmid12517854">{{cite journal| author=Gonin P, Trudel L| title=Detection and differentiation of Entamoeba histolytica and Entamoeba dispar isolates in clinical samples by PCR and enzyme-linked immunosorbent assay. | journal=J Clin Microbiol | year= 2003 | volume= 41 | issue= 1 | pages= 237-41 | pmid=12517854 | doi= | pmc=149615 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12517854 }} </ref> They are | *There are two genetically different species of [[entamoeba]].<ref name="pmid12517854">{{cite journal| author=Gonin P, Trudel L| title=Detection and differentiation of Entamoeba histolytica and Entamoeba dispar isolates in clinical samples by PCR and enzyme-linked immunosorbent assay. | journal=J Clin Microbiol | year= 2003 | volume= 41 | issue= 1 | pages= 237-41 | pmid=12517854 | doi= | pmc=149615 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12517854 }} </ref> They are | ||
:*''[[Entamoeba histolytica]]'' (the [[pathogen]]) | :*''[[Entamoeba histolytica]]'' (the [[pathogen]]) | ||
:*''[[Entamoeba|Entamoeba dispar]]'' (a [[commensal]]) | :*''[[Entamoeba|Entamoeba dispar]]'' (a [[commensal]]) | ||
*The mode of transmission of ''[[Entamoeba histolytica]]'' include:<ref name="pmid22763633">{{cite journal| author=Fletcher SM, Stark D, Harkness J, Ellis J| title=Enteric protozoa in the developed world: a public health perspective. | journal=Clin Microbiol Rev | year= 2012 | volume= 25 | issue= 3 | pages= 420-49 | pmid=22763633 | doi=10.1128/CMR.05038-11 | pmc=3416492 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22763633 }} </ref><ref name="pmid12660071">{{cite journal| author=Stanley SL| title=Amoebiasis. | journal=Lancet | year= 2003 | volume= 361 | issue= 9362 | pages= 1025-34 | pmid=12660071 | doi=10.1016/S0140-6736(03)12830-9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12660071 }} </ref> | *The mode of [[transmission]] of ''[[Entamoeba histolytica]]'' include:<ref name="pmid22763633">{{cite journal| author=Fletcher SM, Stark D, Harkness J, Ellis J| title=Enteric protozoa in the developed world: a public health perspective. | journal=Clin Microbiol Rev | year= 2012 | volume= 25 | issue= 3 | pages= 420-49 | pmid=22763633 | doi=10.1128/CMR.05038-11 | pmc=3416492 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22763633 }} </ref><ref name="pmid12660071">{{cite journal| author=Stanley SL| title=Amoebiasis. | journal=Lancet | year= 2003 | volume= 361 | issue= 9362 | pages= 1025-34 | pmid=12660071 | doi=10.1016/S0140-6736(03)12830-9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12660071 }} </ref> | ||
:*[[Fecal-oral route]] (ingestion of food and water contaminated with feces containing [[cysts]]) | :*[[Fecal-oral route]] (ingestion of food and water contaminated with [[feces]] containing [[cysts]]) | ||
:*Sexual transmission via [[oral-rectal route]] in [[homosexuals]] | :*Sexual [[transmission]] via [[oral-rectal route]] in [[Homosexual|homosexuals]] | ||
:*[[Vector]] transmission via flies, cockroaches, and rodents. | :*[[Vector]] [[transmission]] via flies, cockroaches, and rodents. | ||
*[[Hepatocyte]] programmed cell death induced by ''[[Entamoeba histolytica]]'' causes [[amoebic liver abscess]]. | *[[Hepatocyte]] [[programmed cell death]] induced by ''[[Entamoeba histolytica]]'' causes [[amoebic liver abscess]]. | ||
*The [[infection]] is transmitted to [[liver]] by [[portal venous system]].<ref name="pmid473308">{{cite journal |vauthors=Aikat BK, Bhusnurmath SR, Pal AK, Chhuttani PN, Datta DV |title=The pathology and pathogenesis of fatal hepatic amoebiasis--A study based on 79 autopsy cases |journal=Trans. R. Soc. Trop. Med. Hyg. |volume=73 |issue=2 |pages=188–92 |year=1979 |pmid=473308 |doi= |url=}}</ref> | *The [[infection]] is [[transmitted]] to [[liver]] by [[portal venous system]].<ref name="pmid473308">{{cite journal |vauthors=Aikat BK, Bhusnurmath SR, Pal AK, Chhuttani PN, Datta DV |title=The pathology and pathogenesis of fatal hepatic amoebiasis--A study based on 79 autopsy cases |journal=Trans. R. Soc. Trop. Med. Hyg. |volume=73 |issue=2 |pages=188–92 |year=1979 |pmid=473308 |doi= |url=}}</ref> | ||
*Clinical syndromes associated with ''[[Entamoeba histolytica]]'' [[infection]] | *Clinical syndromes associated with ''[[Entamoeba histolytica]]'' [[infection]] | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | A01| | | | | | | | | | | |A01='''Entamoeba histolytica'''}} | {{familytree | | | | | | | | | | | A01| | | | | | | | | | | |A01='''[[Entamoeba histolytica]]'''}} | ||
{{familytree | | | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} | {{familytree | | | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} | ||
{{familytree | | | | B01 | {{familytree |boxstyle=text-align: left; | | | | B01 | | | | | | | | | | | | B02 |B01='''Intestinal amoebiasis'''<br>• Asymptomatic [[cyst]] passers<br>• [[amoebic colitis|Acute amoebic colitis]]<br> • Mucosal disease<br> • Transmural disease<br> • Ulcerative post dysentric [[colitis]]<br>• [[Appendicitis]]<br>• Amoeboma<br>• Amoebic stricture|B02='''Extra intestinal amoebiasis'''<br>• [[Amoebic liver abscess]]<br>• [[Perforation]] and [[peritonitis]]<br>• Pleuropulmonary amoebiasis<br>• Amoebic [[pericarditis]]<br>• [[Cutaneous amoebiasis]]}} | ||
{{familytree/end}} | {{familytree/end}} | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
*After ingestion of contaminated food and water, ''[[Entamoeba histolytica]]'' trophozoites adhere to epithelial cells of colon, through the galactose/N-acetylgalactosamine specific lectin.<ref name="pmid12049210">{{cite journal| author=Mann BJ| title=Structure and function of the Entamoeba histolytica Gal/GalNAc lectin. | journal=Int Rev Cytol | year= 2002 | volume= 216 | issue= | pages= 59-80 | pmid=12049210 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12049210 }} </ref> | *After ingestion of contaminated food and water, ''[[Entamoeba histolytica]]'' [[trophozoites]] adhere to [[epithelial cells]] of [[colon]], through the galactose/N-acetylgalactosamine specific [[lectin]].<ref name="pmid12049210">{{cite journal| author=Mann BJ| title=Structure and function of the Entamoeba histolytica Gal/GalNAc lectin. | journal=Int Rev Cytol | year= 2002 | volume= 216 | issue= | pages= 59-80 | pmid=12049210 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12049210 }} </ref> | ||
*After adhesion, the parasite releases | *After [[adhesion]], the [[parasite]] releases [[proteinase|cysteine proteinases]] which digest [[extracellular]] matrix proteins. This facilitate [[trophozoite]] invasion into [[submucosa|submucosal tissue]] through amoebapore leading to activation of amoebic [[virulence]] program.<ref name="pmid7715451">{{cite journal| author=Leippe M, Andrä J, Nickel R, Tannich E, Müller-Eberhard HJ| title=Amoebapores, a family of membranolytic peptides from cytoplasmic granules of Entamoeba histolytica: isolation, primary structure, and pore formation in bacterial cytoplasmic membranes. | journal=Mol Microbiol | year= 1994 | volume= 14 | issue= 5 | pages= 895-904 | pmid=7715451 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7715451 }} </ref><ref name="pmid9284127">{{cite journal| author=Berninghausen O, Leippe M| title=Necrosis versus apoptosis as the mechanism of target cell death induced by Entamoeba histolytica. | journal=Infect Immun | year= 1997 | volume= 65 | issue= 9 | pages= 3615-21 | pmid=9284127 | doi= | pmc=175514 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9284127 }} </ref> | ||
*The extracellular amoebic cysteine proteinase converts pIL-1β (precursor interleukin 1β) to active IL-1β. The chemokines and cytokines released from epithelial cells attract macrophages and neutrophils to the site of infection.<ref name="pmid9125540">{{cite journal| author=Seydel KB, Li E, Swanson PE, Stanley SL| title=Human intestinal epithelial cells produce proinflammatory cytokines in response to infection in a SCID mouse-human intestinal xenograft model of amebiasis. | journal=Infect Immun | year= 1997 | volume= 65 | issue= 5 | pages= 1631-9 | pmid=9125540 | doi= | pmc=175187 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9125540 }} </ref> | *The [[extracellular]] amoebic cysteine [[proteinase]] converts pIL-1β (precursor interleukin 1β) to active IL-1β. The [[chemokines]] and [[cytokines]] released from epithelial cells attract [[macrophages]] and [[neutrophils]] to the site of [[infection]].<ref name="pmid9125540">{{cite journal| author=Seydel KB, Li E, Swanson PE, Stanley SL| title=Human intestinal epithelial cells produce proinflammatory cytokines in response to infection in a SCID mouse-human intestinal xenograft model of amebiasis. | journal=Infect Immun | year= 1997 | volume= 65 | issue= 5 | pages= 1631-9 | pmid=9125540 | doi= | pmc=175187 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9125540 }} </ref> | ||
*Neutrophils transmigrating to the epithelial surface facilitate ''[[Entamoeba histolytica|E histolytica]]'' invasion by creating channels. Cysteine proteinases digest extracellular matrix protein, causing epithelial cells to break from the villi, which also aid in the parasite's direct invasion into submucosal tissues.<ref name="pmid10755997">{{cite journal| author=Que X, Reed SL| title=Cysteine proteinases and the pathogenesis of amebiasis. | journal=Clin Microbiol Rev | year= 2000 | volume= 13 | issue= 2 | pages= 196-206 | pmid=10755997 | doi= | pmc=100150 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10755997 }} </ref> | *[[Neutrophils]] transmigrating to the epithelial surface facilitate ''[[Entamoeba histolytica|E histolytica]]'' invasion by creating channels. [[Proteinase|Cysteine proteinases]] digest extracellular matrix protein, causing [[epithelial cells]] to break from the [[villi]], which also aid in the [[parasite's]] direct invasion into [[submucosa|submucosal tissues]].<ref name="pmid10755997">{{cite journal| author=Que X, Reed SL| title=Cysteine proteinases and the pathogenesis of amebiasis. | journal=Clin Microbiol Rev | year= 2000 | volume= 13 | issue= 2 | pages= 196-206 | pmid=10755997 | doi= | pmc=100150 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10755997 }} </ref> | ||
*The mediators released by the neutrophils cause more damage to adjacent intestinal epithelial cells.<ref name="pmid2863284">{{cite journal| author=Salata RA, Pearson RD, Ravdin JI| title=Interaction of human leukocytes and Entamoeba histolytica. Killing of virulent amebae by the activated macrophage. | journal=J Clin Invest | year= 1985 | volume= 76 | issue= 2 | pages= 491-9 | pmid=2863284 | doi=10.1172/JCI111998 | pmc=423849 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2863284 }} </ref> | *The mediators released by the [[neutrophils]] cause more damage to adjacent intestinal [[epithelial cells]].<ref name="pmid2863284">{{cite journal| author=Salata RA, Pearson RD, Ravdin JI| title=Interaction of human leukocytes and Entamoeba histolytica. Killing of virulent amebae by the activated macrophage. | journal=J Clin Invest | year= 1985 | volume= 76 | issue= 2 | pages= 491-9 | pmid=2863284 | doi=10.1172/JCI111998 | pmc=423849 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2863284 }} </ref> | ||
*The trophozoites penetrate the mucosa, | *The [[trophozoites]] penetrate the [[mucosa]], [[submucosa]]l tissues and even into the [[portal circulation]] where they encounter additional host defenses, including [[complement system]]. | ||
*''[[ | *''[[Entamoeba histolytica|E. histolytica]]'' are covered by highly [[glycosylated]] and [[phosphorylated]] lipophosphoglycan which may serve as a physical barrier to [[complement]] components. The amoebic Gal/GalNAc [[lectin]] has a region with [[antigenic]] cross reactivity with [[CD59]] which protect [[trophozoites]] against [[lysis]].<ref name="pmid1381719">{{cite journal| author=Braga LL, Ninomiya H, McCoy JJ, Eacker S, Wiedmer T, Pham C et al.| title=Inhibition of the complement membrane attack complex by the galactose-specific adhesion of Entamoeba histolytica. | journal=J Clin Invest | year= 1992 | volume= 90 | issue= 3 | pages= 1131-7 | pmid=1381719 | doi=10.1172/JCI115931 | pmc=329975 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1381719 }} </ref> | ||
*The cysteine proteinases cleave and inactivate the anaphylatoxins C3a and C5a along with human IgA and IgG which provides further | *The [[cysteine]] [[Proteinase|proteinases]] cleave and inactivate the [[Anaphylatoxin|anaphylatoxins]] [[C3a]] and [[C5a]] along with human [[IgA]] and [[IgG]] which provides further defense against [[Immune response|host immune response]].<ref name="pmid8228372">{{cite journal| author=Kelsall BL, Ravdin JI| title=Degradation of human IgA by Entamoeba histolytica. | journal=J Infect Dis | year= 1993 | volume= 168 | issue= 5 | pages= 1319-22 | pmid=8228372 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8228372 }} </ref><ref name="pmid2543700">{{cite journal| author=Reed SL, Keene WE, McKerrow JH, Gigli I| title=Cleavage of C3 by a neutral cysteine proteinase of Entamoeba histolytica. | journal=J Immunol | year= 1989 | volume= 143 | issue= 1 | pages= 189-95 | pmid=2543700 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2543700 }} </ref> | ||
*The trophozoites which enter the liver through portal | *The [[trophozoites]] which enter the [[liver]] through [[portal circulation]] leading to [[apoptosis]] of [[liver]] cells and [[abscess]] formation. | ||
*Stages of abscess formation include: | *Stages of [[abscess]] formation include: | ||
:*Acute inflammation | :*[[Acute]] [[inflammation]] | ||
:*Granuloma formation | :*[[Granuloma]] formation | ||
:*Necrosis with necrotic abscess or periportal fibrosis | :*[[Necrosis]] with necrotic [[abscess]] or [[periportal]] [[fibrosis]] | ||
====Variants of amoebic liver abscesses==== | ====Variants of amoebic liver abscesses==== | ||
*Solitary lesions (30%-70%) are more common amoebic liver | *Solitary lesions (30%-70%) are more common [[amoebic liver abscess]]es and most commonly seen in [[Right lobe of liver|right lobe of the liver]]. | ||
*The right hepatic lobule is most commonly effected due to portal circulatory system of the right colon. | *The [[Right lobe of liver|right hepatic lobule]] is most commonly effected due to [[Portal circulation|portal circulatory system]] of the [[colon|right colon]]. | ||
{| class="wikitable" style="text-align: Top;" | {| class="wikitable" style="text-align: Top;" | ||
!Multiple liver abscesses | !Multiple liver abscesses | ||
!Left lobe abscess | ![[Left lobe of liver|Left lobe]] abscess | ||
!Compression lesions | !Compression lesions | ||
!Extension of the abscess | !Extension of the abscess | ||
| Line 52: | Line 52: | ||
* 15% of patients have multiple liver abscesses | * 15% of patients have multiple liver abscesses | ||
* Presenting features include: | * Presenting features include: | ||
:*Fever | :*[[Fever]] | ||
:* | :*[[Toxemia]] | ||
:*Encephalopathy | :*[[Encephalopathy]] | ||
:*Jaundice | :*[[Jaundice]] | ||
*The most common organisms that cause multiple liver abscesses are ''[[E.coli]]'' and ''[[Klebsiella]]'' | *The most common organisms that cause multiple liver [[abscesses]] are ''[[E.coli]]'' and ''[[Klebsiella]]'' | ||
*Multiple liver abscesses may cause right hepatic vein occlusion, | *Multiple liver abscesses may cause right hepatic vein occlusion, [[pylephlebitis]], and occlusion of [[portal vein]] radicals resulting in [[hepatic failure|acute hepatic failure]] and [[encephalopathy]]. | ||
| | | | ||
* 35% of patients with amoebic liver abscess present with left lobe abscess | *35% of patients with [[amoebic liver abscess]] present with left lobe [[abscess]] | ||
* Presenting features include: | *Presenting features include: | ||
:*Longer duration of symptoms (3-4 weeks) | :*Longer duration of symptoms (3-4 weeks) | ||
:*Fever | :*[[Fever]] | ||
:*Large epigastric mass (minimal movement with respiration) | :*Large [[epigastric]] mass (minimal movement with respiration) | ||
:* | :*[[Weight loss]] | ||
* Complications include: | *Complications include: | ||
:*Peritonitis | :*[[Peritonitis]] | ||
:* | :*[[Toxemia]] | ||
* Management includes: | * Management includes: | ||
Aspiration + anti-amoebic drugs | [[Aspiration]] + anti-amoebic drugs | ||
| | | | ||
* Compression lesions include posteriorly located right lobe abscess which compresses inferior | *Compression lesions include posteriorly located [[Right lobe of liver|right lobe]] abscess which compresses [[inferior vena cava]] or [[hepatic vein]] | ||
* Presenting features include: | *Presenting features include: | ||
Bilateral pedal edema | :*Bilateral [[pedal edema]] | ||
:*[[Ascites]] | |||
Ascites | :*Visible [[veins]] on anterior and posterior [[abdominal wall]] | ||
*Symptoms disappear after [[aspiration]] of [[abscess]] | |||
Visible veins on anterior and posterior abdominal wall | |||
Symptoms disappear after aspiration of abscess | |||
| | | | ||
* 7% of patients present perforated abscesses | *7% of patients present perforated abscesses | ||
* Rupture of abscess into the following | *Rupture of [[abscess]] into the following | ||
:* Perforation of the abscess into pleural cavity causes empyema thoracis | :*[[Perforation]] of the [[abscess]] into [[pleural cavity]] causes [[empyema thoracis]] | ||
:* Peritoneal cavity causes shock and peritonitis | :*[[Peritoneal cavity]] causes [[shock]] and [[peritonitis]] | ||
:* Colon and biliary tree | :*[[Colon]] and [[biliary tree]] | ||
|} | |} | ||
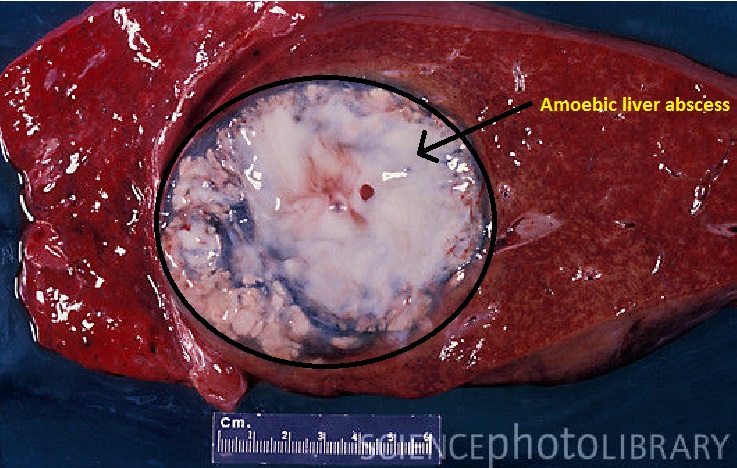
====Gross pathology==== | ====Gross pathology==== | ||
*The amoebic liver abscesses are well circumscribed regions which contain necrotic material (dead hepatocytes, liquefied cells and cellular debris) and the surrounding fibrinous border. | *The amoebic liver abscesses are well circumscribed regions which contain [[necrosis|necrotic]] material (dead [[hepatocytes]], liquefied cells and cellular debris) and the surrounding [[fibrinous]] border. | ||
*The adjacent liver parenchyma is usually normal. | *The adjacent liver [[parenchyma]] is usually normal. | ||
*The | *The [[abscess]]es are single or multiple. | ||
*The abscess cavity may be filled with chocolate colored pasty material (anchovy sauce-like). | *The [[abscess]] cavity may be filled with chocolate colored pasty material (anchovy sauce-like). | ||
[[File:Amoebic-Liver-abscess-Gross-specimen-of-liver-tissue-with-an-abscess-white3.jpg|500px]] | |||
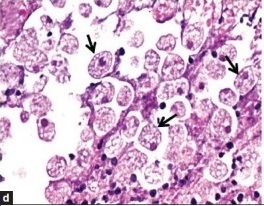
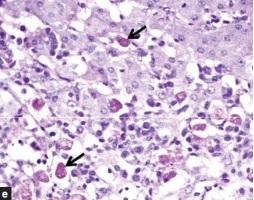
====Microscopic pathology==== | |||
*Multiple [[neutrophil|neutrophilic]] abscess with areas of [[necrosis]] are seen in the liver [[parenchyma]]. | |||
*A rim of [[connective tissue]], with few inflammatory cells and amoebic [[trophozoites]] are clustered in the [[fibrin]] at the junction of viable and [[necrosis|necrotic]] tissue. | |||
[[File:Microscopic_pathology.jpg|Amoebic liver abscess|300px]] | |||
[[File:Microscopic_pathology2.jpg|Amoebic liver abscess|300px]] | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Gastroenterology]] | |||
[[Category:Surgery]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Infectious disease]] | |||
[[Category:Hepatology]] | |||
Latest revision as of 20:23, 29 July 2020
|
Amoebic liver abscess Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Amoebic liver abscess pathophysiology On the Web |
|
American Roentgen Ray Society Images of Amoebic liver abscess pathophysiology |
|
Risk calculators and risk factors for Amoebic liver abscess pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Yamuna Kondapally, M.B.B.S[2]
Overview
Ameoebic liver abscess is caused by a protozoan Entamoeba histolytica. It is the most common extraintestinal manifestation of amoebiasis. The mode of transmission of Entamoeba histolytica include fecal-oral route (ingestion of food and water contaminated with feces containing cysts), sexual transmission via oral-rectal route in homosexuals, vector transmission via flies, cockroaches, and rodents.[1][2] Hepatocyte programmed cell death induced by Entamoeba histolytica causes amoebic liver abscess. The infection is transmitted to liver by portal venous system.[3]
Pathophysiology
- Amoebic liver abscess is the most common extraintestinal manifestation of amoebiasis.
- There are two genetically different species of entamoeba.[4] They are
- The mode of transmission of Entamoeba histolytica include:[1][2]
- Fecal-oral route (ingestion of food and water contaminated with feces containing cysts)
- Sexual transmission via oral-rectal route in homosexuals
- Vector transmission via flies, cockroaches, and rodents.
- Hepatocyte programmed cell death induced by Entamoeba histolytica causes amoebic liver abscess.
- The infection is transmitted to liver by portal venous system.[3]
- Clinical syndromes associated with Entamoeba histolytica infection
| Entamoeba histolytica | |||||||||||||||||||||||||||||||||||||||||||||||
| Intestinal amoebiasis • Asymptomatic cyst passers • Acute amoebic colitis • Mucosal disease • Transmural disease • Ulcerative post dysentric colitis • Appendicitis • Amoeboma • Amoebic stricture | Extra intestinal amoebiasis • Amoebic liver abscess • Perforation and peritonitis • Pleuropulmonary amoebiasis • Amoebic pericarditis • Cutaneous amoebiasis | ||||||||||||||||||||||||||||||||||||||||||||||
Pathogenesis
- After ingestion of contaminated food and water, Entamoeba histolytica trophozoites adhere to epithelial cells of colon, through the galactose/N-acetylgalactosamine specific lectin.[5]
- After adhesion, the parasite releases cysteine proteinases which digest extracellular matrix proteins. This facilitate trophozoite invasion into submucosal tissue through amoebapore leading to activation of amoebic virulence program.[6][7]
- The extracellular amoebic cysteine proteinase converts pIL-1β (precursor interleukin 1β) to active IL-1β. The chemokines and cytokines released from epithelial cells attract macrophages and neutrophils to the site of infection.[8]
- Neutrophils transmigrating to the epithelial surface facilitate E histolytica invasion by creating channels. Cysteine proteinases digest extracellular matrix protein, causing epithelial cells to break from the villi, which also aid in the parasite's direct invasion into submucosal tissues.[9]
- The mediators released by the neutrophils cause more damage to adjacent intestinal epithelial cells.[10]
- The trophozoites penetrate the mucosa, submucosal tissues and even into the portal circulation where they encounter additional host defenses, including complement system.
- E. histolytica are covered by highly glycosylated and phosphorylated lipophosphoglycan which may serve as a physical barrier to complement components. The amoebic Gal/GalNAc lectin has a region with antigenic cross reactivity with CD59 which protect trophozoites against lysis.[11]
- The cysteine proteinases cleave and inactivate the anaphylatoxins C3a and C5a along with human IgA and IgG which provides further defense against host immune response.[12][13]
- The trophozoites which enter the liver through portal circulation leading to apoptosis of liver cells and abscess formation.
- Stages of abscess formation include:
- Acute inflammation
- Granuloma formation
- Necrosis with necrotic abscess or periportal fibrosis
Variants of amoebic liver abscesses
- Solitary lesions (30%-70%) are more common amoebic liver abscesses and most commonly seen in right lobe of the liver.
- The right hepatic lobule is most commonly effected due to portal circulatory system of the right colon.
| Multiple liver abscesses | Left lobe abscess | Compression lesions | Extension of the abscess |
|---|---|---|---|
|
Aspiration + anti-amoebic drugs |
|
|
Gross pathology
- The amoebic liver abscesses are well circumscribed regions which contain necrotic material (dead hepatocytes, liquefied cells and cellular debris) and the surrounding fibrinous border.
- The adjacent liver parenchyma is usually normal.
- The abscesses are single or multiple.
- The abscess cavity may be filled with chocolate colored pasty material (anchovy sauce-like).
Microscopic pathology
- Multiple neutrophilic abscess with areas of necrosis are seen in the liver parenchyma.
- A rim of connective tissue, with few inflammatory cells and amoebic trophozoites are clustered in the fibrin at the junction of viable and necrotic tissue.
References
- ↑ 1.0 1.1 Fletcher SM, Stark D, Harkness J, Ellis J (2012). "Enteric protozoa in the developed world: a public health perspective". Clin Microbiol Rev. 25 (3): 420–49. doi:10.1128/CMR.05038-11. PMC 3416492. PMID 22763633.
- ↑ 2.0 2.1 Stanley SL (2003). "Amoebiasis". Lancet. 361 (9362): 1025–34. doi:10.1016/S0140-6736(03)12830-9. PMID 12660071.
- ↑ 3.0 3.1 Aikat BK, Bhusnurmath SR, Pal AK, Chhuttani PN, Datta DV (1979). "The pathology and pathogenesis of fatal hepatic amoebiasis--A study based on 79 autopsy cases". Trans. R. Soc. Trop. Med. Hyg. 73 (2): 188–92. PMID 473308.
- ↑ Gonin P, Trudel L (2003). "Detection and differentiation of Entamoeba histolytica and Entamoeba dispar isolates in clinical samples by PCR and enzyme-linked immunosorbent assay". J Clin Microbiol. 41 (1): 237–41. PMC 149615. PMID 12517854.
- ↑ Mann BJ (2002). "Structure and function of the Entamoeba histolytica Gal/GalNAc lectin". Int Rev Cytol. 216: 59–80. PMID 12049210.
- ↑ Leippe M, Andrä J, Nickel R, Tannich E, Müller-Eberhard HJ (1994). "Amoebapores, a family of membranolytic peptides from cytoplasmic granules of Entamoeba histolytica: isolation, primary structure, and pore formation in bacterial cytoplasmic membranes". Mol Microbiol. 14 (5): 895–904. PMID 7715451.
- ↑ Berninghausen O, Leippe M (1997). "Necrosis versus apoptosis as the mechanism of target cell death induced by Entamoeba histolytica". Infect Immun. 65 (9): 3615–21. PMC 175514. PMID 9284127.
- ↑ Seydel KB, Li E, Swanson PE, Stanley SL (1997). "Human intestinal epithelial cells produce proinflammatory cytokines in response to infection in a SCID mouse-human intestinal xenograft model of amebiasis". Infect Immun. 65 (5): 1631–9. PMC 175187. PMID 9125540.
- ↑ Que X, Reed SL (2000). "Cysteine proteinases and the pathogenesis of amebiasis". Clin Microbiol Rev. 13 (2): 196–206. PMC 100150. PMID 10755997.
- ↑ Salata RA, Pearson RD, Ravdin JI (1985). "Interaction of human leukocytes and Entamoeba histolytica. Killing of virulent amebae by the activated macrophage". J Clin Invest. 76 (2): 491–9. doi:10.1172/JCI111998. PMC 423849. PMID 2863284.
- ↑ Braga LL, Ninomiya H, McCoy JJ, Eacker S, Wiedmer T, Pham C; et al. (1992). "Inhibition of the complement membrane attack complex by the galactose-specific adhesion of Entamoeba histolytica". J Clin Invest. 90 (3): 1131–7. doi:10.1172/JCI115931. PMC 329975. PMID 1381719.
- ↑ Kelsall BL, Ravdin JI (1993). "Degradation of human IgA by Entamoeba histolytica". J Infect Dis. 168 (5): 1319–22. PMID 8228372.
- ↑ Reed SL, Keene WE, McKerrow JH, Gigli I (1989). "Cleavage of C3 by a neutral cysteine proteinase of Entamoeba histolytica". J Immunol. 143 (1): 189–95. PMID 2543700.