Addison's disease pathophysiology
| Title |
| https://https://www.youtube.com/watch?v=V6XcBp8EV7Q%7C350}} |
|
Addison's disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Addison's disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Addison's disease pathophysiology |
|
Risk calculators and risk factors for Addison's disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
The hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to release corticotropin (ACTH). ACTH travels via the blood to the adrenal gland, where it stimulates the release of cortisol. Cortisol is secreted by the cortex of the adrenal gland from a region called the zona fasciculata in response to ACTH. Elevated levels of cortisol exert negative feedback on the pituitary, which decreases the amount of ACTH released from the pituitary gland. Addison's disease results when the adrenal glands do not produce enough cortisol and aldosterone.
Normal Physiology of Adrenal Glands
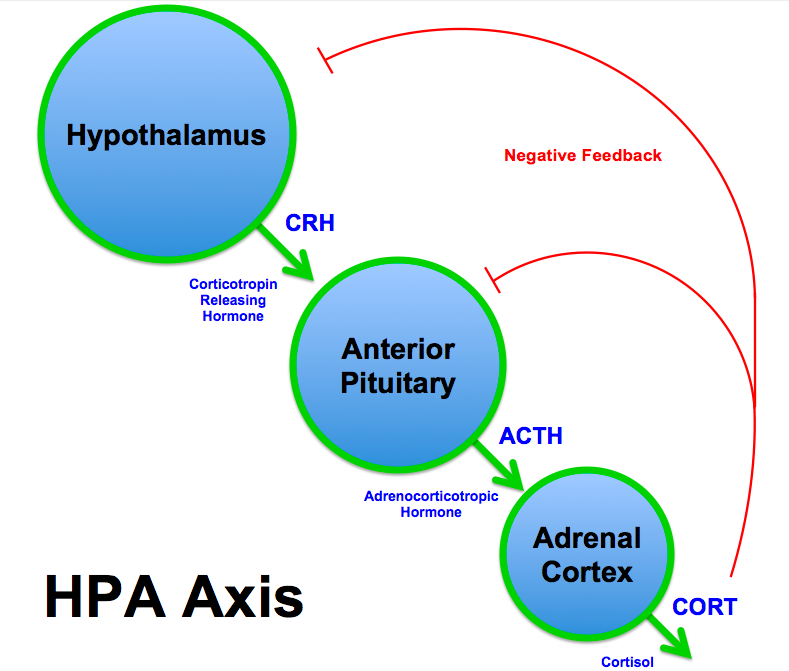
Hypothalamic–pituitary–adrenal axis
- The paraventricular nucleus of the hypothalamus secretes corticotropin-releasing hormone (CRH).
- CRH stimulates the anterior lobe of the pituitary gland, which leads to the release of adrenocorticotropic hormone (ACTH)
- ACTH, in turn, acts on the adrenal cortex, which produces glucocorticoid hormones (mainly cortisol in humans).
- Glucocorticoids, in addition to having physiological functions in the body, also have a negative feedback effect on the hypothalamus and pituitary (suppression of CRH and ACTH production).
Cortisol
| Harmone | Type of class | Function |
|---|---|---|
| Cortisol | Glucocorticoids |
|
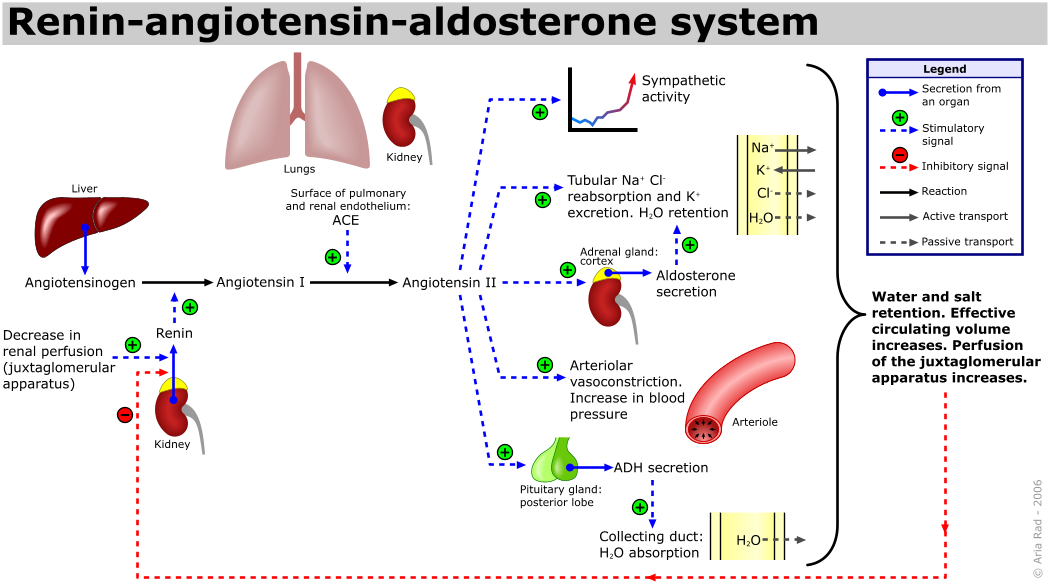
| Aldosterone | Mineralocorticoids |
 |
Pathophysiology
Addison's disease occurs when the adrenal glands do not produce enough cortisol and, in some cases, aldosterone. Adrenal insufficiency may arise due to insufficient release of cortisol from the adrenal glands. Insufficient cortisol secretion may be due to adrenal dysgenesis (the gland does not form adequately during development), impaired steroidogenesis (the gland is present but is biochemically unable to produce cortisol) or adrenal destruction (disease processes leading to the gland being damaged).
| Mechanism of adrenal insufficiency | Definition | Pathophysiology |
|---|---|---|
| Adrenal dysgenesis | Gland does not form adequately during development |
|
| Impaired steroidogenesis |
|
|
| Adrenal destruction |
|
|
Genetics
- Hereditary factors sometimes play a key role in the development of autoimmune adrenal insufficiency.[1]
- Common genetic conditions associated with addison's diseases include:
- Familial glucocorticoid insufficiency may be associated with a recessive gene pattern.
- Adrenomyeloneuropathy is known to be X-linked
- Addison disease is associated with a variety of autoimmune conditions that have been linked to genetic factors.
- Patients with autoimmune polyglandular failure might develop diabetes mellitus, pernicious anemia, and hypothyroidism secondary to antibodies which develop in adrenal glands.
Associated conditions
Addison's disease is commonly seen associated with conditions such as:
- Autoimmune hypoparathyroidism resulting in hypocalcemia
- Vitiligo
- Premature ovarian failure
- Pernicious anemia
- Myasthenia gravis
- Chronic candidiasis
- Sjögren syndrome
- Chronic active hepatitis
- Diabetes mellitus type 1
- Hypothyroidism
- Hashimoto thyroiditis
- Graves hyperthyroidism
- Adrenoleukodystrophy
References
- ↑ Michels AW, Eisenbarth GS (2010). "Immunologic endocrine disorders". J. Allergy Clin. Immunol. 125 (2 Suppl 2): S226–37. doi:10.1016/j.jaci.2009.09.053. PMC 2835296. PMID 20176260.