|
|
| Line 18: |
Line 18: |
| {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} |
|
| |
|
| == Complete Differential Diagnosis of Acute Renal Failure==
| |
|
| |
|
| ===Common Causes===
| |
| Acute renal failure is usually categorised (as in the flowchart below) according to ''pre-renal, renal'' and ''post-renal'' causes.
| |
| {{familytree/start}}
| |
| {{familytree | | | | | | | | | A01 | | | | | |A01=Acute Renal<br>Failure}}
| |
| {{familytree | | | | |,|-|-|-|-|+|-|-|-|-|.| |}}
| |
| {{familytree | | | | B01 | | | B02 | | | B03|B01=Pre-renal|B02=Renal|B03=Post-renal }}
| |
| {{familytree/end}}
| |
|
| |
| * ''Pre-renal'' (causes in the blood supply):
| |
| ** [[hypovolemia]] (decreased blood volume), usually from [[Shock (medical)|shock]] or [[dehydration]] and fluid loss or excessive [[diuretic]]s use.
| |
| ** [[hepatorenal syndrome]] in which renal [[perfusion]] is compromised in [[liver failure]]
| |
| ** vascular problems, such as [[atheroembolic disease]] and [[renal vein thrombosis]] (which can occur as a complication of the [[nephrotic syndrome]])
| |
|
| |
| * ''Renal'' (damage to the kidney itself):
| |
| ** [[infection]] usually [[sepsis]] (systemic inflammation due to infection),rarely of the kidney itself, termed [[pyelonephritis]]
| |
| ** [[toxin]]s or [[medication]] (e.g. some [[NSAID]]s, [[aminoglycoside]] [[antibiotics]], [[iodinated contrast]], [[Lithium salt|lithium]])
| |
| ** [[rhabdomyolysis]] (breakdown of [[muscle]] tissue) - the resultant release of [[myoglobin]] in the [[blood]] affects the kidney; it can be caused by [[injury]] (especially crush injury and extensive [[blunt trauma]]), [[statin]]s, [[stimulant]]s and some other drugs
| |
| ** [[hemolysis]] (breakdown of [[red blood cell]]s) - the [[hemoglobin]] damages the [[tubules]]; it may be caused by various conditions such as [[sickle-cell disease]], and [[lupus erythematosus]]
| |
| ** [[multiple myeloma]], either due to [[hypercalcemia]] or "cast nephropathy" (multiple myeloma can also cause [[chronic renal failure]] by a different mechanism)
| |
| ** acute [[glomerulonephritis]] which may be due to a variety of causes, such as [[anti glomerular basement membrane disease]]/[[Goodpasture's syndrome]], [[Wegener's granulomatosis]] or acute [[lupus nephritis]] with [[systemic lupus erythematosus]]
| |
|
| |
| * ''Post-renal'' (obstructive causes in the urinary tract) due to:
| |
| ** [[medication]] interfering with normal bladder emptying.
| |
| ** [[benign prostatic hypertrophy]] or [[prostate cancer]].
| |
| ** [[kidney stones]].
| |
| ** due to abdominal malignancy (e.g. [[ovarian cancer]], [[colorectal cancer]]).
| |
| ** obstructed urinary catheter.
| |
|
| |
| ===Prerenal Causes===
| |
|
| |
| *[[Acute pancreatitis]]
| |
| *[[Aortic aneurysm]]
| |
| *[[Cirrhosis]]
| |
| *[[Dehydration]]
| |
| *[[Drug|Drugs]] such as [[diuretics]]
| |
| *[[Gastrointestinal bleeding]]
| |
| *[[Hemolysis]]
| |
| *[[Hepatorenal syndrome]]
| |
| *[[Hypovolemia]]
| |
| *[[Metrorrhagia]]
| |
| *[[Nephrotic syndrome]]
| |
| *[[Peritonitis]]
| |
| *[[Pre-eclampsia]]
| |
| *[[Rhabdomyolysis]]
| |
| *[[Renal artery stenosis]]
| |
| *[[Renal vein thrombosis]]
| |
| *Severe [[sodium]] and [[chloride]] loss
| |
| *[[Shock]] of various orgins
| |
| *[[Surgery]]
| |
| *[[Therapy]] with [[ACE inhibitors]]
| |
| *[[Trauma]]
| |
| *[[Water]] / [[electrolyte]] loss
| |
|
| |
| ===Renal Causes===
| |
|
| |
| *[[Arteriosclerosis]] of the [[renal arteries]]
| |
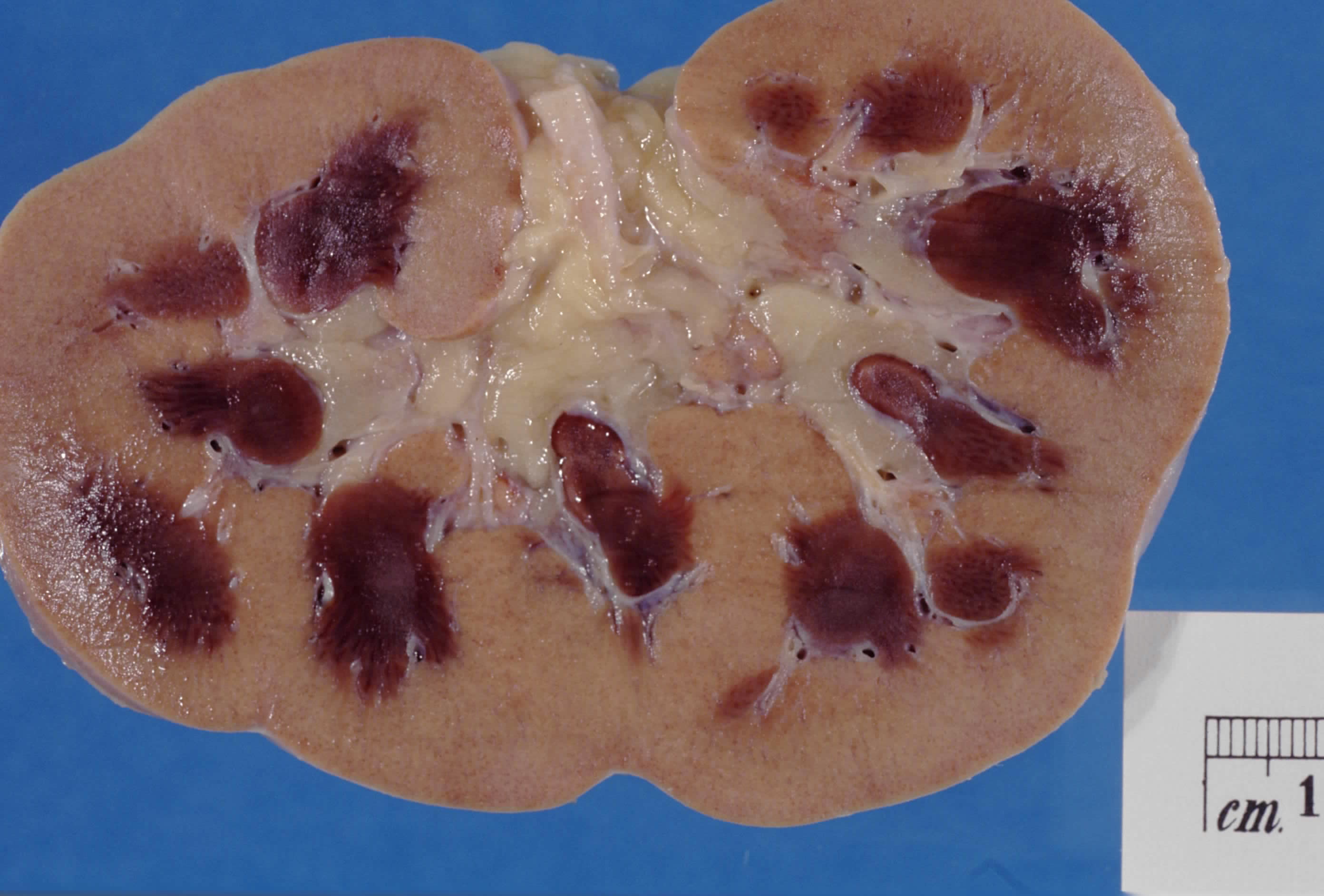
| *Bilateral [[renal cortex|renal cortical]] [[necrosis]]
| |
| *[[Glomerulonephritis]]
| |
| *[[Hemolytic-Uremic Syndrome]]
| |
| *[[Kidney]] [[transplant rejection]]
| |
| *[[Interstitial nephritis]]
| |
| *[[Malignant hypertension]]
| |
| *[[Occlusion]] of the [[renal arteries]]
| |
| *[[Polyarteritis nodosa]] [[PAN]]
| |
| *[[Pyelonephritis]]
| |
| *[[Scleroderma]]
| |
| *[[Thrombotic thrombocytopenic purpura]]
| |
| *[[Tubulointerstitial renal failure]]
| |
| *[[Vasculitis]]
| |
|
| |
| ===Postrenal Causes===
| |
|
| |
| *[[Bladder stone]]
| |
| *[[Bladder carcinoma]]
| |
| *[[Bladder infection]]
| |
| *Bladder [[neuropathy]]
| |
| * [[Colorectal cancer]]
| |
| *[[Multiple sclerosis]]
| |
| *[[Neurosyphillis]]
| |
| * [[Ovarian cancer]]
| |
| *[[Phimosis]]
| |
| *[[Prostatic hypertrophy]]
| |
| *[[Prostatitis]]
| |
| *Ruptured [[ureter]]
| |
| *[[Spinal cord stenosis]]
| |
| *[[Syringomyelia]]
| |
| *[[Tabes dorsalis]]
| |
| *[[Trabeculated bladder]]
| |
| *[[Urethra]]l [[atresia]]
| |
| *[[Urethra]]l [[trauma]]
| |
| *[[Urethra]]l [[stricture]]
| |
|
| |
| ==Diagnosis==
| |
| Renal failure is generally diagnosed either when [[creatinine]] or [[blood urea nitrogen]] tests are markedly elevated in an ill patient, especially when oliguria is present. Previous measurements of renal function may offer comparison, which is especially important if a patient is known to have [[chronic renal failure]] as well. If the cause is not apparent, a large amount of [[blood test]]s and examination of a [[urine]] specimen is typically performed to elucidate the cause of acute renal failure, [[medical ultrasonography]] of the renal tract is essential to rule out obstruction of the urinary tract.
| |
|
| |
| Consensus criteria<ref>Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004 Aug;8(4):R204-12. Epub 2004 May 24. PMID 15312219 [http://ccforum.com/content/8/4/R204 Full Text]. [http://ccforum.com/content/8/4/r204/figure/F1 Criteria for ARF (Figure)].</ref><ref>Lameire N, Van Biesen W, Vanholder R. ''Acute renal failure.'' [[The Lancet|Lancet]] 2005;365:417-30. PMID 15680458.</ref> for the diagnosis of ARF are:
| |
| * Risk: serum creatinine increased 1.5 times OR urine production of <0.5 ml/kg body weight for 6 hours
| |
| * Injury: creatinine 2.0 times OR urine production <0.5 ml/kg for 12 h
| |
| * Failure: creatinine 3.0 times OR creatinine >355 μmol/l (with a rise of >44) or urine output below 0.3 ml/kg for 24 h
| |
| * Loss: persistent ARF or more than four weeks complete loss of kidney function
| |
|
| |
| Kidney [[biopsy]] may be performed in the setting of acute renal failure, to provide a definitive diagnosis and sometimes an idea of the [[prognosis]], unless the cause is clear and appropriate screening investigations are reassuringly negative.
| |
|
| |
| ==Treatment==
| |
|
| |
| Acute renal failure may be reversible if treated promptly and appropriately. Resuscitation to normotension and a normal [[cardiac output]] is key. The main interventions are monitoring fluid intake and output as closely as possible; insertion of a [[Urinary catheterization|urinary catheter]] is useful for monitoring urine output as well as relieving possible bladder outlet obstruction, such as with an enlarged prostate. In the absence of fluid overload, administering [[intravenous fluid]]s is typically the first step to improve renal function. Fluid administration may be monitored with the use of a [[central venous catheter]] to avoid over- or under-replacement of fluid. If the cause is obstruction of the urinary tract, relief of the obstruction (with a [[nephrostomy]] or [[urinary catheter]]) may be necessary. [[Metabolic acidosis]] and [[hyperkalemia]], the two most serious biochemical manifestations of acute renal failure, may require medical treatment with [[sodium bicarbonate]] administration and antihyperkalemic measures, unless [[dialysis]] is required.
| |
|
| |
| Should hypotension prove a persistent problem in the fluid replete patient, [[inotrope]]s such as [[norepinephrine]] and/or [[dobutamine]] may be given to improve [[cardiac output]] and hence renal perfusion. While a useful pressor, there is no evidence to suggest that [[dopamine]] is of any specific benefit,<ref>{{cite journal |author=Holmes CL, Walley KR |title=Bad medicine: low-dose dopamine in the ICU |journal=Chest |volume=123 |issue=4 |pages=1266–75 |year=2003 |pmid=12684320|doi=10.1378/chest.123.4.1266}}</ref> and at least a suggestion of possible harm. A [[Swan-Ganz catheter]] may be used, to measure ''pulmonary artery occlusion pressure'' to provide a guide to left atrial pressure (and thus left heart function) as a target for inotropic support.
| |
|
| |
| The use of [[diuretics]] such as [[furosemide]], while widespread and sometimes convenient in ameliorating fluid overload, does not reduce the risk of complications and death.<ref>{{cite journal |author=Uchino S, Doig GS, Bellomo R, ''et al'' |title=Diuretics and mortality in acute renal failure |journal=Crit. Care Med. |volume=32 |issue=8 |pages=1669–77 |year=2004 |pmid=15286542|doi=10.1097/01.CCM.0000132892.51063.2F}}</ref> In practice, diuretics may simply mask things, making it more difficult to judge the adequacy of resuscitation.
| |
|
| |
| Lack of improvement with fluid resuscitation, therapy-resistant hyperkalemia, metabolic acidosis, or fluid overload may necessitate artificial support in the form of [[dialysis]] or [[hemofiltration]]. Depending on the cause, a proportion of patients will never regain full renal function, thus having [[end stage renal failure]] requiring lifelong [[dialysis]] or a [[kidney transplant]].
| |
|
| |
| ==History==
| |
| Before the advancement of modern medicine, acute renal failure might be referred to as uremic poisoning. [[Uremia]] was the term used to describe the contamination of the [[blood]] with [[urine]]. Starting around 1847 this term was used to describe reduced urine output, now known as [[oliguria]], which was thought to be caused by the urine's mixing with the blood instead of being voided through the [[urethra]].
| |
|
| |
| Acute renal failure due to [[acute tubular necrosis]] (ATN) was recognised in the 1940s in the United Kingdom, where crush victims during the Battle of Britain developed patchy necrosis of renal tubules, leading to a sudden decrease in renal function.<ref>{{cite journal |author=Bywaters EG, Beall D |title=Crush injuries with impairment of renal function. |journal=[[British Medical Journal|Br Med J]] |volume= |issue=1 |pages=427-32 |year=1941 |pmid=9527411 |doi= |url=http://jasn.asnjournals.org/cgi/pmidlookup?view=long&pmid=9527411}}</ref> During the Korean and Vietnam wars, the incidence of ARF decreased due to better acute management and intravenous infusion of fluids.<ref>{{cite journal |author=Schrier RW, Wang W, Poole B, Mitra A |title=Acute renal failure: definitions, diagnosis, pathogenesis, and therapy |journal=J. Clin. Invest. |volume=114 |issue=1 |pages=5–14 |year=2004 |pmid=15232604 |pmc=437979 |doi=10.1172/JCI22353 |url=}}</ref>
| |
|
| |
|
| ==Acute Renal Failure Videos== | | ==Acute Renal Failure Videos== |