Gastroesophageal reflux disease
| Gastroesophageal reflux disease | |
| ICD-10 | K21 |
|---|---|
| ICD-9 | 530.81 |
| OMIM | 109350 |
| DiseasesDB | 23596 |
| MeSH | D005764 |
|
Gastroesophageal reflux disease Microchapters |
|
Differentiating Gastroesophageal Reflux Disease from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gastroesophageal reflux disease On the Web |
|
American Roentgen Ray Society Images of Gastroesophageal reflux disease |
|
Directions to Hospitals Treating Gastroesophageal reflux disease |
|
Risk calculators and risk factors for Gastroesophageal reflux disease |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: GERD, GORD, gastroesophageal reflux, oesophageal reflux, peptic esophagitis, esophageal reflux
Diagnosis
Symptoms
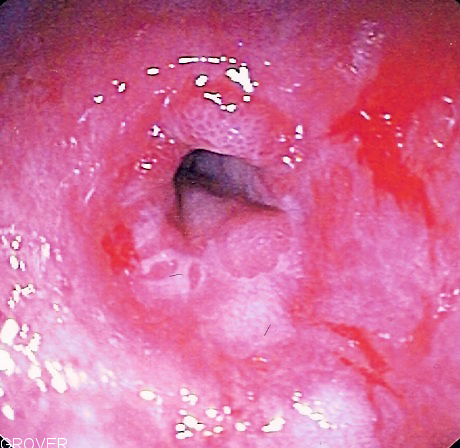
Useful investigations may include barium swallow X-rays, esophageal manometry, 24 hour esophageal pH monitoring and Esophagogastroduodenoscopy (EGD). In general, an EGD is done when the patient does not respond well to treatment, or has alarm symptoms including: dysphagia, anemia, blood in the stool (detected chemically), wheezing, weight loss, or voice changes. Some physicians advocate once-in-a-lifetime endoscopy for patients with longstanding GERD, to evaluate the possible presence of Barrett's esophagus, a precursor lesion for esophageal adenocarcinoma.
Esophagogastroduodenoscopy (EGD) (a form of endoscopy) involves insertion of a thin scope through the mouth and throat into the esophagus and stomach (often while the patient is sedated) in order to assess the internal surfaces of the esophagus, stomach, and duodenum.
Biopsies can be performed during gastroscopy and these may show:
- Edema and basal hyperplasia (non-specific inflammatory changes)
- Lymphocytic inflammation (non-specific)
- Neutrophilic inflammation (usually due to reflux or Helicobacter gastritis)
- Eosinophilic inflammation (usually due to reflux)
- Goblet cell intestinal metaplasia or Barretts esophagus.
- Elongation of the papillae
- Thinning of the squamous cell layer
- Dysplasia or pre-cancer.
- Carcinoma.
Causes
- Hereditary sensory and autonomic neuropathy type 1B
- Systemic sclerosis
- Autonomic neuropathy
- Esophageal achalasia
- Hiatus hernia
- Pharyngeal pouch
- Another paradoxical cause of GERD-like symptoms is not enough stomach acid (hypochlorhydria). The valve that empties the stomach into the intestines is triggered by acidity. If there is not enough acid, this valve does not open and the stomach contents are churned up into the esophagus. However, there is still enough acidity to irritate the esophagus.
- Hiatus hernia, which increases the likelihood of GERD due to mechanical and motility factors[1]
- Obesity: increasing body mass index is associated with more severe GERD[2]
- Zollinger-Ellison syndrome, which can be present with increased gastric acidity due to gastrin production
- Hypercalcemia, which can increase gastrin production, leading to increased acidity
- Scleroderma and systemic sclerosis, which can feature esophageal dysmotility
Treatment
The rubric "lifestyle modifications" is the term physicians use when recommending non-drug GERD treatments. A 2006 review suggested that evidence for most dietary interventions is anecdotal; only weight loss and elevating the head of the bed were supported by evidence[3]. A subsequent randomized crossover study showed benefit by avoiding eating two hours before bed.[1]
Foods
Certain foods and lifestyle are considered to promote gastroesophageal reflux:
- Coffee, alcohol, and excessive amounts of Vitamin C supplements stimulate gastric acid secretion. Taking these before bedtime especially can cause evening reflux. (Although a study published in 2006 by Stanford University researchers disputes the effect of coffee, acidic, spicy foods etc. as a myth.[3])
- Antacids based on calcium carbonate (but not aluminum hydroxide) were found to actually increase the acidity of the stomach. However, all antacids reduced acidity in the lower esophagus, so the net effect on GERD symptoms may still be positive.[4].
- Foods high in fats and smoking reduce lower esophageal sphincter competence, so avoiding these tends to help. Fat also delays stomach emptying.
- Eating shortly before bedtime (For clinical purposes, this usually means 2-3 hours before going to bed).
- Large meals. Having more but smaller meals reduces GERD risk, as it means there is less food in the stomach at any one time.
- Soda or pop (regular or diet).
- Chocolate and peppermint.
- Acidic foods, such as oranges and tomatoes.
- Cruciferous vegetables: onions, cabbage, cauliflower, broccoli, spinach, brussel sprouts.
- Milk and milk-based products contain calcium and fat, and should be avoided before bedtime.
Positional therapy
Sleeping on one's left side has been shown to drastically reduce nighttime reflux episodes in patients.[5].
Elevating the head of the bed is also effective. When combining drug therapy, food avoidance before bedtime, and elevation of the head of the bed, over 95% of patients will have complete relief. Additional conservative measures may be considered if there is incomplete relief. Another approach is to apply all conservative measures for maximum response. A meta-analysis suggested that elevating the head of bed is an effective therapy, although this conclusion was only supported by nonrandomized studies [3].
Elevating the head of the bed can be done by using various items: plastic or wooden bed risers that support bed posts or legs, a bed wedge pillow, or a wedge or an inflatable mattress lifter that fits in between mattress and box spring. The height of the elevation is critical and must be at least 6 to 8 inches (15 to 20 cm) in order to be at least minimally effective to prevent the backflow of gastric fluids. It should be noted that some innerspring mattresses do not work well when inclined and tend to cause back pain, thus foam based mattresses or futons are to be preferred. Some report relief from back pain by sleeping with one leg bent at the knee, alternating legs. Moreover, some use higher degrees of incline than provided by the commonly suggested 6 to 8 inches (15 to 20 cm) and claim greater success.
Drug treatment
A number of drugs are registered for GERD treatment, and they are among the most-often-prescribed forms of medication in most Western countries. They can be used in combination with other drugs, although some antacids can interfere with the function of other drugs:
- Proton pump inhibitors are the most effective in reducing gastric acid secretion. These drugs stop acid secretion at the source of acid production, i.e., the proton pump.
- Antacids before meals or symptomatically after symptoms begin can reduce gastric acidity (increase pH).
- Alginic acid (Gaviscon) may coat the mucosa as well as increase pH and decrease reflux. A meta-analysis of randomized controlled trials suggests alginic acid may be the most effective of non-prescription treatments with a number needed to treat of 4 [6].
- Gastric H2 receptor blockers such as ranitidine or famotidine can reduce gastric secretion of acid. These drugs are technically antihistamines. They relieve complaints in about 50% of all GERD patients. Compared to placebo (which also is associated with symptom improvement), they have a number needed to treat of eight (8) [6].
- Prokinetics strengthen the LES and speed up gastric emptying. Cisapride, a member of this class, was withdrawn from the market for causing Long QT syndrome.
- Sucralfate (Carafate®) is also useful as an adjunct in helping to heal and prevent esophageal damage caused by GERD, however it must be taken several times daily and at least two (2) hours apart from meals and medications.
Posture and GERD
In adults, a slouched posture is an important factor contributing to GERD. With a slouched posture there is no straight path between the stomach and esophagus; muscles around the esophagus go into a spasm. Gas and acidity get blocked in the spasm, causing coughing and other asthma-like symptoms. A meta-analysis suggested that elevating the head of the bed is an effective therapy, although this conclusion was only supported by nonrandomized studies.[3]
Surgical treatment
The standard surgical treatment, sometimes preferred over longtime use of medication, is the Nissen fundoplication. The upper part of the stomach is wrapped around the LES to strengthen the sphincter and prevent acid reflux and to repair a hiatal hernia. The procedure is often done laparoscopically.[7]
An obsolete treatment is vagotomy ("highly selective vagotomy"), the surgical removal of vagus nerve branches that innervate the stomach lining. This treatment has been largely replaced by medication.
Endoluminal fundoplication
In June 2006 EndoGastric Solutions introduced EsophyX ELF in the Europe Union as an alternative to surgical and pharmaceutical approaches for GERD treatment. EsophyX ELF is intended to deliver similar benefits as the time-proven laparoscopic fundoplication procedures, by reducing hiatal hernia, recreating the Angle of His, and creating a GastroEsophageal Valve (GEV). The key differences are that EsophyX ELF is an endoscopic non-invasive procedure that is performed transorally (through the mouth), does not require incisions, and does not dissect any part of the natural anatomy.
Previous endoluminal treatments focused predominantly on the LES. However, failure to effectively treat reflux long-term with endoluminal therapies that focused only on the Lower Esophageal Sphincter (LES) combined with the fact that surgical approaches like Nissen fundoplication recreate the GEV and have excellent long-term efficacy, has led to an awareness that the GEV is probably the most powerful component of the Anti-Reflux Barrier. The device has been designed to deploy multiple tissue fasteners to create a robust and durable valve and is intended to restore the geometry of the GastroEsophageal Junction and recreate the natural, unidirectional valve mechanism necessary to prevent GERD. EsophyX ELF has recently been cleared by the US FDA and is now available in the U.S.
Other treatments
In 2000 , the U.S. Food and Drug Administration (FDA) approved two endoscopic devices to treat chronic heartburn. One system, Endocinch, puts stitches in the LES to create little pleats that help strengthen the muscle. Another, the Stretta Procedure, uses electrodes to apply radio frequency energy to the LES. The long term outcomes of both procedures compared to a Nissen fundoplication are still being determined.
Subsequently the NDO Surgical Plicator was FDA cleared for the endoscopic GERD treatment. The Plicator creates a plication, or fold, of tissue near the gastroesophageal junction, and fixates the plication with a suture-based implant. The Plicator is currently marketed by NDO Surgical, Inc. [2].
Another treatment that involved injection of a solution during endoscopy into the lower esophageal wall was available for about one year ending in late 2005. It was marketed under the name Enteryx. It was removed from the market due to several reports of complications from misplaced injections.
Barrett's esophagus
Barrett's esophagus, a type of dysplasia, is a precursor high-grade dysplasia, which is in turn a precursor condition for carcinoma. The risk of progression from Barrett's to dysplasia is uncertain but is estimated to include 0.1% to 0.5% of cases, and has probably been exaggerated in the past. Due to the risk of chronic heartburn progressing to Barrett's, EGD every 5 years is recommended for patients with chronic heartburn, or who take drugs for chronic GERD.
References
- ↑ 1.0 1.1 Piesman M, Hwang I, Maydonovitch C, Wong RK (2007). "Nocturnal reflux episodes following the administration of a standardized meal. Does timing matter?". Am. J. Gastroenterol. 102 (10): 2128–2134. doi:10.1111/j.1572-0241.2007.01348.x. PMID 17573791.
- ↑ Ayazi S, Crookes P, Peyre C, (2007). "Objective documentation of the link between gastroesophageal reflux disease and obesity". Am. J. Gastroenterol. 102 (S): 138–139.
- ↑ 3.0 3.1 3.2 3.3 Kaltenbach T, Crockett S, Gerson LB (2006). "Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach". Arch. Intern. Med. 166 (9): 965–71. doi:10.1001/archinte.166.9.965. PMID 16682569.
- ↑ Decktor DL, Robinson M, Maton PN, Lanza FL, Gottlieb S. Effects of Aluminum/Magnesium Hydroxide and Calcium Carbonate on Esophageal and Gastric pH in Subjects with Heartburn. Am J Ther 1995;2:546-552. PMID 11854825.
- ↑ Khoury RM, Camacho-Lobato L, Katz PO, Mohiuddin MA, Castell DO. Influence of spontaneous sleep positions on nighttime recumbent reflux in patients with gastroesophageal reflux disease. Am J Gastroenterol 1999;94:2069-73. PMID 10445529.
- ↑ 6.0 6.1 Tran T, Lowry A, El-Serag H (2007). "Meta-analysis: the efficacy of over-the-counter gastro-oesophageal reflux disease drugs". Aliment Pharmacol Ther. 25 (2): 143–53. doi:10.1111/j.1365-2036.2006.03135.x. PMID 17229239.
- ↑ Abbas A, Deschamps C, Cassivi SD; et al. (2004). "The role of laparoscopic fundoplication in Barrett's esophagus". Annals of Thoracic Surgery. 77 (2): 393–396. PMID 14759403.
External links
- GERD patient information page at NIH
- KidsHealth GERD Information for Kids
- Mayo Clinic review of diagnosis and treatment options
- Overview at Cleveland Clinic
de:Refluxösophagitis it:Malattia da reflusso gastroesofageo no:Gastroøsofageal refluks sv:Gastroesofageal refluxsjukdom