Mastitis pathophysiology
|
Mastitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Mastitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Mastitis pathophysiology |
|
Risk calculators and risk factors for Mastitis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Prince Tano Djan, BSc, MBChB [2]
Overview
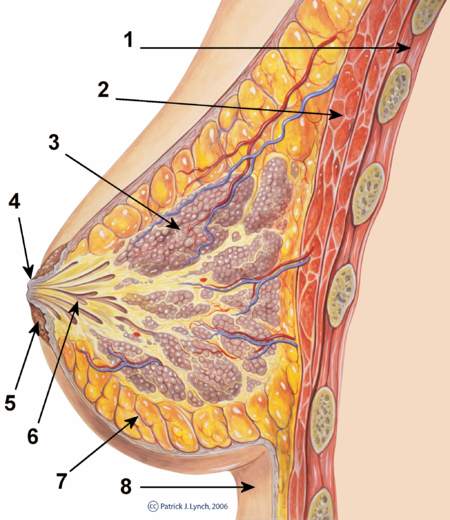
Most clinically significant cases of non-puerperal mastitis start as inflammation of the ductal and lobular system (galactophoritis) and possibly the immediate surrounding tissue (refer to the image below). Development of non-puerperal mastitis is the result of secretory stasis whereas puerperal mastitis occurs when bacteria, often from patients skin or the baby's mouth/nostrils,[1] enters a milk duct through a crack in the nipple.
-
Cross-section of the breast: 1) Chest wall, 2) Pectoralis muscles, 3) Lobules, 4) Nipple, 5) Areola, 6) Milk duct, 7) Fatty tissue and 8) Skin
-
Surface anatomy of the breast
Pathophysiology
Non-puerperal Mastitis: Pathogenesis
Most clinically significant cases of non-puerperal mastitis start as inflammation of the ductal and lobular system (galactophoritis) and possibly the immediate surrounding tissue. Development of puerperal mastitis occurs when bacteria, often from patients skin or the baby's mouth/nostrils,[2] enters a milk duct through a crack in the nipple.
Development of non-puerperal mastitis is the result of secretory stasis in about 80% of cases. The retained secretions can get infected or lead to inflammation by causing mechanical injury leading to leakage of the lactiferous ducts. Autoimmune reaction to the secretions may also be a factor.
Peurperal Mastitis: Pathogenesis
Development of Peurperal mastitis occurs when bacteria, often from patients skin or the baby's mouth/nostrils [3] enters a milk duct through a crack in the nipple.
Several mechanisms are thought to lead to the pathogenesis of mastitis as shown below:
- Secretory disease or galactorrhea.
- Changes in permeability of lactiferous ducts (retention syndrome).
- Blockage of lactiferous ducts, for example duct plugging caused by squamous metaplasia of lactiferous ducts.
- Trauma, injury.
- Mechanical irritation caused by retention syndrome or Fibrocystic Condition.
- Infection.
- Autoimmune reaction to luminal fluid.
Approximately a quarter of patients may be hyperprolactinemic. There have been strong association with fibrocystic condition and thyroid conditions. Up to half of patients may experience transient hyperprolactinemia possibly caused by inflammation or treatment and significant number may have abnormally high Prolactin reserve.[4] [5]
TSH, Prolactin, and IGF-1 are important sytemic factors in galactopoiesis. The significance of these factors in secretory disease is not well documented but it has been asserted that the mechanisms of secretory disease and galactopoiesis are closely related.
Alveolar and ductal epithelia permeability is mostly controlled by tight junction regulation and is closely linked to galactopoiesis and secretory disease. The tight junctions are regulated by a multitude of systemic (prolactin, progesterone, glucocorticoids) and local (intramammary pressure, TGF-beta, osmotic balance) factors.
Current smokers have the worst prognosis and highest rate of recurrent abscesses.[6]
Acromegaly may present with symptoms of non-puerperal mastitis.
Microscopic pathology
Histopathology of granulomatous mastitis shows characteristic distribution of granulomatous inflammation which remains the gold standard for diagnosis.[7]
Histologically, Lupus matitis is seen as lymphocytic lobular panniculitis and hyaline sclerosis of the adipose tissue. Treatment is primarily medical due to exacerbation of disease by surgical intervention. This histologic finding is required to make an accurate diagnosis.[8]
Terminology
Depending on appearance, symptoms, aetiological assumptions and histopathological findings a variety of terms has been used to describe mastitis and various related aspects.
- Galactopoiesis: means milk production
- Secretory disease: this refers to inappropriate secretory activity in the lobular and lactiferous duct system. This frequently leads to galactophoritis.
- Retention syndrome (retention mastitis): accumulation of secretions in the ducts with mainly intraductal inflammation.
- Galactostasis: like retention syndrome where the secret is known to be milk.
- Galactophoritis: inflammation of the lobular and lactiferous duct system, mainly resulting from secretory disease and retention syndrome.
- Plasma cell mastitis: plasma cells from the intraductal inflammation infiltrate surrounding tissue.
- Duct ectasia: this refers to widening of lactiferous ducts. It is relatively common finding in breast examinations and it increases with age. Strongly correlated with cyclic and very strongly with noncyclic breast pain.
- Duct ectasia syndrome: this was formerly used as synonym for nonpuerperal mastitis with recurring breast abscess, nipple discharge and possibly associated fibrocystic condition with blue dome cysts. Recent research shows that duct ectasia is only very weakly correlated with mastitis symptomes (inflammation, breast abscess).
- Squamous metaplasia of lactiferous ducts: This refers to cuboid cells in the epithelial lining of lactiferous ducts that transform (squamous metaplasia) to squamous epithelial cells. Can be seen in many cases of subareolar abscesses.
- Subareolar abscess: abscess bellow or in close vicinity of the areola. Mostly resulting from galactophoritis.
- Retroareolar abscess: deeper (closer to chest) than the lobular ductal system and thus deeper than a subareolar abscess.
- Periductal inflammation (periductal mastitis): infiltrative inflammation of the tissue surrounding lactiferous ducts. Almost synonym for subaerolar abscess.
- Fistula: is a tract draining an abscess cavity
- Zuska's disease: periareolar abscess associated with squamous metaplasia of lactiferous ducts. This may also have associated nipple discharge.
References
- ↑ Amir LH, Garland SM, Lumley J. (2006). "A case-control study of mastitis: nasal carriage of Staphylococcus aureus". BMC Family Practice. 7: 57. doi:10.1186/1471-2296-7-57.
- ↑ Amir LH, Garland SM, Lumley J. (2006). "A case-control study of mastitis: nasal carriage of Staphylococcus aureus". BMC Family Practice. 7: 57. doi:10.1186/1471-2296-7-57.
- ↑ Amir LH, Garland SM, Lumley J. (2006). "A case-control study of mastitis: nasal carriage of Staphylococcus aureus". BMC Family Practice. 7: 57. doi:10.1186/1471-2296-7-57.
- ↑ Peters F, Schuth W (1989). "Hyperprolactinemia and nonpuerperal mastitis (duct ectasia)". JAMA. 261 (11): 1618–20. PMID 2918655.
- ↑ Kutsuna S, Mezaki K, Nagamatsu M, Kunimatsu J, Yamamoto K, Fujiya Y; et al. (2015). "Two Cases of Granulomatous Mastitis Caused by Corynebacterium kroppenstedtii Infection in Nulliparous Young Women with Hyperprolactinemia". Intern Med. 54 (14): 1815–8. doi:10.2169/internalmedicine.54.4254. PMID 26179543.
- ↑ Risager R, Bentzon N (2010). "[Smoking and increased risk of mastitis]". Ugeskr Laeger. 172 (33): 2218–21. PMID 20727287.
- ↑ Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K (2010). "Granulomatous mastitis: clinical, pathological features, and management". Breast J. 16 (2): 176–82. doi:10.1111/j.1524-4741.2009.00879.x. PMID 20030652.
- ↑ Summers TA, Lehman MB, Barner R, Royer MC (2009). "Lupus mastitis: a clinicopathologic review and addition of a case". Adv Anat Pathol. 16 (1): 56–61. doi:10.1097/PAP.0b013e3181915ff7. PMID 19098467.