Polio pathophysiology
|
Polio Microchapters |
|
Causes |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Polio pathophysiology On the Web |
|
American Roentgen Ray Society Images of Polio pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The poliovirus is transmitted by the fecal-oral or oral route. Acute infection involves the oropharynx, gastrointestinal tract, and occasionally the central nervous system. Poliovirus divides within gastrointestinal cells for about one week before penetrating the intestinal lining. Once the virus enters the bloodstream it becomes a viremia and is widely-distributed throughout the body. Rarely, the major viremia progresses and the virus invades the central nervous system, causing a local inflammatory response.
Pathophysiology
| Outcome | Proportion of cases |
|---|---|
| Asymptomatic | 90–95% |
| Minor illness | 4–8% |
| Non-paralytic aseptic meningitis |
1–2% |
| Paralytic poliomyelitis | 0.1–0.5% |
| — Spinal polio | 79% of paralytic cases |
| — Bulbospinal polio | 19% of paralytic cases |
| — Bulbar polio | 2% of paralytic cases |
Pathogenesis

Poliovirus enters the body through the mouth, infecting the first cells it comes into contact with—follicular dendritic cells residing within the germinal centers of the tonsils and intestinal M cells-by binding to a immunoglobulin-like receptor known as the poliovirus receptor (CD155) on the cell surface. Once inside a human cell the virus hijacks the host cell's own machinery, and begins to replicate. Poliovirus divides within gastrointestinal cells for about one week before penetrating the intestinal lining. Following penetration, the virus is absorbed into the blood via the mesentery, and into the lymphatic system via the Peyer's patches.
Once the virus enters the bloodstream it becomes a viremia and is widely-distributed throughout the body. Poliovirus can survive and multiply within the blood and lymphatics for long periods of time, sometimes as long as 17 weeks. In a small percentage of cases the virus spreads and replicates in other sites such as brown fat, the reticuloendothelial tissues, and muscle. This sustained replication causes a secondary major viremia, and leads to the development of minor influenza-like symptoms.
Rarely, the major viremia progresses and the virus invades the central nervous system (CNS), causing a local inflammatory response. In most cases this causes a self limiting inflammation of the meninges, the layers of tissue surrounding the brain, causing non-paralytic aseptic meningitis. Penetration of the CNS provides no known benefit to the virus, and is quite possibly an "accidental" deviation of a normal gastrointestinal infection. The mechanisms by which poliovirus spreads to the CNS are poorly understood, but it appears to be primarily a chance event—largely independent of the age, gender, or socioeconomic position of the individual.
Paralytic Polio
In approximately 1% of infections poliovirus spreads along certain nerve fiber pathways, preferentially replicating in and destroying motor neurons within the spinal cord, brain stem, or motor cortex, which leads to the development of paralytic poliomyelitis. The various forms of paralytic poliomyelitis (spinal, bulbar, and bulbospinal) vary only with the amount of neuronal damage and inflammation that occurs, and the region of the CNS that is affected.
The destruction of neuronal cells produces lesions within the spinal ganglia; lesions can also be found in the reticular formation, vestibular nuclei, cerebellar vermis, and deep cerebellar nuclei. Inflammation associated with nerve cell destruction often alters the color and appearance of the gray matter in the spinal column, causing it to appear reddish and swollen. Other changes associated with paralytic disease occur in the hypothalamus and thalamus. The molecular mechanisms by which poliovirus causes paralytic disease are poorly understood.
Early symptoms of paralytic polio include a high fever, headache, stiffness in the back and neck, asymmetrical weakness of various muscles, sensitivity to touch, difficulty swallowing, muscle pain, loss of superficial and deep reflexes, paresthesia, irritability, constipation, or difficulty urinating. Paralysis generally develops 1 to 10 days after early symptoms begin, and progresses for 2 to 3 days. Paralysis is usually complete when the fever breaks.
The likelihood of developing paralytic polio and the extent of paralysis increase with age. In children non-paralytic meningitis is the most likely consequence of CNS involvement, and paralysis occurs in only 1 in 1000 cases. In adults paralysis occurs in 1 in 75 cases. In children under 5 years of age paralysis of one leg is most common, while in adults extensive paralysis in the trunk and muscles of the chest and abdomen and affecting all four limbs—quadriplegia—is more likely. Paralysis rates also vary depending on the serotype of the infecting poliovirus. The highest rates of paralysis (1 in 200) are associated with poliovirus type 1, the lowest rates (1 in 2,000) are associated with type 2.
Spinal Polio
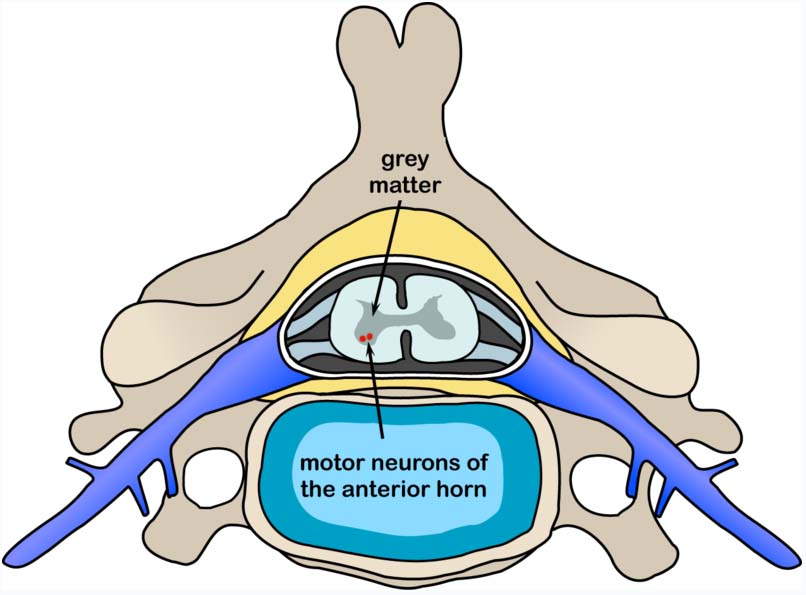
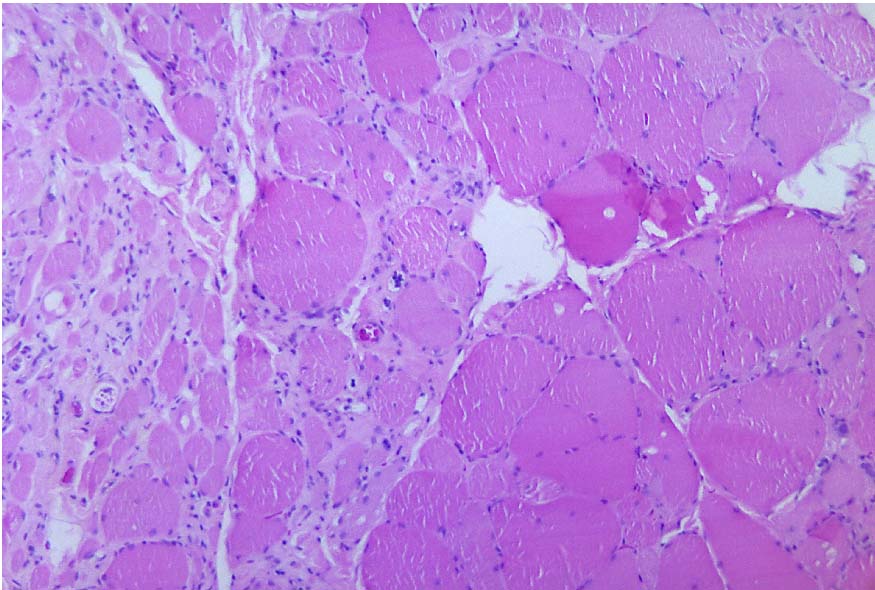
Spinal polio is the most common form of paralytic poliomyelitis; it results from viral invasion of the motor neurons of the anterior horn cells, or the ventral (front) gray matter section in the spinal column, which are responsible for movement of the muscles, including those of the trunk, limbs and the intercostal muscles.[1] Virus invasion causes inflammation of the nerve cells, leading to damage or destruction of motor neuron ganglia. When spinal neurons die, Wallerian degeneration takes place, leading to weakness of those muscles formerly innervated by the now dead neurons. With the destruction of nerve cells, the muscles no longer receive signals from the brain or spinal cord; without nerve stimulation, the muscles atrophy, becoming weak, floppy and poorly controlled, and finally completely paralyzed.[1] Progression to maximum paralysis is rapid (two to four days), and is usually associated with fever and muscle pain.[2] Deep tendon reflexes are also affected, and are usually absent or diminished; sensation (the ability to feel) in the paralyzed limbs, however, is not affected.
The extent of spinal paralysis depends on the region of the cord affected, which may be cervical, thoracic, or lumbar.[3] The virus may affect muscles on both sides of the body, but more often the paralysis is asymmetrical.[4] Any limb or combination of limbs may be affected—one leg, one arm, or both legs and both arms. Paralysis is often more severe proximally (where the limb joins the body) than distally (the fingertips and toes). [5]
Bulbar Polio
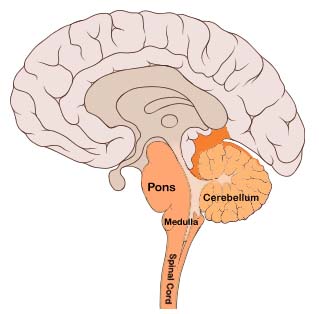
Comprising about 2% of cases of paralytic polio, bulbar polio occurs when poliovirus invades and destroys nerves within the bulbar region of the brain stem. The bulbar region is a white matter pathway that connects the cerebral cortex to the brain stem. The destruction of these nerves weakens the muscles supplied by the cranial nerves, producing symptoms of encephalitis, and causes difficulty breathing, speaking and swallowing. Critical nerves affected are the glossopharyngeal nerve, which partially controls swallowing and functions in the throat, tongue movement and taste; the vagus nerve, which sends signals to the heart, intestines, and lungs; and the accessory nerve, which controls upper neck movement. Due to the effect on swallowing, secretions of mucus may build up in the airway causing suffocation. [6] Other signs and symptoms include facial weakness, caused by destruction of the trigeminal nerve and facial nerve, which innervate the cheeks, tear ducts, gums, and muscles of the face, among other structures; double vision; difficulty in chewing; and abnormal respiratory rate, depth, and rhythm, which may lead to respiratory arrest. Pulmonary edema and shock are also possible, and may be fatal.
Bulbospinal Polio
Approximately 19% of all paralytic polio cases have both bulbar and spinal symptoms; this subtype is called respiratory polio or bulbospinal polio. Here the virus affects the upper part of the cervical spinal cord (C3 through C5), and paralysis of the diaphragm occurs. The critical nerves affected are the phrenic nerve, which drives the diaphragm to inflate the lungs, and those that drive the muscles needed for swallowing. By destroying these nerves this form of polio affects breathing, making it difficult or impossible for the patient to breathe without the support of a ventilator. It can lead to paralysis of the arms and legs and may also affect swallowing and heart functions.
Transmission
Poliomyelitis is highly contagious and spreads easily from human-to-human contact.[7] In endemic areas, wild polioviruses can infect virtually the entire human population.[8] It is seasonal in temperate climates, with peak transmission occurring in summer and autumn. These seasonal differences are far less pronounced in tropical areas. The time between first exposure and first symptoms, known as the incubation period, is usually 6 to 20 days, with a maximum range of 3 to 35 days.[9] Virus particles are excreted in the feces for several weeks following initial infection. The disease is transmitted primarily via the fecal-oral route, by ingesting contaminated food or water. It is occasionally transmitted via the oral-oral route,[10] a mode especially visible in areas with good sanitation and hygiene. Polio is most infectious between 7–10 days before and 7–10 days after the appearance of symptoms, but transmission is possible as long as the virus remains in the saliva or feces.
Factors that increase the risk of polio infection or affect the severity of the disease include immune deficiency,[11] malnutrition,[12] tonsillectomy,[13] physical activity immediately following the onset of paralysis,[14] skeletal muscle injury due to injection of vaccines or therapeutic agents,[15] and pregnancy.[16] Although the virus can cross the placenta during pregnancy, the fetus does not appear to be affected by either maternal infection or polio vaccination.[17] Maternal antibodies also cross the placenta, providing passive immunity that protects the infant from polio infection during the first few months of life.[18]
References
- ↑ 1.0 1.1 Frauenthal HWA, Manning JVV (1914). Manual of infantile paralysis, with modern methods of treatment. Philadelphia Davis. pp. 79–101. OCLC 2078290.
- ↑ Cono J, Alexander LN (2002). "Chapter 10, Poliomyelitis.". Vaccine Preventable Disease Surveillance Manual (PDF) (3rd ed. ed.). Centers for Disease Control and Prevention. pp. p. 10–1.
- ↑ Professional Guide to Diseases (Professional Guide Series). Hagerstown, MD: Lippincott Williams & Wilkins. 2005. pp. 243–5. ISBN 1-58255-370-X.
- ↑ Yin-Murphy M, Almond JW (1996). "Picornaviruses: The Enteroviruses: Polioviruses", Baron's Medical Microbiology (Baron S et al, eds.), 4th ed., Univ of Texas Medical Branch, e-text. ISBN 0-9631172-1-1
- ↑ Yin-Murphy M, Almond JW (1996). "Picornaviruses: The Enteroviruses: Polioviruses", Baron's Medical Microbiology (Baron S et al, eds.), 4th ed., Univ of Texas Medical Branch, e-text. ISBN 0-9631172-1-1
- ↑ Silverstein A, Silverstein V, Nunn LS (2001). Polio, Diseases and People. Berkeley Heights, NJ: Enslow Publishers, 12. ISBN 0-7660-1592-0.
- ↑ Kew O, Sutter R, de Gourville E, Dowdle W, Pallansch M (2005). "Vaccine-derived polioviruses and the endgame strategy for global polio eradication". Annu Rev Microbiol. 59: 587–635. PMID 16153180.
- ↑ Parker SP (ed.) (1998). McGraw-Hill Concise Encyclopedia of Science & Technology. New York: McGraw-Hill. p. 67. ISBN 0-07-052659-1.
- ↑ Racaniello V (2006). "One hundred years of poliovirus pathogenesis". Virology. 344 (1): 9–16. PMID 16364730.
- ↑ Ohri, Linda K. (1999). "Polio: Will We Soon Vanquish an Old Enemy?". Drug Benefit Trends. 11 (6): 41–54. Retrieved 2007-11-06. Unknown parameter
|coauthors=ignored (help) (Available free on Medscape; registration required.) - ↑ Davis L, Bodian D, Price D, Butler I, Vickers J (1977). "Chronic progressive poliomyelitis secondary to vaccination of an immunodeficient child". N Engl J Med. 297 (5): 241–5. PMID 195206.
- ↑ Chandra R (1975). "Reduced secretory antibody response to live attenuated measles and poliovirus vaccines in malnourished children". Br Med J. 2 (5971): 583–5. PMID 1131622.
- ↑ Miller A (1952). "Incidence of poliomyelitis; the effect of tonsillectomy and other operations on the nose and throat". Calif Med. 77 (1): 19–21. PMID 12978882.
- ↑ Horstmann D (1950). "Acute poliomyelitis relation of physical activity at the time of onset to the course of the disease". J Am Med Assoc. 142 (4): 236–41. PMID 15400610.
- ↑ Gromeier M, Wimmer E (1998). "Mechanism of injury-provoked poliomyelitis". J. Virol. 72 (6): 5056–60. PMID 9573275.
- ↑ Evans C (1960). "Factors influencing the occurrence of illness during naturally acquired poliomyelitis virus infections" (PDF). Bacteriol Rev. 24 (4): 341–52. PMID 13697553.
- ↑ Joint Committee on Vaccination and Immunisation (Salisbury A, Ramsay M, Noakes K (eds.) (2006). Chapter 26:Poliomyelitis. in: Immunisation Against Infectious Disease, 2006 (PDF). Edinburgh: Stationery Office. pp. 313–29. ISBN 0-11-322528-8.
- ↑ Sauerbrei A, Groh A, Bischoff A, Prager J, Wutzler P (2002). "Antibodies against vaccine-preventable diseases in pregnant women and their offspring in the eastern part of Germany". Med Microbiol Immunol. 190 (4): 167–72. PMID 12005329.