Pyelonephritis
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Pyelonephritis |
|
Articles |
|---|
|
Most recent articles on Pyelonephritis Most cited articles on Pyelonephritis |
|
Media |
|
Powerpoint slides on Pyelonephritis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pyelonephritis at Clinical Trials.gov Trial results on Pyelonephritis Clinical Trials on Pyelonephritis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pyelonephritis NICE Guidance on Pyelonephritis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pyelonephritis Discussion groups on Pyelonephritis Patient Handouts on Pyelonephritis Directions to Hospitals Treating Pyelonephritis Risk calculators and risk factors for Pyelonephritis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pyelonephritis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Pyelonephritis is an ascending urinary tract infection that has reached the pyelum (pelvis) of the kidney (nephros in Greek). If the infection is severe, the term "urosepsis" is used interchangeably (sepsis being a systemic inflammatory response syndrome due to infection). It requires antibiotics as therapy, and treatment of any underlying causes to prevent recurrence. It is a form of nephritis. It can also be called pyelitis.[1]. There are four different types of pyelonephritis:
- Acute Pyelonephritis
- Acute pyelonephritis is a common clinical diagnosis in patients who present with fever, chills, and flank tenderness.
- Infections typically result from ascending retrograde spread through the collecting ducts into the renal parenchyma.
- Patients are referred for CT evaluation of acute pyelonephritis when symptoms are poorly localized or complications are suspected.
- Chronic Pyelonephritis
- Chronic pyelonephritis is a somewhat controversial disease from a pathogenetic standpoint. It is unclear that, whether it is an active chronic infection, arises from multiple recurrent infections, or represents stable changes from a remote single infection.
- Hypertension is frequently a long-term sequela.
- Emphysematous Pyelonephritis
- Emphysematous pyelonephritis represents a severe life-threatening infection (overall mortality rate of approximately 50%) of the renal parenchyma with gas-forming bacteria.
- Underlying poorly controlled diabetes mellitus is present in up to 90% of patients who develop emphysematous pyelonephritis.
- Patients present clinically with varying degrees of renal failure, lethargy, acid-base irregularities, and hyperglycemia.
- E coli is the causative bacterial source in approximately 70% of cases
- Xanthogranulomatous Pyelonephritis
- Xanthogranulomatous pyelonephritis (XGP) is a rare inflammatory condition usually secondary to chronic obstruction caused by nephrolithiasis and resulting in infection and irreversible destruction of the renal parenchyma.
- XGP is associated with a staghorn calculus in approximately 70% of cases.
- Patients with diabetes are particularly predisposed to the formation of XGP.
- Treatment is nephrectomy.
- At histologic analysis, the inflammatory mass is composed of lipid-laden macrophages and chronic inflammatory cells.
Signs and symptoms
It presents with dysuria (painful voiding of urine), abdominal pain (radiating to the back on the affected side) and tenderness of the bladder area and the side of the involved kidney ("renal angle tenderness"). In many cases there are systemic symptoms in the form of fever, rigors (violent shivering while the termpature rises), headache and vomiting. In severe cases, delirium may be present.[1]
Diagnosis
The presence of nitrite and leukocytes (white blood cells) on a urine dipstick test in patients with typical symptoms are sufficient for the diagnosis of pyelonephritis, and are an indication for empirical treatment. Formal diagnosis is with culture of the urine; blood cultures may be needed if the source of the infection is initially doubtful.[1]
If a kidney stone is suspected (e.g. on the basis of characteristic colicky pain, disproportionate amount of blood in the urine), X-rays of the kidneys, ureters and bladder (KUB) may assist in identifying radioopaque stones.[1]
In patients with recurrent ascending urinary tract infections, it may be necessary to exclude an anatomical abnormality, such as vesicoureteral reflux (urine from the bladder flowing back into the ureter) or polycystic kidney disease. Investigations that are commonly used in this setting are ultrasound of the kidneys or voiding cystourethrography.[1]
Acute Pyelonephritis
Contrast Nephrograms
- Acute pyelonephritis consist of focal areas of striated or wedge-shaped hypoperfusion, resulting in a characteristic striated nephrogram.
- Striations result from stasis of contrast material within edematous tubules that demonstrates increasing attenuation over time.
- The infected kidney is usually enlarged, and there is often stranding in the perinephric fat.
- Delayed views of the infected kidney may demonstrate a nephrogram with increased attenuation.
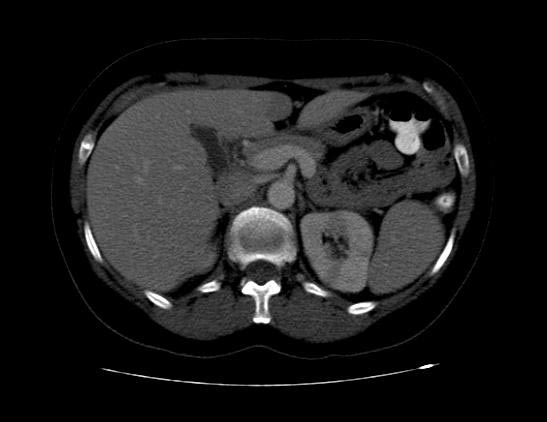
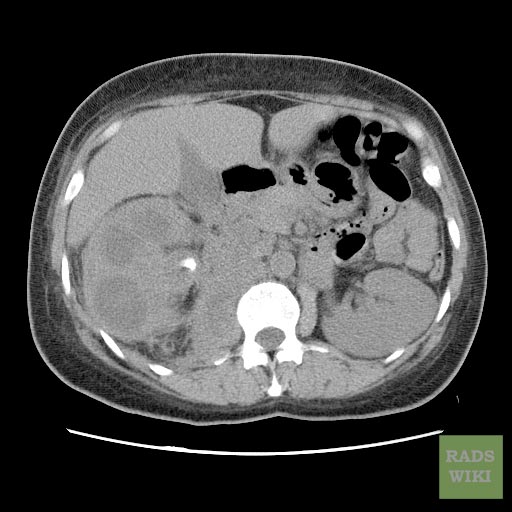
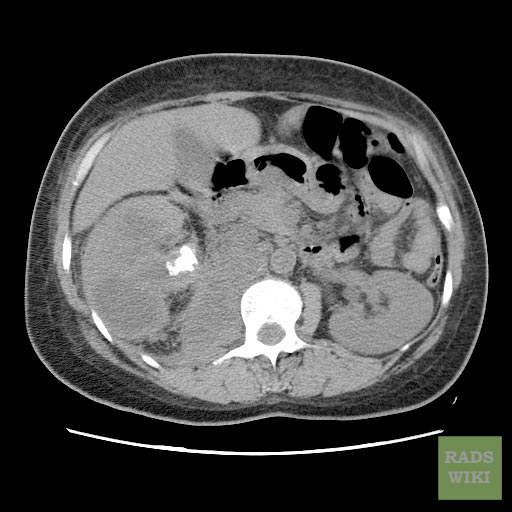
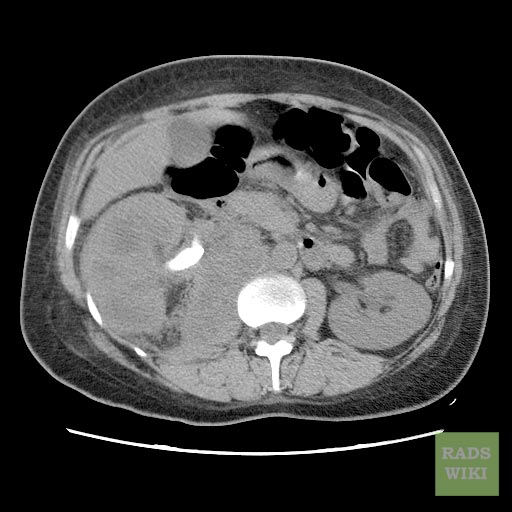
Computed Tomography
-
CT: Acute pyelonephritis
-
CT: Acute pyelonephritis
-
CT: Acute pyelonephritis
Chronic Pyelonephritis
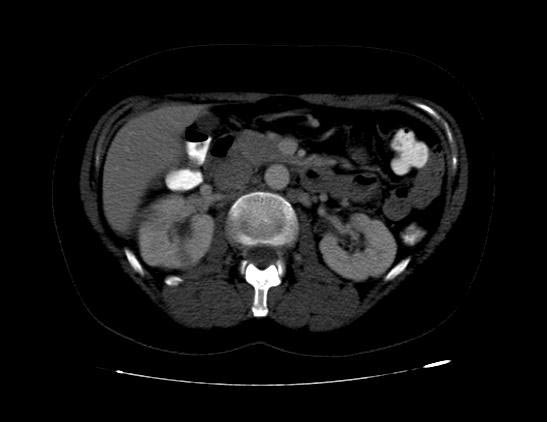
Computed Tomography
Imaging findings are characterized by renal scarring, atrophy and cortical thinning, hypertrophy of residual normal tissue, caliceal clubbing secondary to retraction of the papilla from overlying scar, thickening and dilatation of the caliceal system, and overall renal asymmetry.
(Images courtesy of RadsWiki)
-
CT image demonstrates chronic pyelonephritis on the right
-
CT image demonstrates chronic pyelonephritis on the right
-
CT image demonstrates chronic pyelonephritis on the right
Emphysematous Pyelonephritis
Plain film
- Conventional radiography may demonstrate gas bubbles overlying the renal fossa or may show a diffusely mottled kidney with radially oriented gas corresponding to the renal pyramids.
Ultrasonography
- US will characteristically show an enlarged kidney containing high-amplitude echoes within the renal parenchyma, often with low-level posterior dirty acoustic shadowing; however, the depth of parenchymal involvement may be underestimated at US, and multiple renal stones may also manifest as echogenic foci without "clean" posterior shadowing.
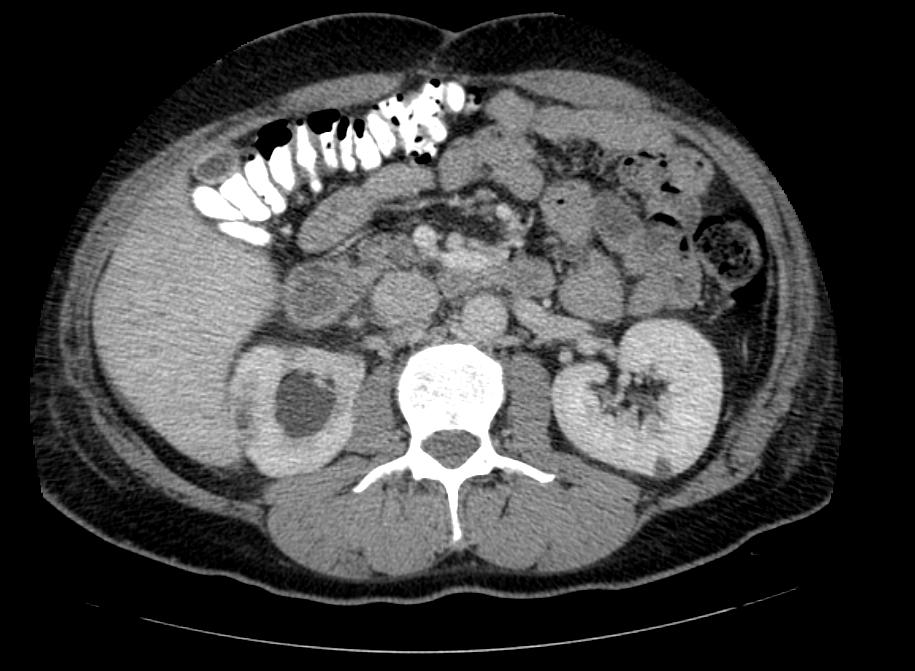
Computed Tomography
- Additional evaluation with CT will confirm the presence and extent of parenchymal gas and will often allow identification of the source of obstruction when present.
- The use of intravenous contrast material will often reveal asymmetric renal enhancement or delayed excretion, and, during the nephrographic phase, will help identify areas of focal tissue necrosis or abscess formation.
(Images courtesy of RadsWiki)
-
CT: Emphysematous pyelonephritis
-
CT: Emphysematous pyelonephritis
-
CT: Emphysematous pyelonephritis
Xanthogranulomatous Pyelonephritis
Urography
Classic urographic triad in diffuse xanthogranulomatous pyelonephritis consists of unilaterally decreased or (more commonly) absent renal excretion, a staghorn calculus, and a poorly defined mass or diffuse renal enlargement.
Ultrasonography
At sonography, the inflammatory mass itself is hypoechoic, with central echogenic foci corresponding to renal calculi.
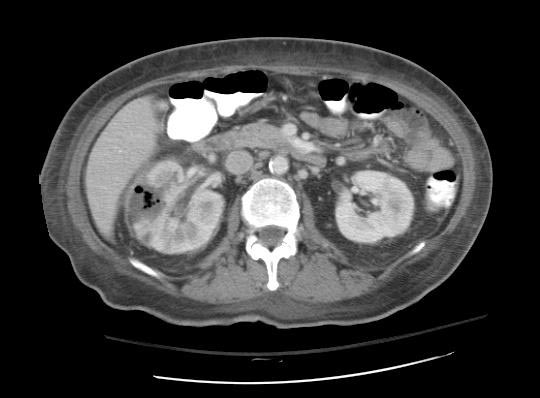
Computed Tomography
The CT findings of xanthogranulomatous pyelonephritis are pathognomonic in most cases: diffuse reniform enlargement with ill-defined central low attenuation, apparent cortical thinning, and central calculi.
- Extension into the perinephric space and beyond the Gerota fascia is not uncommon.
- Central areas of low attenuation represent nonenhancing xanthomatous material that may demonstrate attenuation values less than those of water.
(Images courtesy of RadsWiki)
-
CT image demonstrates right xanthogranulomatous pyelonephritis
-
CT image demonstrates right xanthogranulomatous pyelonephritis
-
CT image demonstrates right xanthogranulomatous pyelonephritis
Causes
Most cases of "community-acquired" pyelonephritis are due to bowel organisms that enter the urinary tract. Common organisms are E. coli (70-80%) and Enterococcus faecalis. Hospital-acquired infections may be due to coliforms and enterococci, as well as other organisms uncommon in the community (e.g. Klebsiella spp., Pseudomonas aeruginosa). Most cases of pyelonephritis start off as lower urinary tract infections, mainly cystitis and prostatitis.[1]
Risk is increased in the following situations:[1][2]
- Mechanical: any structural abnormalities to the kidneys and the urinary tract, calculi (kidney stones), urinary tract catheterisation, urinary tract stents or drainage procedures (e.g. nephrostomy), pregnancy, neuropathic bladder (e.g. due to spinal cord damage, spina bifida or multiple sclerosis) and prostate disease (e.g. benign prostatic hyperplasia) in men
- Constitutional: diabetes mellitus, immunocompromised states
- Behavioural: change in sexual partner within the last year, spermicide use
- Positive family history (close family members with frequent urinary tract infections)
Pathology
Acute pyelonephritis is an exudative purulent localized inflammation of the renal pelvis (collecting system) and kidney. The renal parenchyma presents in the interstitium abscesses (suppurative necrosis), consisting in purulent exudate (pus): neutrophils, fibrin, cell debris and central germ colonies (hematoxylinophils). Tubules are damaged by exudate and may contain neutrophil casts. In the early stages, glomeruli and vessels are normal.[4] Gross pathology often reveals pathognomonic radiations of hemorrhage and suppuration through the renal pelvis to the renal cortex. Chronic infections can result in fibrosis and scarring.
Acute pyelonephritis
<youtube v=aZ2il9a63J4/>
Chronic pyelonephritis
<youtube v=Q62z5EfzQjE/>
Treatment
As practically all cases of pyelonephritis are due to bacterial infections, antibiotics are the mainstay of treatment. Mild cases may be treated with oral therapy, but generally intravenous antibiotics are required for the initial stages of treatment. The type of antibiotic depends on local practice, and may include fluoroquinolones (e.g. ciprofloxacin), beta-lactam antibiotics (e.g. amoxicillin or a cephalosporin), trimethoprim (or co-trimoxazole) or nitrofurantoin. Aminoglycosides are avoided due to their toxicity, but may be added for a short duration.[1]
If the patient is unwell and septic, intravenous fluids may be administered to compensate for the reduced oral intake, insensible losses (due to the raised temperature) and vasodilation and to maximise urine output.
In recurrent infections, additional investigations may identify an underlying abnormality. Occasionally, surgical intervention is necessary to improve chances of recurrence. If no abnormality is identified, some studies suggest long-term preventative (prophylactic) treatment with antibiotics, either daily or after sexual intercourse.[3] In children at risk of recurrent UTIs, the evidence is inconclusive as to whether long-term prophylactic antibiotics are of use.[4] Ingestion of cranberry juice has been studied as a prophylactic measure; while studies are heterogeneous, many suggest a benefit.[5]
Epidemiology
Pyelonephritis is very common, with 12-13 cases annually per 10,000 population in women and 3-4 cases per 10,000 in men. Young women are most likely to be affected, traditionally reflecting sexual activity in that age group. Infants and the elderly are also at increased risk, reflecting anatomical abnormalities and hormonal status.[6]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Ramakrishnan K, Scheid DC (2005). "Diagnosis and management of acute pyelonephritis in adults". Am Fam Physician. 71 (5): 933–42. PMID 15768623.
- ↑ Scholes D, Hooton TM, Roberts PL, Gupta K, Stapleton AE, Stamm WE (2005). "Risk factors associated with acute pyelonephritis in healthy women". Ann. Intern. Med. 142 (1): 20–7. PMID 15630106.
- ↑ Schooff M, Hill K (2005). "Antibiotics for recurrent urinary tract infections". American family physician. 71 (7): 1301–2. PMID 15832532.
- ↑ Williams GJ, Wei L, Lee A, Craig JC (2006). "Long-term antibiotics for preventing recurrent urinary tract infection in children". Cochrane database of systematic reviews (Online). 3: CD001534. doi:10.1002/14651858.CD001534.pub2. PMID 16855971.
- ↑ Raz R, Chazan B, Dan M (2004). "Cranberry juice and urinary tract infection". Clin. Infect. Dis. 38 (10): 1413–9. doi:10.1086/386328. PMID 15156480.
- ↑ Czaja CA, Scholes D, Hooton TM, Stamm WE (2007). "Population-based epidemiologic analysis of acute pyelonephritis". Clin. Infect. Dis. 45 (3): 273–80. doi:10.1086/519268. PMID 17599303.
External links
- Template:GPnotebook
- Patient UK
- NKUDIC
- Goldminer: Xanthogranulomatous pyelonephritis
- Goldminer: Chronic pyelonephritis
- Goldminer: Emphysematous pyelonephritis
- Goldminer: Pyelonephritis
Additional Resources
- Bhatt, Shweta, MacLennan, Gregory, Dogra, Vikram. Renal Pseudotumors. Am. J. Roentgenol. 2007 188: 1380-1387.
- Perry J. Pickhardt, Gael J. Lonergan, Charles J. Davis, Jr, Naoko Kashitani, and Brent J. Wagner. From the Archives of the AFIP : Infiltrative Renal Lesions: Radiologic-Pathologic Correlation. RadioGraphics 2000 20: 215-243.
- William D. Craig, Brent J. Wagner, and Mark D. Travis. From the Archives of the AFIP: Pyelonephritis: Radiologic-Pathologic Review. RadioGraphics 2008 28: 255-276.
- David E. Grayson, Robert M. Abbott, Angela D. Levy, and Paul M. Sherman. Emphysematous Infections of the Abdomen and Pelvis: A Pictorial Review. RadioGraphics 2002 22: 543-561.
- Bruce A. Urban, and Elliot K. Fishman. Tailored Helical CT Evaluation of Acute Abdomen. RadioGraphics 2000 20: 725-749.
Template:Nephrology Template:SIB
de:Pyelonephritis
sv:Pyelonefrit